New Developments in Prokinetic Therapy for Gastric Motility Disorders
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Prokinetics and Ghrelin for the Management of Cancer Cachexia Syndrome
85 Review Article Prokinetics and ghrelin for the management of cancer cachexia syndrome Jimi S. Malik, Sriram Yennurajalingam Department of Palliative Care, Rehabilitation and Integrative Medicine, The University of Texas MD Anderson Cancer Center, Houston, TX, USA Contributions: (I) Conception and design: All authors; (II) Administrative support: S Yennurajalingam; (III) Provision of study materials or patients: S Yennurajalingam; (IV) Collection and assembly of data: All authors; (V) Data analysis and interpretation: All authors; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors. Correspondence to: Sriram Yennurajalingam, MD. Department of Palliative Care, Rehabilitation, and Integrative Medicine, The University of Texas MD Anderson Cancer Center, 1515 Holcombe Blvd., Unit 1414, Houston, TX 77030, USA. Email: [email protected]. Abstract: Cancer cachexia (CC) is one of the most distressing syndromes for both patients and their families. CC can have an impact on patient reported quality of life and overall survival. It is often associated with symptoms such as fatigue, depressed mood, early satiety, and anorexia. Prokinetic agents have been found to improve chronic nausea and early satiety associated with CC. Among the prokinetic agents, metoclopramide is one of the best studied medications. The role of the other prokinetic agents, such as domperidone, erythromycin, haloperidol, levosulpiride, tegaserod, cisapride, mosapride, renzapride, and prucalopride is unclear for use in cachectic cancer patients due to their side effect profile and limited efficacy studies in cancer patients. There has been an increased interest in the use of ghrelin-receptor agonists for the treatment of CC. Anamorelin HCl is a highly selective, novel ghrelin receptor agonist. -

International Journal of Medicine and Pharmaceutical Research
Wayal Sunil Anil et al, IJMPR, 2019, 7(6): 180-183 CODEN (USA): IJCPNH | ISSN: 2321-2624 International Journal of Medicine and Pharmaceutical Research Journal Home Page: www.pharmaresearchlibrary.com/ijmpr R E S E A R C H A R T I C L E Formulation and In-vitro Evaluation of Alosetron Oral Thin Films Wayal Sunil Anil1, G.S. Valluri2, Gampa Vijay Kumar3 Department of Pharmacy, KGR Institute of Technology and Management, Rampally, Kesara, Medchal, Telangana, India. A B S T R A C T Alosetron, is a 5-HT3 antagonist used for the management of severe diarrhea-predominant irritable bowel syndrome. In present study oral thin films of Alosetron were developed to have a faster on set of action. The oralthin films were developed by using polymers Guar gum, Pullulan and PVP K30.Oral thin films were prepared by employing solvent casting method. Propylene glycol was selected as permeation enhancer and plasticizer. Drug excipient compatibility studies were carried out by using FTIR, and it was observed that there were no interactions. Formulations were prepared with the varying concentrations polymers ranging from F1-F9, and all the formulations were evaluated for various physical parameters Physical appearance, Weight variation, Thickness, Folding endurance, Tensile strength, Drug content, Moisture uptake, Moisture content and all the results were found to be were found to be within the pharmacopeial limits, in-vitro drug release studies by using USP dissolution Apparatus Type II. Among all the 9 formulations F4 formulation which contain Pullulan 10mg and shown 97.06% cumulative drug release within 30 min. -

Comprehensive Pgx Report for 1 / 31 Examples of Different Levels of Evidence for Pgx Snps
Comprehensive PGx report for PERSONAL DETAILS Advanced Diagnostics Laboratory LLC CLIA:31D2149403 Phone: Fax: PATIENT DOB Address: 1030 North Kings Highway Suite 304 Cherry Hill, NJ 08034 GENDER FEMALE Website: http://advanceddiagnosticslaboratory.com/ SPECIMEN TYPE Oral Fluid LABORATORY INFORMATION ORDERING PHYSICIAN ACCESSION NUMBER 100344 FACILITY COLLECTION DATE 08/10/2020 RECEIVED DATE 08/14/2020 REPORT GENERATED 09/08/2020 LABORATORY DIRECTOR Dr. Jeanine Chiaffarano Current Patient Medication Clonidine (Catapres, Kapvay) The personalized pharmacogenomics profile of this patient reveals intermediate CYP2D6-mediated metabolism, extensive CYP1A2-mediated metabolism, and extensive CYP3A5-mediated metabolism. For further details, please find supporting evidence in this report or on websites such as www.pharmgkb.org or www.fda.gov. Losartan (Cozaar) The personalized pharmacogenomics profile of this patient reveals extensive CYP2C9-mediated metabolism, extensive CYP3A4-mediated metabolism, and extensive CYP3A5-mediated metabolism. For further details, please find supporting evidence in this report or on websites such as www.pharmgkb.org or www.fda.gov. Diltiazem (Cardizem, Tiazac) The personalized pharmacogenomics profile of this patient reveals extensive CYP3A4-mediated metabolism, intermediate CYP2C19-mediated metabolism, and extensive CYP3A5- mediated metabolism. For further details, please find supporting evidence in this report or on websites such as www.pharmgkb.org or www.fda.gov. Labetalol (Normodyne, Trandate) The personalized pharmacogenomics profile of this patient reveals intermediate CYP2D6-mediated metabolism, and intermediate CYP2C19-mediated metabolism. For further details, please find supporting evidence in this report or on websites such as www.pharmgkb.org or www.fda.gov. Mycophenolate mofetil (Myfortic, CellCept) The personalized pharmacogenomics profile of this patient reveals extensive CYP3A4-mediated metabolism, extensive CYP3A5-mediated metabolism, and extensive CYP2C8-mediated metabolism. -

Classification of Medicinal Drugs and Driving: Co-Ordination and Synthesis Report
Project No. TREN-05-FP6TR-S07.61320-518404-DRUID DRUID Driving under the Influence of Drugs, Alcohol and Medicines Integrated Project 1.6. Sustainable Development, Global Change and Ecosystem 1.6.2: Sustainable Surface Transport 6th Framework Programme Deliverable 4.4.1 Classification of medicinal drugs and driving: Co-ordination and synthesis report. Due date of deliverable: 21.07.2011 Actual submission date: 21.07.2011 Revision date: 21.07.2011 Start date of project: 15.10.2006 Duration: 48 months Organisation name of lead contractor for this deliverable: UVA Revision 0.0 Project co-funded by the European Commission within the Sixth Framework Programme (2002-2006) Dissemination Level PU Public PP Restricted to other programme participants (including the Commission x Services) RE Restricted to a group specified by the consortium (including the Commission Services) CO Confidential, only for members of the consortium (including the Commission Services) DRUID 6th Framework Programme Deliverable D.4.4.1 Classification of medicinal drugs and driving: Co-ordination and synthesis report. Page 1 of 243 Classification of medicinal drugs and driving: Co-ordination and synthesis report. Authors Trinidad Gómez-Talegón, Inmaculada Fierro, M. Carmen Del Río, F. Javier Álvarez (UVa, University of Valladolid, Spain) Partners - Silvia Ravera, Susana Monteiro, Han de Gier (RUGPha, University of Groningen, the Netherlands) - Gertrude Van der Linden, Sara-Ann Legrand, Kristof Pil, Alain Verstraete (UGent, Ghent University, Belgium) - Michel Mallaret, Charles Mercier-Guyon, Isabelle Mercier-Guyon (UGren, University of Grenoble, Centre Regional de Pharmacovigilance, France) - Katerina Touliou (CERT-HIT, Centre for Research and Technology Hellas, Greece) - Michael Hei βing (BASt, Bundesanstalt für Straßenwesen, Germany). -

Serotonin Receptors and Their Role in the Pathophysiology and Therapy of Irritable Bowel Syndrome
Tech Coloproctol DOI 10.1007/s10151-013-1106-8 REVIEW Serotonin receptors and their role in the pathophysiology and therapy of irritable bowel syndrome C. Stasi • M. Bellini • G. Bassotti • C. Blandizzi • S. Milani Received: 19 July 2013 / Accepted: 2 December 2013 Ó Springer-Verlag Italia 2013 Abstract Results Several lines of evidence indicate that 5-HT and Background Irritable bowel syndrome (IBS) is a functional its receptor subtypes are likely to have a central role in the disorder of the gastrointestinal tract characterized by pathophysiology of IBS. 5-HT released from enterochro- abdominal discomfort, pain and changes in bowel habits, maffin cells regulates sensory, motor and secretory func- often associated with psychological/psychiatric disorders. It tions of the digestive system through the interaction with has been suggested that the development of IBS may be different receptor subtypes. It has been suggested that pain related to the body’s response to stress, which is one of the signals originate in intrinsic primary afferent neurons and main factors that can modulate motility and visceral per- are transmitted by extrinsic primary afferent neurons. ception through the interaction between brain and gut (brain– Moreover, IBS is associated with abnormal activation of gut axis). The present review will examine and discuss the central stress circuits, which results in altered perception role of serotonin (5-hydroxytryptamine, 5-HT) receptor during visceral stimulation. subtypes in the pathophysiology and therapy of IBS. Conclusions Altered 5-HT signaling in the central ner- Methods Search of the literature published in English vous system and in the gut contributes to hypersensitivity using the PubMed database. -

Pharmacological Agents Currently in Clinical Trials for Disorders in Neurogastroenterology
Pharmacological agents currently in clinical trials for disorders in neurogastroenterology Michael Camilleri J Clin Invest. 2013;123(10):4111-4120. https://doi.org/10.1172/JCI70837. Clinical Review Esophageal, gastrointestinal, and colonic diseases resulting from disorders of the motor and sensory functions represent almost half the patients presenting to gastroenterologists. There have been significant advances in understanding the mechanisms of these disorders, through basic and translational research, and in targeting the receptors or mediators involved, through clinical trials involving biomarkers and patient responses. These advances have led to relief of patients’ symptoms and improved quality of life, although there are still significant unmet needs. This article reviews the pipeline of medications in development for esophageal sensorimotor disorders, gastroparesis, chronic diarrhea, chronic constipation (including opioid-induced constipation), and visceral pain. Find the latest version: https://jci.me/70837/pdf Review Pharmacological agents currently in clinical trials for disorders in neurogastroenterology Michael Camilleri Clinical Enteric Neuroscience Translational and Epidemiological Research (CENTER), Mayo Clinic, Rochester, Minnesota, USA. Esophageal, gastrointestinal, and colonic diseases resulting from disorders of the motor and sensory functions represent almost half the patients presenting to gastroenterologists. There have been significant advances in under- standing the mechanisms of these disorders, through basic and translational research, and in targeting the recep- tors or mediators involved, through clinical trials involving biomarkers and patient responses. These advances have led to relief of patients’ symptoms and improved quality of life, although there are still significant unmet needs. This article reviews the pipeline of medications in development for esophageal sensorimotor disorders, gastropa- resis, chronic diarrhea, chronic constipation (including opioid-induced constipation), and visceral pain. -

Classification Decisions Taken by the Harmonized System Committee from the 47Th to 60Th Sessions (2011
CLASSIFICATION DECISIONS TAKEN BY THE HARMONIZED SYSTEM COMMITTEE FROM THE 47TH TO 60TH SESSIONS (2011 - 2018) WORLD CUSTOMS ORGANIZATION Rue du Marché 30 B-1210 Brussels Belgium November 2011 Copyright © 2011 World Customs Organization. All rights reserved. Requests and inquiries concerning translation, reproduction and adaptation rights should be addressed to [email protected]. D/2011/0448/25 The following list contains the classification decisions (other than those subject to a reservation) taken by the Harmonized System Committee ( 47th Session – March 2011) on specific products, together with their related Harmonized System code numbers and, in certain cases, the classification rationale. Advice Parties seeking to import or export merchandise covered by a decision are advised to verify the implementation of the decision by the importing or exporting country, as the case may be. HS codes Classification No Product description Classification considered rationale 1. Preparation, in the form of a powder, consisting of 92 % sugar, 6 % 2106.90 GRIs 1 and 6 black currant powder, anticaking agent, citric acid and black currant flavouring, put up for retail sale in 32-gram sachets, intended to be consumed as a beverage after mixing with hot water. 2. Vanutide cridificar (INN List 100). 3002.20 3. Certain INN products. Chapters 28, 29 (See “INN List 101” at the end of this publication.) and 30 4. Certain INN products. Chapters 13, 29 (See “INN List 102” at the end of this publication.) and 30 5. Certain INN products. Chapters 28, 29, (See “INN List 103” at the end of this publication.) 30, 35 and 39 6. Re-classification of INN products. -

Gastroparesis - Recent Advances in the Pathophysiology and Treatment
ICDM 2015 Gastroparesis - Recent advances in the pathophysiology and treatment - Department of Internal Medicine, College of Medicine, St. Paul’s hospital, The Catholic University of Korea, Seoul, Korea Jung Hwan Oh 2015-10-16 Etiology . Idiopathic -- 40% . Diabetes mellitus -- 30% . Postsurgical (Gastrectomy/fundoplication) . Connective tissue disease . Hypothyroidism . Malignancy . Provocation drugs 2/46 . End-stage renal disease Number of people with diabetes (20-79 years), 2013 International Diabetes Federation: Diabetes Atlas 6th ed. 2013 3/46 Prevalence of DM in Korea % 15 11.9 10.1 10 8.6 5 0 2001 2010 2013 4/46 (>30 yo) Prevalence of GI symptoms in DM in Korea 15 % 13.2 11.2 10 8.2 7.1 5 N/V bloating dyspepsia heartburn 5/46 Oh JH, Choi MG et al. Korean J Intern Med 2009 Contents . Gastroparesis? . Prevalence . Recent advances in pathophysiology & treatment . Summary 6/46 What is gastroparesis? Delayed Absence of Symptoms gastric obstruction emptying 7/46 Classification . Mild gastroparesis . Moderate : Compensated gastroparesis – moderate symptoms with use of daily medications, maintain nutrition with dietary adjustments . Severe : Gastric failure – refractory symptoms that are not controlled, – inability to maintain oral nutrition Stanghellini V. Gut. 2014 8/46 Typical symptoms? . Nausea, vomiting . Abdominal discomfort . Early satiety . Postprandial fullness . Bloating 9/46 Gastroparesis: separate entity or just a part of FD? FD GP dus=bad gastro=stomach pa’ resis=incomplete paralysis pepto=digestion FD: Functional dyspepsia, GP: Gastroparesis Stanghellini V. Gut. 2014 Diagnosis . Scintigraphy . Wireless motility capsule (WMC) . Breath testing : 13C breath testing using otanoic acid, acetate or spirulina 11/46 Gastric Emptying Scintigraphy 20 Min 40 60 80 120 Delayed gastric emptying as greater than 60% retention at 2 hours and/or 10% at 4 hours 12/46 Consensus recommendations for gastric emptying scintigraphy . -

( 12 ) United States Patent
US010317418B2 (12 ) United States Patent ( 10 ) Patent No. : US 10 ,317 ,418 B2 Goosens (45 ) Date of Patent: * Jun . 11 , 2019 (54 ) USE OF GHRELIN OR FUNCTIONAL 7 , 479 ,271 B2 1 / 2009 Marquis et al . GHRELIN RECEPTOR AGONISTS TO 7 ,632 , 809 B2 12 / 2009 Chen 7 ,666 , 833 B2 2 /2010 Ghigo et al. PREVENT AND TREAT STRESS -SENSITIVE 7 , 901 ,679 B2 3 / 2011 Marquis et al . PSYCHIATRIC ILLNESS 8 ,013 , 015 B2 9 / 2011 Harran et al . 8 ,293 , 709 B2 10 /2012 Ross et al . (71 ) Applicant: Massachusetts Institute of 9 ,724 , 396 B2 * 8 / 2017 Goosens A61K 38 /27 9 , 821 ,042 B2 * 11 /2017 Goosens .. A61K 39/ 0005 Technology , Cambridge , MA (US ) 10 , 039 ,813 B2 8 / 2018 Goosens 2002/ 0187938 A1 12 / 2002 Deghenghi (72 ) Inventor : Ki Ann Goosens, Cambridge , MA (US ) 2003 / 0032636 Al 2 /2003 Cremers et al. 2004 / 0033948 Al 2 / 2004 Chen ( 73 ) Assignee : Massachusetts Institute of 2005 / 0070712 A1 3 /2005 Kosogof et al. Technology , Cambridge , MA (US ) 2005 / 0148515 Al 7/ 2005 Dong 2005 / 0187237 A1 8 / 2005 Distefano et al. 2005 /0191317 A1 9 / 2005 Bachmann et al. ( * ) Notice : Subject to any disclaimer , the term of this 2005 /0201938 A1 9 /2005 Bryant et al. patent is extended or adjusted under 35 2005 /0257279 AL 11 / 2005 Qian et al. U . S . C . 154 ( b ) by 0 days. 2006 / 0025344 Al 2 /2006 Lange et al. 2006 / 0025566 A 2 /2006 Hoveyda et al. This patent is subject to a terminal dis 2006 / 0293370 AL 12 / 2006 Saunders et al . -

CAS Number Index
2334 CAS Number Index CAS # Page Name CAS # Page Name CAS # Page Name 50-00-0 905 Formaldehyde 56-81-5 967 Glycerol 61-90-5 1135 Leucine 50-02-2 596 Dexamethasone 56-85-9 963 Glutamine 62-44-2 1640 Phenacetin 50-06-6 1654 Phenobarbital 57-00-1 514 Creatine 62-46-4 1166 α-Lipoic acid 50-11-3 1288 Metharbital 57-22-7 2229 Vincristine 62-53-3 131 Aniline 50-12-4 1245 Mephenytoin 57-24-9 1950 Strychnine 62-73-7 626 Dichlorvos 50-23-7 1017 Hydrocortisone 57-27-2 1428 Morphine 63-05-8 127 Androstenedione 50-24-8 1739 Prednisolone 57-41-0 1672 Phenytoin 63-25-2 335 Carbaryl 50-29-3 569 DDT 57-42-1 1239 Meperidine 63-75-2 142 Arecoline 50-33-9 1666 Phenylbutazone 57-43-2 108 Amobarbital 64-04-0 1648 Phenethylamine 50-34-0 1770 Propantheline bromide 57-44-3 191 Barbital 64-13-1 1308 p-Methoxyamphetamine 50-35-1 2054 Thalidomide 57-47-6 1683 Physostigmine 64-17-5 784 Ethanol 50-36-2 497 Cocaine 57-53-4 1249 Meprobamate 64-18-6 909 Formic acid 50-37-3 1197 Lysergic acid diethylamide 57-55-6 1782 Propylene glycol 64-77-7 2104 Tolbutamide 50-44-2 1253 6-Mercaptopurine 57-66-9 1751 Probenecid 64-86-8 506 Colchicine 50-47-5 589 Desipramine 57-74-9 398 Chlordane 65-23-6 1802 Pyridoxine 50-48-6 103 Amitriptyline 57-92-1 1947 Streptomycin 65-29-2 931 Gallamine 50-49-7 1053 Imipramine 57-94-3 2179 Tubocurarine chloride 65-45-2 1888 Salicylamide 50-52-2 2071 Thioridazine 57-96-5 1966 Sulfinpyrazone 65-49-6 98 p-Aminosalicylic acid 50-53-3 426 Chlorpromazine 58-00-4 138 Apomorphine 66-76-2 632 Dicumarol 50-55-5 1841 Reserpine 58-05-9 1136 Leucovorin 66-79-5 -
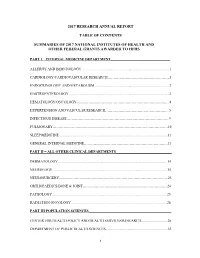
2017 Research Annual Report Table of Contents Summaries of 2017
2017 RESEARCH ANNUAL REPORT TABLE OF CONTENTS SUMMARIES OF 2017 NATIONAL INSTITUTES OF HEALTH AND OTHER FEDERAL GRANTS AWARDED TO HFHS PART I – INTERNAL MEDICINE DEPARTMENT_________________________________ ALLERGY AND IMMUNOLOGY ................................................................................................. 1 CARDIOLOGY/CARDIOVASCULAR RESEARCH…………………………………………….1 ENDOCRINOLOGY AND METABOLISM .................................................................................. 2 GASTROENTEROLOGY ............................................................................................................. .3 HEMATOLOGY/ONCOLOGY…………………………………………………………………...4 HYPERTENSION AND VASCULAR RESEARCH……………………………………………...5 INFECTIOUS DISEASE…………………………………………………………………………..9 PULMONARY……………………………………………………………………………………10 SLEEP MEDICINE ....................................................................................................................... 11 GENERAL INTERNAL MEDICINE…………………………………………………………….13 PART II – ALL OTHER CLINICAL DEPARTMENTS_______________________________ DERMATOLOGY ........................................................................................................................ 14 NEUROLOGY .............................................................................................................................. 15 NEUROSURGERY……………………………………………………………………………….23 ORTHOPAEDICS/BONE & JOINT……………………………………………………………..24 PATHOLOGY .............................................................................................................................. -

New Treatment Options for Chronic Constipation: Mechanisms, Efficacy and Safety
View metadata, citation and similar papers at core.ac.uk brought to you by CORE CHRONIC CONSTIPATION – CHALLENGES AND REMEDIES provided by Crossref New treatment options for chronic constipation: Mechanisms, efficacy and safety Michael Camilleri MD M Camilleri. New treatment options for chronic constipation: De nouvelles options thérapeutiques contre la Mechanisms, efficacy and safety. Can J Gastroenterol constipation chronique : leurs mécanismes, leur 2011;(Suppl B):29B-35B. efficacité et leur innocuité The present review has several objectives, the first of which is to review the pharmacology and selectivity of serotonergic agents to La présente analyse comporte plusieurs objectifs, le premier étant de contrast the older serotonergic agents (which were withdrawn because réviser la pharmacologie et la sélectivité des sérotoninergiques pour of cardiac or vascular adverse effects) with the newer generation sero- comparer les anciens sérotoninergiques (retirés du marché en raison de tonin receptor subtype 4 agonists. Second, the chloride ion secret- leurs effets cardiaques ou vasculaires) avec les agonistes de récepteurs agogues that act through the guanylate cyclase C receptor are appraised de la sérotonine de sous-type 4 de nouvelle génération. En deuxième and their pharmacology is compared with the approved medication, lieu, les sécrétagogues des ions chlorures qui agissent par le récepteur lubiprostone. Third, the efficacy and safety of the application of bile du guanylatecyclase C sont évalués, et leur pharmacologie est com- acid modulation to treat constipation are addressed. The long-term parée avec celle du lubiprostone, un médicament approuvé. En studies of surgically induced excess bile acid delivery to the colon are troisième lieu, l’efficacité et l’innocuité de l’application de la modula- reviewed to ascertain the safety of this therapeutic approach.