210867Orig1s000
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Bulletin Leading the Fight Against Heartworm Disease
BULLETIN LEADING THE FIGHT AGAINST HEARTWORM DISEASE SEPTEMBER HEARTWORM 2017 Q&A VOLUME 44 No. 3 Heartworm History: In What Year Was Heartworm First INSIDE THIS ISSUE Treated? Page 4 From the President Page 8 Research Update Abstracts from the Literature Page 14 Heartworm Hotline: Role of Heat Treatment in Diagnostics Page 19 NEW! Best Practices: Minimizing Heartworm Transmission in Relocated Dogs uestions from members, prac- published in the 1998 AHS Symposium 1 titioners, technicians, and the Proceedings. Dr. Roncalli wrote, “The Page 21 Qgeneral public are often submit- first trial to assess the efficacy of a Welcome Our New AHS ted to the American Heartworm Society microfilaricide (natrium antimonyl tar- Student Liaisons (AHS) via our website. Two of our AHS trate) was conducted some 70 years Board members, Dr. John W.McCall and ago (1927) in Japan by S. Itagaki and R. Page 25 Dr. Tom Nelson, provided the resources Makino.2 Fuadin (stibophen), a trivalent In the News: Surgeons to answer this question: In What Year antimony compound, was tested, intra- Remove a Heartworm from Was Heartworm First Treated? venously, as a microfilaricide by Popescu the Femoral Artery of a Cat The first efforts to treat canine heart- in 1933 in Romania and by W.H. Wright worm disease date back to the 1920s. Dr. and P.C. Underwood in 1934 in the USA. Page 26 Nelson referenced a review article by Dr. In 1949, I.C. Mark evaluated its use Quarterly Update Raffaele Roncalli, “Tracing the History of intraperitoneally.” What’s New From AHS? Heartworms: A 400 Year Perspective,” Continues on page 7 American Heartworm Society / PO Box 8266, Wilmington, DE 19803-8266 Become an American Heartworm Society www.heartwormsociety.org / [email protected] fan on Facebook! Follow us on Twitter! OUR GENEROUS SPONSORS PLATINUM LEVEL PO Box 8266 Wilmington, DE 19803-8266 [email protected] www.heartwormsociety.org Mission Statement The mission of the American Heartworm Society is to lead the vet- erinary profession and the public in the understanding of heartworm disease. -

Expert Review 2
2021 Expert Committee on Selection and Use of Essential Medicines Application review I.1 Albendazole, mebendazole and praziquantel for the indication of treatment of (item number) taeniid cestode cysts Does the application adequately ☒ Yes address the issue of the public health ☐ need for the medicine? No ☐ Not applicable Comments: The larval stages of three taeniid cestode parasites, Echinococcus granulosus, Echinococcus multilocularis and Taenia solium, produce cysts in humans that are of medical relevance. The diseases caused by these parasitic cysts are called cystic echinococcosis (CE), alveolar echinococcosis (AE), and cysticercosis (being neurocysticercosis (NCC) the most common form) respectively, and they are recognised by WHO as neglected tropical diseases. NCC is mainly a disease of poverty that predominantly affects rural populations in Africa, Asia and Latin America. Access to diagnostic and treatment, to better manage epilepsy and other NCC is a challenge for the people affected in these communities due to the availability and costs of specialised diagnostic and care. Stigma and social discrimination also mean that many people try to “hide” the disease. Briefly summarize the role of the The only real options for treatment of CE are albendazole (ALB) and Mebendazole proposed medicine(s) relative to other (MEB). ALB is the drug of choice as it has better bioavailability. ALB is also preferred to therapeutic agents currently included in MEB, because MEB requires a higher dose and a higher pill burden, for example, an the Model List, or available in the adult patient would require 8 tablets/day of MEB compared with 2 tablets/day ALB. market. ALB and praziquantel ( PZQ) are the only drugs used for the antiparasitic treatment of NCC. -
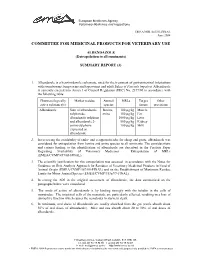
ALBENDAZOLE (Extrapolation to All Ruminants)
European Medicines Agency Veterinary Medicines and Inspections EMEA/MRL/865/03-FINAL June 2004 COMMITTEE FOR MEDICINAL PRODUCTS FOR VETERINARY USE ALBENDAZOLE (Extrapolation to all ruminants) SUMMARY REPORT (3) 1. Albendazole is a benzimidazole carbamate, used for the treatment of gastrointestinal infestations with roundworms, lungworms and tapeworms and adult flukes of Fasciola hepatica. Albendazole is currently entered into Annex I of Council Regulation (EEC) No. 2377/90 in accordance with the following table: Pharmacologically Marker residue Animal MRLs Target Other active substance(s) species tissues provisions Albendazole Sum of albendazole Bovine, 100 µg/kg Muscle sulphoxide, ovine 100 µg/kg Fat albendazole sulphone 1000 µg/kg Liver and albendazole 2- 500 µg/kg Kidney amino sulphone 100 µg/kg Milk expressed as albendazole 2. In reviewing the availability of endo- and ectoparasiticides for sheep and goats, albendazole was considered for extrapolation from bovine and ovine species to all ruminants. The considerations and criteria leading to the identification of albendazole are described in the Position Paper Regarding Availability of Veterinary Medicines – Extrapolation of MRLs (EMEA/CVMP/457/03-FINAL). 3. The scientific justification for this extrapolation was assessed in accordance with the Notes for Guidance on Risk Analysis Approach for Residues of Veterinary Medicinal Products in Food of Animal Origin (EMEA/CVMP/187/00-FINAL) and on the Establishment of Maximum Residue Limits for Minor Animal Species (EMEA/CVMP/153a/97-FINAL). 4. In setting the ADI in the original assessment of albendazole, the data summarised on the paragraphs below were considered. 5. The mode of action of albendazole is by binding strongly with the tubulin in the cells of nematodes. -

Efficacy and Tolerability of Quinacrine Monotherapy and Albendazole Plus Chloroquine Combination Therapy in Nitroimidazole-Refractory Giardiasis: a Tropnet Study
Klinik für Infektiologie & Spitalhygiene Efficacy and tolerability of quinacrine monotherapy and albendazole plus chloroquine combination therapy in nitroimidazole-refractory giardiasis: a TropNet study Andreas Neumayr, Mirjam Schunk, Caroline Theunissen, Marjan Van Esbroeck, Matthieu Mechain, Manuel Jesús Soriano Pérez, Kristine Mørch, Peter Sothmann, Esther Künzli, Camilla Rothe, Emmanuel Bottieau Journal Club 01.03.21 Andreas Neumayr Background on giardia treatment: • 1st-line treatment: 5-nitroimidazoles: metronidazole (1957), tinidazole, ornidazole, secnidazole • cure rate of 5NIs in 1st-line treatment: ~90% • in the last decade, an increase of 5NI-refractory giardia cases has been observed in travel medicine clinics across Europe: Hospital for Tropical Diseases, London: 2008: 15% --> 2013: 40% 70% of 5NI-refractory cases imported from India • 2nd-line treatment: effectiveness of a 2nd round with a 5NI: ~17% alternative drugs: albendazole, mebendazole, nitazoxanide, quinacrine, furazolidone, chloroquine, paromomycin 2012 TropNet member survey: 53 centres use 39 different treatment regimens, consisting of 7 different drugs in mono- or combination-therapy in various dosages and durations JC 01.03.21 Nabarro LE et al. Clin Microbiol Infect. 2015;21:791-6. • by 2013, there were only 13 reports of 2nd-line therapy for giardiasis (8 case series, 5 individual case reports): n=110 Cure rates Albendazole 6/32 18.7% Paromomycin 5/17 29.4% Nitazoxanide 2/5 40.0% Albendazole + 5-NI 42/53 79.2% Quinacrine 19/21 90.5% Quinacrine + 5-NI 14/14 100% Quinacrine + Paromomycin 2/2 100% • 2013: TropNet "GiardiaREF" study kick-off: Study on efficacy and tolerability of two 2nd-line regimens in nitroimidazole-refractory giardiasis: Quinacrine JC 01.03.21 Meltzer E et al. -
Computational Studies of Drug Repurposing Targeting P-Glycoprotein Mediated Multidrug-Resistance Phenotypes in Agents of Neglect
bioRxiv preprint doi: https://doi.org/10.1101/2020.06.12.147926; this version posted June 12, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. Computational studies of drug repurposing targeting P- glycoprotein mediated multidrug-resistance phenotypes in agents of neglected tropical diseases Nivedita Jaishankar 1, Sangeetha Muthamilselvan 2, Ashok Palaniappan 1,2* 1 Department of Biotechnology, Sri Venkateswara College of Engineering, Post Bag No. 1, Pennalur, Sriperumbudur Tk 602117. India 2 Department of Bioinformatics, School of Chemical and BioTechnology, SASTRA Deemed University, Thanjavur 613401. India * Corresponding author: [email protected] ABSTRACT Mammalian ABCB1 P-glycoprotein is an ATP- dependent efflux pump with broad substrate specificity associated with cellular drug resistance. Homologous to this role in mammalian biology, the P-glycoprotein of agents of neglected tropical diseases (NTDs) mediates the emergence of multidrug- resistance phenotypes. The clinical and socioeconomic implications of NTDs are exacerbated by the lack of research interest among Big Pharma for treating such conditions. This work aims to characterise P-gp homologues in certain agents of key NTDs, namely (1) Protozoa: Leishmania major, Trypanosoma cruzi; (2) Helminths: Onchocerca volvulus, Schistosoma mansoni. PSI-BLAST searches against the genome of each of these organisms confirmed the presence of P-gp homologues. Each homologue was aligned against five P- gp sequences of known structure, to identify the most suitable template based on sequence homology, phylogenetic nearest neighbor, and query coverage. -
Study Assessing Prices, Availability and Affordability of Children's
Study assessing prices, availability and affordability of children’s medicine in Chhattisgarh, India Part of the Better Medicine for Children project Authors Dr Antony KR Virendra Jain Puni Kokho Dr Kamlesh Jain The salient findings and views expressed in this report are solely those of the authors. Please direct correspondence to the authors: ([email protected], [email protected] [email protected], [email protected]). This publication does not necessarily represent the decisions or policies of the World Health Organization. ii Contents Acknowledgements ........................................................................................... v Abbreviations ................................................................................................... vi Executive summary ......................................................................................... vii Medicine availability .............................................................................................vii Medicine costs ................................................................................................... viii Affordability of standard treatment regimens ........................................................... ix Price components survey ...................................................................................... ix Conclusion .......................................................................................................... x 1. Introduction ................................................................................................. -

Veterinary Guide to Resistance & Parasites
Veterinary Guide to Resistance & Parasites How to make the Get Rotation Right deworming strategy part of your equine health wellness protocol. ||||||||||||||||||||||||||||||||||||||||| GET ROTATION RIGHT Resistant parasites – veterinary involvement is needed now. Deworming has come a long way in the past 50 years – from products that were nearly toxic and required complicated tubing to the easy-to-administer dewormers we know now. As more horse owners recognize the value of regular deworming, past troublemakers such as large strongyles have become much less of a threat. Still, deworming is nothing to take lightly. As internal parasites become more resistant, your expertise is needed Horseowners unknowingly more than ever to make sure deworming programs remain efficient contribute to resistance. and effective. Only with veterinary involvement will we control parasite • Rotating brand names, not populations, combat resistance and get rotation right. chemical classes – general confusion about when and RESISTANCE IS REAL: MULTIPLE DRUGS, MULTIPLE PARASITES. how to use different classes • No new drug class since avermectins in 1981. of dewormers. • Benzimidazole resistance in cyathostomes.1-3 • Lack of knowledge about • Pyrantel resistance in cyathostomes and ascarids.4-8,11 resistance issues. • Ivermectin and moxidectin resistance among ascarids.8,9,11 • Deworming many horses more • Early warning signs of macrocyclic-lactone-resistant cyathostomes.10 frequently than necessary. • Health-related issues caused by parasites: • Misunderstanding about the ~ Ascarids (roundworms) unique properties of larvicidal Verminous pneumonia: cough, nasal discharge, low-grade fever treatments and how to maximize Unthriftiness – rough hair coat their efficacy. Intestinal obstruction/colic • Underdosing their horses. Intestinal perforation leading to peracute death Decreased performance and reduced weight gain ~ Cyathostomes (small strongyles) Most common in young and old horses, but can afflict any horse. -

Valbazen ® (Albendazole)
® (albendazole oral suspension) Broad-Spectrum Dewormer Oral Suspension for Use in Cattle, Sheep, and Goats for removal and control of liver flukes, tapeworms, stomach worms (including 4th stage inhibited larvae of Ostertagia ostertagi), intestinal worms, and lungworms in cattle and sheep and for the treatment of adult liver flukes in nonlactating goats Active Ingredient Albendazole ............................. 11.36% (equivalent to 113.6 mg/mL) 1 L/33.8 fl oz (1 qt 1.8 fl oz) Approved by FDA under NADA # 110-048 40029175 ® (albendazole oral suspension) Broad-Spectrum Dewormer Oral Suspension for Use in Cattle, Sheep, and Goats for removal and control of liver Indications: flukes, tapeworms, stomach worms (including 4th stage inhibited larvae of Ostertagia Cattle and sheep: Valbazen is a broad-spectrum anthelmintic effective in the removal ostertagi), intestinal worms, and lungworms in cattle and sheep and for the treatment and control of liver flukes, tapeworms, stomach worms (including 4th stage inhibited of adult liver flukes in nonlactating goats larvae of Ostertagia ostertagi ), intestinal worms, and lungworms as indicated below. Active Ingredient: Goats: For the treatment of adult liver flukes in nonlactating goats. Albendazole .......................................................... 11.36% (Equivalent to 113.6 mg/mL) Parasite Cattle Sheep Goats Adult Liver Flukes Fasciola hepatica Fasciola hepatica, Fascioloides magna Fasciola hepatica Heads and Segments Moniezia benedeni, M. expansa Common Tapeworm (Moniezia expansa), Fringed Tapeworm of Tapeworms (Thysanosoma actinioides) Adult and 4th Stage Brown Stomach Worm, including 4th stage Brown Stomach Worm (Ostertagia circumcincta, Marshallagia Larvae of Stomach inhibited larvae (Ostertagia ostertagi), marshalli), Barber Pole Worm (Haemonchus contortus), Small Worms Barber Pole Worm (Haemonchus Stomach Worm (Trichostrongylus axei) contortus, H. -

Table of Contents Introduction
TABLE OF CONTENTS INTRODUCTION............................................................................................................. 2 DEFINITIONS .................................................................................................................. 2 ADVERSE EVENT REPORTING FOR ANIM AL DRUGS ....................................... 4 CANINE HEARTW ORM DISEASE.............................................................................. 7 M ACROCYCLIC LACTONES ...................................................................................... 8 PROHEART 6 PRODUCT INFORM ATION ............................................................... 8 REGULATORY HISTORY OF PROHEART 6 ......................................................... 10 ADE REPORTS FOR PROHEART 6 AND OTHER HEARTW ORM PREVENTIVES .............................................................................................................. 11 PROHEART 6 ADES ..................................................................................................... 16 TRENDS IN PROHEART 6 ADE REPORTING ....................................................... 19 CLINICAL M ANIFESTATIONS ................................................................................. 22 ANAPHYLAXIS/ANAPHYLACTOID REACTIONS ................................................................ 22 CONVULSIONS ................................................................................................................ 24 LIVER SIGNS.................................................................................................................. -

Albendazole: a Review of Anthelmintic Efficacy and Safety in Humans
S113 Albendazole: a review of anthelmintic efficacy and safety in humans J.HORTON* Therapeutics (Tropical Medicine), SmithKline Beecham International, Brentford, Middlesex, United Kingdom TW8 9BD This comprehensive review briefly describes the history and pharmacology of albendazole as an anthelminthic drug and presents detailed summaries of the efficacy and safety of albendazole’s use as an anthelminthic in humans. Cure rates and % egg reduction rates are presented from studies published through March 1998 both for the recommended single dose of 400 mg for hookworm (separately for Necator americanus and Ancylostoma duodenale when possible), Ascaris lumbricoides, Trichuris trichiura, and Enterobius vermicularis and, in separate tables, for doses other than a single dose of 400 mg. Overall cure rates are also presented separately for studies involving only children 2–15 years. Similar tables are also provided for the recommended dose of 400 mg per day for 3 days in Strongyloides stercoralis, Taenia spp. and Hymenolepis nana infections and separately for other dose regimens. The remarkable safety record involving more than several hundred million patient exposures over a 20 year period is also documented, both with data on adverse experiences occurring in clinical trials and with those in the published literature and\or spontaneously reported to the company. The incidence of side effects reported in the published literature is very low, with only gastrointestinal side effects occurring with an overall frequency of just "1%. Albendazole’s unique broad-spectrum activity is exemplified in the overall cure rates calculated from studies employing the recommended doses for hookworm (78% in 68 studies: 92% for A. duodenale in 23 studies and 75% for N. -

210867Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 210867Orig1s000 OTHER REVIEW(S) Clinical Inspection Summary (CIS) NDA 210867 (Moxidectin) Clinical Inspection Summary Date May 31, 2018 From John Lee, M.D., Medical Officer Janice Pohlman, M.D., M.P.H., Team Leader Kassa Ayalew, M.D., M.P.H., Branch Chief Good Clinical Practice Assessment Branch (GCPAB) Division of Clinical Compliance Evaluation (DCCE) Office of Scientific Investigations (OSI) To Kristine Park, Ph.D., Regulatory Project Manager Hiwot Hiruwy, M.D., Ph.D., Medical Officer Dmitri Iarikov, M.D., Ph.D., Clinical Team Leader Sumati Nambiar, M.D., M.P.H., Director Division of Anti-Infective Products (DAIP) Application NDA 210867 Applicant Medicines Development for Global Health (MDGH) Drug Moxidectin (trade name pending) NME Yes Review Status Priority Proposed Indication Treatment of ochocerciasis due to Onchocerca volvulus Consultation Date December 15, 2017 CIS Goal Date June 1, 2018 Action Goal Date June 13, 2018 PDUFA Due Date June 13, 2018 I. OVERALL ASSESSMENT OF FINDINGS Studies 3110A1-200-GH and 3110A1-3000-AF/ONCBL60801 were audited at good clinical practice (GCP) inspections of a clinical investigator (CI) and a contract research organization (CRO). For both inspections, the establishment inspection report (EIR) has not been received from the field office and the inspection outcome shown is based on preliminary communication with the field investigator. Both inspections revealed significant GCP deficiencies, typically (apparently) deficiencies in recordkeeping (Form FDA 483 issued at CI inspection, not issued at CRO inspection). Evidence of serious deficiencies indicative of unreliable study data was not observed and study conduct otherwise appeared GCP-compliant. -

Suramin Pharmacokinetics After Regional Or Systemic
TRANSLATIONAL RESEARCH IN CANCER: PRECLINICAL PHARMACODYNAMICS AND CANCER EPIDEMIOLOGY DISSERTATION Presented in Partial Fulfillment of the Requirements for the Degree Doctor of Philosophy in the Graduate School of The Ohio State University By Jia Ji, M.A.S. Graduate Program in Pharmacy The Ohio State University 2009 Dissertation Committee: Dr. Jessie L.-S. Au, Advisor Dr. M. Guillaume Wientjes Dr. Dennis B. McKay Copyright by Jia Ji 2009 ABSTRACT Translational research bridges preclinical and clinical research and shortens distance between these two areas in biomedical research. In preclinical study, our laboratory has found suramin sensitization at low and non-toxic dose and antagonism at toxic dose in multiple experimental models. The first part of this dissertation, Chapter 2 and 3, aims to evaluate cellular pharmacodynamics (PD) of biphasic effect of suramin and identify potential PD endpoint for future application in clinical practice. In Chapter 2, we first established an in vitro experimental model that illustrated suramin sensitization and antagonism to cisplatin, known as DNA-damaging drug. Addition of low dose suramin enhanced cellular response to cisplatin-induced DNA damage in three aspects, which are cell cycle arrest, cell death and senescence. Chapter 3 documented that persistence of γH2AX, a marker of DNA damage, was sustained by the addition of low dose suramin compared with cisplatin-alone treatment. No significant change of γH2AX kinetics was detected when suramin biphasic effect to taxanes, non-DNA-damaging drugs, was observed under both in vitro and in vivo settings. These preclinical discoveries not only lead us to treatment-dependant mechanism of suramin sensitization effect, but also indicate prospective clinical application of γH2AX as PD endpoint in anti-cancer therapy combined with suramin.