Patient Care Delivery
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
2017 Match Day Results by Program
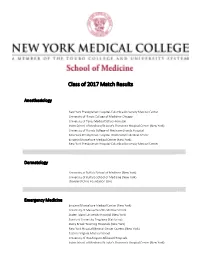
Class of 2017 Match Results Anesthesiology New York Presbyterian Hospital-Columbia University Medical Center University of Illinois College of Medicine-Chicago University of Texas Medical School-Houston Icahn School of Medicine/St Luke's-Roosevelt Hospital Center (New York) University of Florida College of Medicine-Shands Hospital New York Presbyterian Hospital-Weill Cornell Medical Center Einstein/Montefiore Medical Center (New York) New York Presbyterian Hospital-Columbia University Medical Center Dermatology University at Buffalo School of Medicine (New York) University of Buffalo School of Medicine (New York) Cleveland Clinic Foundation (OH) Emergency Medicine Einstein/Montefiore Medical Center (New York) University of Massachusetts Medical School Staten Island University Hospital (New York) Stanford University Programs (California) Stony Brook Teaching Hospitals (New York) New York Hospital Medical Center Queens (New York) Eastern Virginia Medical School University of Washington Affiliated Hospitals Icahn School of Medicine/St Luke's-Roosevelt Hospital Center (New York) University of Connecticut School of Medicine Rhode Island Hospital/Brown University Wake Forest Baptist Medical Center (North Carolina) Icahn School of Medicine/St Luke's-Roosevelt Hospital Center (New York) Einstein/Montefiore Medical Center (New York) Oregon Health and Science University Dartmouth-Hitchcock Medical Center (New Hampshire) Einstein/Montefiore Medical Center (New York) University of Washington Affiliated Hospitals Einstein/Montefiore Medical Center -

New York City Health and Hospitals Corporation New York City Health and Hospitals Corporation
NEW YORK CITY HEALTH AND HOSPITALS CORPORATION NEW YORK CITY HEALTH AND HOSPITALS CORPORATION Bronx Kings County Hospital Center Metropolitan Hospital Center Jacobi Medical Center 451 Clarkson Avenue 1901 First Avenue 1400 Pelham Parkway South Brooklyn, New York 11203 New York, New York 10029 Bronx, New York 10461 718-245-3131 212-423-6262 212-918-5000 Woodhull Medical and Mental Renaissance Health Care Lincoln Medical and Mental Health Center Network Diagnostic Health Center 760 Broadway & Treatment Center 234 East 149th Street Brooklyn, New York 11206 215 West 125th Street Bronx, New York 10451 718-963-8000 New York, New York 10027 718-579-5000 212-932-6500 Manhattan Morrisania Diagnostic Bellevue Hospital Center Queens & Treatment Center 462 First Avenue Elmhurst Hospital Center 1228 Gerard Avenue New York, New York 10016 79-01 Broadway Bronx, New York 10452 212-562-4141 Elmhurst, New York 11373 718-960-2777 Coler Goldwater Specialty 718-334-4000 North Central Bronx Hospital Hospital Queens Hospital Center 3424 Kossuth Avenue Roosevelt Island 82-70 164th Street Bronx, New York 10467 New York, New York 10044 Jamaica, New York 11432 718-519-5000 212-848-6000 718-883-3000 Segundo Ruiz Belvis Diagnostic Gouverneur Healthcare Services & Treatment Center 227 Madison Street Staten Island 545 East 142nd Street New York, New York 10002 Sea View Hospital Bronx, New York 10454 212-238-7000 Rehabilitation Center & Home 718-579-4000 460 Brielle Avenue Harlem Hospital Center Staten Island, New York 10314 506 Lenox Avenue Brooklyn 718-317-3000 New York, New York 10037 Coney Island Hospital 212-939-1000 2601 Ocean Parkway Brooklyn, New York 11235 718-616-30000 Cumberland Diagnostic & Treatment Center 100 North Portland Avenue Brooklyn, New York 11205 718-260-7500 Dr. -

Jacobi Medical Center
. June 10, 2015 Dear Manufacturers, I am writing on behalf of Jacobi Medical Center, 340B ID DSH330127, to inform manufacturers that Jacobi Medical Center recently underwent an audit by the Health Resources and Services Administration (HRSA) of Jacobi Medical Center’s compliance with 340B Drug Pricing Program (340B) requirements. As background, Jacobi Medical Center qualified for the 340B Program as a Disproportionate Share Hospital at 1400 Pelham Parkway South, Bronx, New York 10461 and has participated in the 340B Program since 1992. Through the audit process, Jacobi Medical Center was found to have non-compliance within their 340B Program and responsible for repayment as a result of the following findings: Jacobi Medical Center dispensed 340B drugs to ineligible providers, as prohibited by 42 USC 256b(a)(5)(B). The sample revealed that Jacobi’s contract pharmacies deemed two prescriptions 340B-eligible even though they should not have been eligible. The prescriptions were written by providers at ineligible sites (private offices which were not reimbursable on Jacobi’s Medicare cost report) without an arrangement demonstrating that responsibility of care provided remained at Jacobi. In addition, the auditor found that the 12 month eligibility period did not screen the patient-provider relationship or the patient referral process. It was also noted that the electronic medical record system did not update the billing software, thus allowing the third party pharmacy benefits manager to consider deactivated providers as eligible prescribers. Jacobi Medical Center reversed the 2 prescriptions from contract pharmacies that should not have been eligible, and removed the ineligible providers from Jacobi medical Center’s list of eligible providers. -

HOSPITAL SHARPS COLLECTION SITES in NEW YORK STATE As of July 11, 2016
HOSPITAL SHARPS COLLECTION SITES in NEW YORK STATE as of July 11, 2016 No. County Facility Name Address Phone Number Additional information about this site Albany Medical Center Hospital- 43 New Scotland Avenue Saturday 1 ALBANY 518-262-8700 E Building Basement Main Campus Albany, NY 12208 9:00 AM - 1:00 PM Albany Medical Center - South 25 HACKETT BLVD No public drop-off at this site. Drop off site is at Albany Med 2 ALBANY 518-262-1200 Clinical Campus Albany, NY 12208 Main Campus 600 Northern Blvd Albany, NY 12204 3 ALBANY Albany Memorial Hospital 518-471-3221 24/7 Laboratory The community sharps drop box is accessible 24 hrs a day 7 315 South Manning Blvd. 4 ALBANY St Peters Hospital 518-525-1163 24/7 days a week. The drop box is accessible if you park in the Albany, NY 12208 receiving dock and use the walkway to enter the hospital. Monday to Friday 140 West Main Street 5 ALLEGANY Cuba Memorial Hospital Inc 585-968-2000 8:00 AM - 4:00 PM Registration Area Cuba, NY 14727 191 N. Main Street Monday to Friday Memorial Hospital Jones Lobby, Emergency Department , Infection Prevention 6 ALLEGANY Box 72 585-593-1100 8:00 AM-5:00 PM Memorial Hospital Department or at each MD's Practice Andover, NY 14806 Monday to Friday Memorial Hospital Jones 15 Loder Street 9:00 AM - 12:00 PM 7 ALLEGANY 585-596-4101 Main Entrance Memorial Hospital Welsville, NY 14895 1:00 PM - 4:00 PM Monday to Friday 5877 Old State Route 19 Memorial Hospital Jones 9:00 AM - 12:00 PM 8 ALLEGANY Belmont, Wellsville 585-596-2051 Main Entrance Memorial Hospital 1:00 PM - 5:00 -

Directions to Jacobi Medical Center by SUBWAY AND
Directions to Jacobi Medical Center BY SUBWAY AND BUS: IRT EAST SIDE No. 5 Dyre Avenue train to E. 180th Street No. 2 White Plains Road/241st Street train to Pelham Parkway Any No.12 bus directly to Jacobi Medical Center (eastbound) IRT WEST SIDE No. 2 White Plains Road/241st Street train to Pelham Parkway Any No.12 bus directly to Jacobi Medical Center (eastbound) IND 6th AVENUE D train to Fordham Road (Grand Concourse) Any No.12 bus directly to Jacobi Medical Center (eastbound) AMBULATORY CARE PAVILION IRT EAST SIDE No. 5 Dyre Avenue train to E. 180th Street No. 21 bus (Morris Park Avenue) to Seminole Avenue IRT WEST SIDE No. 2 White Plains Road/241st Street train to E. 180th Street No. 21 bus (Morris Park Avenue) to Seminole Avenue BY CAR From Brooklyn: Brooklyn-Queens Expressway to Triborough Bridge to the Bronx. Bear right for the Bruckner Expressway. Follow signs for New Haven (I-95) on the Bruckner and get off at Bronx River Parkway exit. Take Bronx River Parkway north to Pelham Parkway exit. Follow Pelham Parkway east to Jacobi Medical Center, Main Gate. From Queens: Same as Brooklyn or Whitestone Bridge to Hutchinson River Parkway to Pelham Parkway West exit. Take Pelham Parkway west to Eastchester Road. Turn left at Eastchester Road to Morris Park Avenue. Turn right at Morris Park Avenue to Seminole Avenue. -OR- Throggs Neck Bridge to New England Thruway to Pelham Parkway West exit. From Manhattan: F.D.R. to Triborough Bridge to the Bronx bear right for the Bruckner Expressway. -

Residency Appointments 1981-2017
RESIDENCY APPOINTMENTS CLASS OF 1981 Harvey Finkelstein Robert Jacobson Anesthesiology OB-GYN Steven Abrams SUNY at Stony Brook, Mt. Sinai M. C., NY, NY Surgery Teaching Hosp., Stony Brook, Douglas Kahn Montefiore M. C., Bronx, NY NY Surgery Norman Back Barry Gach Buffalo General Hosp., OB-GYN Internal Medicine Buffalo, NY Maimonides M. C., Brooklyn, Washington Hosp. Ctr., Gary Maniloff NY Washington, D.C. Internal Medicine Andrea Bizar-Schneebaum Jay Gewolb Long Island Jewish Hosp., Internal Medicine Anesthesiology New Hyde Park, NY Waterbury Hosp., Waterbury, Yale New Haven Hosp., New Mark Melzer CT Haven, CT Pediatrics/Adolescent David Burton Benjamin Goldman Medicine Pediatrics Internal Medicine Montefiore M. C., Bronx, NY Northwestern University Cleveland Clinic Hosp., Michael Mogerman Children’s Memorial Hosp., Cleveland, OH Psychiatry Chicago, ILL Norman Heching Institute of Living Hosp., Lawrence Cytryn Internal Medicine Hartford, CT Internal Medicine Veterans Administration David Nierman Roosevelt Hosp., NY, NY Hosp., Hines, ILL Internal Medicine Marc Ehrenpreis Gerard Igel Long Island Jewish Hosp., Anesthesiology Pediatrics New Hyde Park, NY Long Island Jewish Hosp., Bronx Municipal Hosp. Ctr., Philip Orbuch New Hyde Park, NY Bronx, NY Dermatology David Ettinger Joseph Irrera NYU M. C., NY, NY Surgery Anesthesiology Dan Orron Buffalo General Hosp., Millard Fillmore Hosp., Radiology Buffalo, NY Buffalo, NY Beth Israel M. C., NY, NY Marc Palter Hallie Weiss Michael Dourmashkin Surgery Internal Medicine Urology Boston University Affiliated V.A. Hosp., NY, NY Montefiore M. C., Bronx, NY Hosp., Boston, MA Bruce Wenig Susan Drucker Lynne Quitell Pathology Pediatrics Pediatrics Mt. Sinai M. C., NY, NY University of MA M. C., Long Island Jewish Hosp., Worcester, MA Kenneth Werner New Hyde Park, NY Family Practice Gary Friedman Lonny Reisman St. -

Art of Caring Brochure:Layout 7.Qxd
Jacobi Medical Center Always the best of care. Now in the best of places. HHC - NYC Health & Hospitals Corporation (nyc.gov) A teaching hospital of the Albert Einstein College of Medicine Sutures, bandages and medicine are the tools that our physicians and caregivers use to restore the body. However, as physicians and caregivers we cannot ignore the power of the mind and the stimulating effect of art in the curative process. Our art...inspires the soul, which in turn heals and rejuvenates the body. Excerpt from The Medicine Of Art A Retrospective of Public Art in the New York City Health and Hospitals Corporation, 1977 For more information on the Art of Caring Campaign, please call 718.918.3827 or e-mail [email protected] Jacobi Medical Center Auxiliary, Inc. 1400 Pelham Parkway South Building 4, 7N5 Bronx, New York 10461 The Art of Caring he Art of Caring Campaign Suggested wording for recognition and dedicatory plaques affixed recognizes that medicine is an on individual pictures includes: Made Possible Through The Tart as much as a science; pays Generosity Of; Donated By; In Honor Of; In Recognition Of; In homage to an extraordinary array of Loving Memory Of; and, Dedicated To. caregivers whose interventions make the critical difference in both saving WAYS TO GET INVOLVED lives and optimizing recovery; and Jacobi Medical Center is supported by the Jacobi Medical Center acknowledges the power of the mind Auxiliary, Inc. a group of very special volunteers that helps to in the curative process, bringing art support and enhance the care provided at our hospital. -

Carrier Hospital Guide
2021 Carrier Hospital Guide EmblemHealth EmblemHealth EmblemHealth Oscar Oxford Oxford Hospital Name Healthfirst County Prime Select Care Millenium Circle Metro Liberty Albert Einstein College of Medicine √ √ √ √ √ Bronx BronxCare Health System √ √ √ √ Bronx Calvary Hospital √ √ √ √ Bronx Jacobi Medical Center √ √ √ √ √ Bronx Lincoln Medical & Mental Health Center √ √ √ √ √ Bronx Montefiore Medical Center √ √ √ √ Bronx Montefiore Westchester Square √ √ Bronx North Central Bronx Hospital √ √ √ √ √ Bronx St. Barnabas Hospital √ √ √ √ √ √ Bronx Total Hospitals in Bronx County 9 4 4 7 2 7 7 Midhudson Regional Hospital √ √ √ Dutchess Northern Dutchess Hospital √ √ √ √ Dutchess Vassar Brothers Medical Center √ √ √ √ Dutchess Total Hospitals in Dutchess County 3 2 0 0 0 3 3 Brookdale University Hospital Medical Center √ √ √ √ √ Kings Brooklyn Hospital Center √ √ √ √ √ √ √ Kings Coney Island Hospital Center √ √ √ √ √ Kings Interfaith Medical Center √ √ √ √ √ Kings Kings County Hospital Center √ √ √ √ √ Kings Kingsbrook Jewish Medical Center √ √ √ √ √ Kings Maimonides Medical Center √ √ √ Kings Mount Sinai Brooklyn √ √ √ √ √ √ √ Kings NYC Health + Hospitals √ √ √ √ √ Kings New York Community Hospital of Brooklyn √ √ √ √ Kings New York Presbyterian Methodist √ √ √ √ √ Kings NYU Lutheran Medical Center √ √ √ √ Kings SUNY Downstate Medical Center √ √ √ √ Kings Woodhull Medical and Mental Health Center √ √ √ √ √ Kings Wyckoff Heights Medical Center √ √ √ √ Kings Total Hospitals in Kings County 15 6 11 10 3 13 15 Cohen Children's Medical Center √ √ -

Dental Clinics – Bronx
DENTAL CLINICS – BRONX Listed below are dental clinics that offer low-cost dental services. If you or your child already has health insurance, please check with the plan to make sure that you or your child can get dental services through any of the clinics below. Please contact the organizations directly for information about services available for children and adults, hours of operation, appointments, health insurance accepted and any associated fees. 1) 161st Street Dental Clinic (Montefiore) 2) BronxCare Third Avenue Medical & Dental Practice* 305 E 161st St, Lower Level 2739-43 3rd Ave Bronx, NY 10451 Bronx, NY 10451 718-579-2535 or 888-700-6623 718-838-1022/1024 3) Lincoln Medical & Mental Health Center Department of 4) BronxCare Ogden Family Medical & Dental* Oral & Maxillofacial Surgery* 1067 Ogden Ave 234 E 149th St, Suite 2A8 Bronx, NY 10452 Bronx, NY 10451 718-466-3222 718 579-5690 5) Inwood Health Center (Bright Point Health)* 6) Morrisania Diagnostic and Treatment Center* 1543-1545 Inwood Ave 1225 Gerard Ave, 3rd Fl. Bronx, NY 10452 Bronx, NY 10452 855-681-8700 718-960-2777 7) BronxCare Dr. Martin Luther King, Jr. Health Center* 8) Morris Heights Health Center at Burnside* 1775 Grand Concourse 85 W Burnside Ave Bronx, NY 10453 Bronx, NY 10453 718-901-8400 718-716-4400 Ext. 2124 9) Morris Heights Health Center at Walton Avenue* 10) Union Community Health Center* 25 E 183rd St 2021 Grand Concourse Bronx, NY 10453 Bronx, NY 10453 718-716-4400 Ext. 8130 718 -960-3744 11) Walton Family Health Practice Dental Department 12) Morris Heights Health Center at 137th Street/ St. -

Directory of RWPA-Funded Care & Treatment Services
Directory of RWPA-funded Care & Treatment Services Bureau of HIV/AIDS Prevention & Control Care & Treatment Program Quality Management & Technical Assistance Spring 2019 1 Table of Contents Introduction .................................................................................................................................................. 5 New York City Services for People Living with HIV ....................................................................................... 6 Food & Nutrition Services ......................................................................................................................... 6 Bronx ..................................................................................................................................................... 6 Brooklyn ................................................................................................................................................ 7 Manhattan ............................................................................................................................................ 8 Queens ................................................................................................................................................ 11 Staten Island ....................................................................................................................................... 11 The Positive Life Workshop .................................................................................................................... -

Care Management Materials & Links
Care Management Materials & Links: Could It Be Early HIV? (DOH 9585) http://www.health.ny.gov/publications/958S.pdf HIV Case Management Standards & Forms (Not Printed) http://www.health.ny.gov/diseases/aids/providers/standards/casemanagement/cmstandards.htm Medicaid Health Homes & HIV Case Management Mother-to-Child Transmission (DOH 9685) http :1/www. health. ny .gov /publication s/9685. pdf Designated AIDS Centers Ending the Epidemic GET TESTED TREAT EARLY STAY SAFE END AIDS healt h.ny.gov/ete* Early/Acute Early HIV is the beginning stage of HIV disease, right after H IV infection occurs. If you were not aware that your partner is living with HIV, you did not realize you were at risk. During early HIV, the virus is reproducing very rapidly and HIV can be easily passed to others through sex or sharing injection equipment. Early HIV is sometimes called acute HIV infection. Signs and Symptoms of Acute/Early HIV • Sore throat • Swollen glands • Fever • Ra sh • Joint and muscle aches • Diarrhea • Tired feeling • Tonsillitis • Mouth sores The signs and symptoms of acute HIV infection can begin 2 to 4 weeks after you are infected with HIV. Symptoms can last for j ust a few days or weeks. In rare cases, they could last for several months. The signs and symptoms of early HIV infection are similar to the signs and symptoms of other common illnesses like the flu, cold, sore throat or mononucleosis. Is it the flu or Early/Acute HIV? The symptoms of early HIV and the flu are similar but not the same. -

The July 2017 Newsletter. We Hope You Enjoy!
Welcome to the July 2017 Newsletter. We hope you enjoy! Take a look at these resources from the PPS by simply clicking on the logo! Webinars Sa v e th e Da te fo r th e Up c o min g Cu ltu ra l Co mp e te n c y & He a lth L ite ra c y T ra in in g : "Instituting Agency Transformation for LGBTQ+ Inclusion: Understanding Disparities, Addressing Needs and Implementing Change." Free CME credits will be provided for eligible participants! NewYork-Presbyterian Hospital Vivian and Seymour Milstein Family Heart Center Riverview Terrace 173 Fort Washington Avenue New York, NY 10032 October 3, 2017 8:00am-1:00pm The NYP PPS aims to address institutional transformation for LGBTQ+ inclusion and needs. We will also provide an opportunity for networking, sharing resources, and showcasing the outstanding research and work being done regarding the LGBTQ+ community. Now accepting Poster Abstracts & Resource Table Requests! We are seeking submissions surrounding projects or resources that address structural and institutional inclusiveness, assessment or reduction of outcome disparities, or best practices in sexual orientation and gender identity data collection and analysis. Poster presentations may include examples of current LGBTQ+ inclusive practices, lessons learned, case studies, original research, or relevant literature/research reviews. Application Deadline: 5:00 p.m. (EST), August 15th, 2017 (Submissions will be reviewed on a rolling basis.) For additional information on Cultural Competency & Health Literacy efforts in the NYP PPS, please see our