Hyperthyroidism and Other Causes of Thyrotoxicosis: Management Guidelines of the American Thyroid Association and American Association of Clinical Endocrinologists
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Thyroid Hormone Misuse and Abuse
Endocrine (2019) 66:79–86 https://doi.org/10.1007/s12020-019-02045-1 REVIEW Thyroid hormone misuse and abuse Victor J. Bernet 1,2 Received: 11 June 2019 / Accepted: 2 August 2019 © Springer Science+Business Media, LLC, part of Springer Nature 2019 Abstract Thyroid hormone (TH) plays an essential role in human physiology and maintenance of appropriate levels is important for good health. Unfortunately, there are instances in which TH is misused or abused. Such misuse may be intentional such as when individuals take thyroid hormone for unapproved indications like stimulation of weight loss or improved energy. There are instances where healthcare providers prescribe thyroid hormone for controversial or out of date uses and sometimes in supraphysiologic doses. Othertimes, unintentional exposure may occur through supplements or food that unknowingly contain TH. No matter the reason, exposure to exogenous forms of TH places the public at risk for potential adverse side effects. Keywords Thyrotoxicosis ● Thyroid hormone abuse ● Thyroid hormone misuse ● Factitious thyrotoxicosis ● Supplements ● 1234567890();,: 1234567890();,: Analogs Overdose Thyroid hormone misuse and abuse secondary to exogenous TH ingestion that may be unin- tentional or purposeful such as in some cases of Munch- Almost any substance that impacts body physiology and ausen syndrome. Instances of TH misuse can be associated function is at risk for misuse or frank abuse, usually in the with the development of significant side effects. There are misgiven belief that the particular agent whether it be a other instances of chronic, low-grade over treatment with herb, supplement, medication, or hormone has healing TH, which occur for various misreasoning such as weight properties beyond that of which it actually possesses. -

Liothyronine Sodium(BANM, Rinnm) Potassium Perchlorate
2174 Thyroid and Antithyroid Drugs with methodological limitations. However, a controlled trial of In myxoedema coma liothyronine sodium may be liothyronine with paroxetine could not confirm any advantage of given intravenously in a dose of 5 to 20 micrograms by 3 O additive therapy. slow intravenous injection, repeated as necessary, usu- 1. Aronson R, et al. Triiodothyronine augmentation in the treat- HO I ally at intervals of 12 hours; the minimum interval be- ment of refractory depression: a meta-analysis. Arch Gen Psychi- OH atry 1996; 53: 842–8. tween doses is 4 hours. An alternative regimen advo- 2. Altshuler LL, et al. Does thyroid supplementation accelerate tri- NH2 cates an initial dose of 50 micrograms intravenously cyclic antidepressant response? A review and meta-analysis of I O the literature. Am J Psychiatry 2001; 158: 1617–22. followed by further injections of 25 micrograms every 3. Appelhof BC, et al. Triiodothyronine addition to paroxetine in I 8 hours until improvement occurs; the dosage may the treatment of major depressive disorder. J Clin Endocrinol then be reduced to 25 micrograms intravenously twice Metab 2004; 89: 6271–6. (liothyronine) daily. Obesity. Thyroid drugs have been tried in the treatment of obes- Liothyronine has also been given in the diagnosis of ity (p.2149) in euthyroid patients, but they produce only tempo- NOTE. The abbreviation T3 is often used for endogenous tri-io- hyperthyroidism in adults. Failure to suppress the up- rary weight loss, mainly of lean body-mass, and can produce se- dothyronine in medical and biochemical reports. Liotrix is USAN rious adverse effects, especially cardiac complications.1 for a mixture of liothyronine sodium with levothyroxine sodium. -

Salutary Lessons from TGA-Approved Sources for Thyroid-Related Medications
REVIEW Barriers in the quest for quality drug information: salutary lessons from TGA-approved sources for thyroid-related medications Jim R Stockigt n iodine-replete countries, about 5% of the population have a ABSTRACT thyroid disorder,1 of whom about a quarter will require long- • term medication either to correct deficiency or to control Product information (PI) for thyroid-related medications I endorsed by the Therapeutic Goods Administration, as thyroid hormone excess. In 2005, about 700 000 Pharmaceutical Benefits Scheme prescriptions were filled in Australia for thyrox- reproduced in the commonly used compilation publications ine, with about 80 000 scripts for the antithyroid drugs carbima- June 2006 MIMS (Monthly index of medical specialties) zole and propylthiouracil.2 annual, MIMS Online and the Australian prescription products Although no major new therapeutic agent has been introduced in guide 2006, was evaluated to see whether it reflects The Medical Journal of Australia ISSN: 0025- contemporary therapeutic practice. the thyroid729X 15 field January for 2007some 186 years, 2 76-79 the body of knowledge and • evidence©The has Medicaladvanced. Journal It is important of Australia that these 2007 developments are Compared with current medical literature, these PI-based reflectedwww.mja.com.au in the product information (PI) widely used by medical sources provide inadequate, inaccurate or outdated practitionersReview and a range of health professionals, who may not refer therapeutic directives. Examples include: directly to current scientific literature on thyroid disorders. MIMS ¾ Incorrect advice that thyroxine therapy should always 3 (Monthly index of medical specialties) annual, in its 30th edition in begin at very low dosage. -

A Case of Thyrotoxic Paralysis Caused by Consumption of Iodocaseine
Journal of Health and Social Sciences 2019; 4,2:277-282 CASE REPORT IN EMERGENCY MEDICINE A case of thyrotoxic paralysis caused by consumption of iodocaseine Antonio Villa1, Gabriella Nucera2 Affiliations: 1 M.D., Department of Emergency, ASST Monza, PO Desio, Monza, Italy 2 M.D., Department of Emergency Medicine, ASST Fatebenefratelli-Sacco, PO Fatebenefratelli, Milano, Italy Corresponding author: Dr Antonio Villa, ASST Monza, PO Desio. Via Fiuggi, 56 20159 Milan, Italy. E-mail: [email protected] Abstract Acute hypokalaemic paralysis is a rare but treatable cause of acute limb weakness. Thyrotoxic paralysis is an uncommon, potentially life-threatening endocrine emergency and it is a rare complication of hyperthyroidism. The most common causes of hyperthyroidism include Graves’ disease, multinodular goiters or solitary thyroid nodule, and iodine-induced thyrotoxicosis ( Jod-Basedow syndrome). Thyreotoxicosis factitia, which is caused by the excessive ingestion of exogenous thyroid hormone or iodine derivatives administration, has been rarely reported as a cause of thyrotoxic paralysis. We describe the case of a young Caucasian male with flaccid paralysis of all four limbs and severe hypokalaemia after inappropriate iodine derivatives (iodocasein) intake to show, in conclusion, how critical care physicians need to be aware of this rare but curable condition. KEY WORDS: Iodocaseine; hypokalaemia; thyrotoxic paralysis. 277 Journal of Health and Social Sciences 2019; 4,2:277-282 Riassunto La paralisi acuta ipokaliemica è una causa rara ma curabile di astenia acuta. La paralisi tireotossica è un'e- mergenza endocrina non comune e potenzialmente pericolosa per la vita ed è una rara complicanza dell'i- pertiroidismo. L'ipertiroidismo è causato prevalentemente dalla malattia di Graves, da gozzi singoli o multi- nodulari, e dalla malattia indotta da iodio ( Jod-Basedow). -

Survey of the Actual Administration of Thiamazole for Hyperthyroidism in Japan by the Japan Thyroid Association
doi:10.1507/endocrj.EJ21-0238 Original Survey of the actual administration of thiamazole for hyperthyroidism in Japan by the Japan Thyroid Association Natsuko Watanabe, Jaeduk Yoshimura Noh, Takashi Akamizu, Masanobu Yamada and the study group members of the Japan Thyroid Association The Japan Thyroid Association, Tokyo, Japan Abstract. To clarify the actual administration of thiamazole (MMI), the first choice of antithyroid drugs, the actual therapy provided by the Japan Thyroid Association (JTA) members for the following conditions was surveyed. The subjects included adult patients, pregnant women, and pediatric patients with Graves’ disease who visited each medical institution from September 2019 to February 2020. Initial doses, frequency of administration, maintenance doses, maximum doses, consultation intervals for pregnant women, and dosages administrated to breastfeeding mothers were surveyed. The total number of cases collected was 11,663. Administration of 15 mg once a day was the most common initial therapy, constituted 74.4% (2,526/3,397 cases) of adults, 33.8% (44/130) of pregnant women, and 50.8% (61/120) of children. The maintenance dose before discontinuation was equivalent to 2.5 mg/day in 52.3% (3,147/6,015). The most common maximum dose for adults and children was 30 mg/day, administrated to 57.5% of adults (223/388) and 59.6% (28/47) of children; for pregnant women, it was 15 mg/day, administrated to 71.1% (27/38). The most common consultation interval for pregnant women was every four weeks (32.1%, 341/1,063). In lactating mothers, the dose was 10 mg/day or less in 366 of 465 cases (78.7%). -

Resistance to Thyroid Hormone with a Mutation of the Thyroid B Receptor
Case report/opis przypadku Endokrynologia Polska DOI: 10.5603/EP.a2018.0082 Tom/Volume 70; Numer/Number 1/2019 ISSN 0423–104X Resistance to thyroid hormone with a mutation of the thyroid b receptor gene in an eight-month-old infant — a case report Zespół oporności na hormony tarczycy spowodowany mutacją w genie kodującym podjednostkę b receptora hormonów tarczycy u 8-miesięcznego niemowlęcia: opis przypadku Elżbieta Foryś-Dworniczak, Carla Moran, Barbara Kalina-Faska, Ewa Małecka-Tendera, Agnieszka Zachurzok Department of Paediatrics and Paediatric Endocrinology, School of Medicine in Katowice, Katowice, Poland Abstract Introduction: Resistance to thyroid hormone (RTHb) is a rare syndrome of impaired tissue responsiveness to thyroid hormones (THs). The disorder has an autosomal dominant or recessive pattern of inheritance. Most of the reported mutations have been detected in the thyroid hormone receptor b gene (THRB). Case report: Authors present an eight-month-old infant with poor linear growth, decreased body weight, tachycardia, positive family history, and neonatal features suggestive of RTHb. Both our patient and his mother had elevated free thyroxine, free triiodothyronine, and non-suppressed thyrotropin (TSH) concentration. The fluorescent sequencing analysis showed a heterozygous mutation c.728G>A in TRb gene. This pathogenic variant is known to be associated with THR. Conclusions: The clinical presentation of RTHb is variable, ranging from isolated biochemical abnormalities to symptoms of thyrotoxicosis or hypothyroidism. The -

EANM Practice Guideline/SNMMI Procedure Standard for RAIU and Thyroid Scintigraphy
European Journal of Nuclear Medicine and Molecular Imaging (2019) 46:2514–2525 https://doi.org/10.1007/s00259-019-04472-8 GUIDELINES EANM practice guideline/SNMMI procedure standard for RAIU and thyroid scintigraphy Luca Giovanella 1,2 & Anca M. Avram3 & Ioannis Iakovou4 & Jennifer Kwak5 & Susan A. Lawson3 & Elizabeth Lulaj6 & Markus Luster7 & Arnoldo Piccardo8 & Matthias Schmidt9 & Mark Tulchinsky10 & Frederick A. Verburg7 & Ely Wolin11 Received: 11 July 2019 /Accepted: 29 July 2019 / Published online: 7 August 2019 # Springer-Verlag GmbH Germany, part of Springer Nature 2019 Abstract Introduction Scintigraphic evaluation of the thyroid gland enables determination of the iodine-123 iodide or the 99mTc-pertechnetate uptake and distribution and remains the most accurate method for the diagnosis and quantification of thyroid autonomy and the detection of ectopic thyroid tissue. In addition, thyroid scintigraphy and radioiodine uptake test are useful to discriminate hyperthyroidism from destructive thyrotoxicosis and iodine-induced hyperthyroidism, respectively. Methods Several radiopharmaceuticals are available to help in differentiating benign from malignant cytologically indeterminate thyroid nodules and for supporting clinical decision-making. This joint practice guideline/procedure standard from the European Association of Nuclear Medicine (EANM) and the Society of Nuclear Medicine and Molecular Imaging (SNMMI) provides recommendations based on the available evidence in the literature. Conclusion The purpose of this practice guideline/procedure standard is to assist imaging specialists and clinicians in recommending, performing, and interpreting the results of thyroid scintigraphy (including positron emission tomography) with various radiopharmaceuticals and radioiodine uptake test in patients with different thyroid diseases. Keywords Thyroid . Scintigraphy . Radioiodine uptake test . 99mTc-sestaMIBI, 18F-fluorodeoxyglucose Preamble approval of the Committee on Guidelines and Board of Directors of both organizations. -

IRENAT 300 Mg/Ml, Solution Buvable En Gouttes
1. NAME OF THE MEDICINAL PRODUCT Irenat Drops 300 mg sodium perchlorate, oral drops Sodium perchlorate monohydrate 2. QUALITATIVE AND QUANTITATIVE COMPOSITION 1 ml solution (approximately 15 drops) contains 344.2 mg sodium perchlorate monohydrate (equivalent to 300 mg sodium perchlorate) For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Oral drops 4. CLINICAL PARTICULARS 4.1 Therapeutic indications For the treatment of hyperthyroidism, for thyroid blockade in the context of radionuclide studies of other organs using radioactively labelled iodine or of immunoscintigraphy to detect tumours using antibodies labelled with radioiodine. For the detection of a congenital iodine organification defect (perchlorate discharge test). 4.2 Posology and method of administration Posology Adults receive 4-5 x 10 Irenat drops daily (equivalent to 800-1000 mg sodium perchlorate) or, exceptionally, 5 x 15 Irenat drops daily (equivalent to 1500 mg sodium perchlorate) as an initial dose for the first 1-2 weeks. The mean maintenance dose is 4 x 5 Irenat drops (equivalent to 400 mg sodium perchlorate) per day. Children between the ages of 6 and 14 are treated throughout with a dose of 3-6 x 1 or 4-6 x 2 Irenat drops (equivalent to 60-240 mg sodium perchlorate) daily. When used for the perchlorate discharge test following administration of the dose of radioiodine tracer, a single dose is given of 30-50 Irenat drops (equivalent to 600-1000 mg sodium perchlorate) or 300 mg-600 mg/m 2 body surface area in children. As pretreatment for radionuclide studies not involving the thyroid itself and using radioactively labelled drugs or antibodies containing iodine or technetium, Irenat drops should be administered at doses of 10 – 20 drops (equivalent to 200-400 mg sodium perchlorate) and, in isolated cases, up to 50 drops (equivalent to 1000 mg sodium perchlorate) so as to reduce exposure of the thyroid to radiation and to block uptake of radionuclide into certain compartments. -

Neo-Mercazole
NEW ZEALAND DATA SHEET 1 NEO-MERCAZOLE Carbimazole 5mg tablet 2 QUALITATIVE AND QUANTITATIVE COMPOSITION Each tablet contains 5mg of carbimazole. Excipients with known effect: Sucrose Lactose For a full list of excipients see section 6.1 List of excipients. 3 PHARMACEUTICAL FORM A pale pink tablet, shallow bi-convex tablet with a white centrally located core, one face plain, with Neo 5 imprinted on the other. 4 CLINICAL PARTICULARS 4.1 Therapeutic indications Primary thyrotoxicosis, even in pregnancy. Secondary thyrotoxicosis - toxic nodular goitre. However, Neo-Mercazole really has three principal applications in the therapy of hyperthyroidism: 1. Definitive therapy - induction of a permanent remission. 2. Preparation for thyroidectomy. 3. Before and after radio-active iodine treatment. 4.2 Dose and method of administration Neo-Mercazole should only be administered if hyperthyroidism has been confirmed by laboratory tests. Adults Initial dosage It is customary to begin Neo-Mercazole therapy with a dosage that will fairly quickly control the thyrotoxicosis and render the patient euthyroid, and later to reduce this. The usual initial dosage for adults is 60 mg per day given in divided doses. Thus: Page 1 of 12 NEW ZEALAND DATA SHEET Mild cases 20 mg Daily in Moderate cases 40 mg divided Severe cases 40-60 mg dosage The initial dose should be titrated against thyroid function until the patient is euthyroid in order to reduce the risk of over-treatment and resultant hypothyroidism. Three factors determine the time that elapses before a response is apparent: (a) The quantity of hormone stored in the gland. (Exhaustion of these stores usually takes about a fortnight). -

Summary of Product Characteristics
Health Products Regulatory Authority Summary of Product Characteristics 1 NAME OF THE MEDICINAL PRODUCT Ultra-TechneKow FM 2.15-43.00 GBq radionuclide generator 2 QUALITATIVE AND QUANTITATIVE COMPOSITION Sodium pertechnetate (99mTc) injection is produced by means of a (99Mo/99mTc) generator. Technetium (99mTc) decays with the emission of gamma radiation with a mean energy of 140 keV and a half-life of 6.01 hours to technetium (99Tc) which, in view of its long half-life of 2.13 x 105 years can be regarded as quasi stable. The radionuclide generator containing the parent isotope 99Mo, adsorbed on a chromatographic column delivers sodium pertechnetate (99mTc) injection in sterile solution. The 99Mo on the column is in equilibrium with the formed daughter isotope 99mTc. The generators are supplied with the following 99Mo activity amounts at activity reference time which deliver the following technetium (99mTc) amounts, assuming a 100% theoretical elution yield and 24 hours time from previous elution and taking into account that branching ratio of 99Mo is about 87%: 99mTc activity (maximum theoretical elutable 1.90 3.81 5.71 7.62 9.53 11.43 15.24 19.05 22.86 26.67 30.48 38.10 GBq activity at ART, 06.00 h CET) 99Mo activity (at ART, 06.00 h 2.15 4.30 6.45 8.60 10.75 12.90 17.20 21.50 25.80 30.10 34.40 43.00 GBq CET) The technetium (99mTc) amounts available by a single elution depend on the real yields of the kind of generator used itself declared by manufacturer and approved by National Competent Authority. -
Hyperthyroidism and Thyrotoxicosis
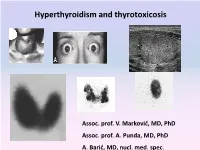
Hyperthyroidism and thyrotoxicosis Assoc. prof. V. Marković, MD, PhD Assoc. prof. A. Punda, MD, PhD A. Barić, MD, nucl. med. spec. Hyperthyroidism- Thyrotoxicosis Hyperthyroidism- elevated serum levels of thyroid hormones caused by overproduction of thyroid hormones Thyrotoxicosis: elevated serum level of thyroid hormones/ excessive amount of circulating thyroid hormone Hyperthyreoidism includes thyreotoxycosis but Thyrotoxicosis is not exclusively caused by hyperthyroidism Classification of thyrotoxicosis Hyperthyroidism Thyrotoxicosis without hyperthyroidism Mb Basedow-Graves Thyrotoxicosis factitia Multinodular toxic goiter Subacute thyroiditis (painfull) Toxic adenoma Subacute thyroiditis (painless) Elevated TSH levels Ectopic thyroid tissue Trophoblastic tumors Iod-Basedow Diffuse toxic goiter (Mb Basedow, Graves) Diffuse toxic goiter Mb. Graves-Basedow Epidemiology and etiology Diffuse toxic goiter (Mb. Graves- Basedow) is an autoimune, multysistemic dissease, wich includes the thyoid gland, infiltrative ophthalmopathy, dermopathy and acropathy. World wide prevalence is about 0,4-2% in women, 0,1% in men, includes 60-90% of hyperthyroidism cases*. It is complex disease with predominant genetic component.& Sex hormones, stress. Disease is caused by TSH receptor stimulating antibodies/ TSH stimulating antibodies (TSAb), in 80-100% patients. *Taunbridge WMG, Vanderpump MPJ. Population screening for autoimmune thyroid disease. Endocriol Metab Clin North Am. 2000;29:239-253. &Brix TH, Kyvik KO, Christensen K, et al. Evdence for a major -

Thyroid Crisis Following Interstitial Nephritis
□ CASE REPORT □ Thyroid Crisis following Interstitial Nephritis Toshio Kahara 1, Miyako Yoshizawa 1, Izaya Nakaya 1, Akio Uchiyama 2,AtsuoMiwa2, Yasunori Iwata 1, Muneyoshi Torita 1, Rika Usuda 1 and Hiroyuki Iida 1 Abstract A 54-year-old man with Graves’ disease had been treated with thiamazole (5 mg/day). His thyroid hor- mone level was increased after exodontia in February 2006. Although his prescribed dose of thiamazole was increased after exodontia on the fourth day, he developed thyroid crisis on exodontia 52nd day. Laboratory findings also showed renal dysfunction (from Cr 1.0 mg/dL in July 2005 to Cr 1.8 mg/dL on exodontia 37th day). His thyroid hormone level was normalized after subtotal thyroidectomy; however, serum Cr level was still high. He was diagnosed with interstitial nephritis as a result of renal biopsy, and he was treated with prednisolone 30 mg/day. This present case developed thyroid crisis even though the quantity of thiamazole was increased after exodontia. It seems that interstitial nephritis, as well as exodontia, is an aggravation fac- tor of thyroid function. After a poor response to anti-thyroid drugs, it is necessary to prevent thyroid crisis by determining the aggravating factor and to then provide appropriate treatment. Key words: interstitial nephritis, thyroid crisis, hyperthyroidism, Graves’ disease (Inter Med 47: 1237-1240, 2008) (DOI: 10.2169/internalmedicine.47.0947) 4.7% are due to tubulointerstitial nephritis and uveitis syn- Introduction drome (TINU) (2). There are case reports of transient hyper- thyroidism in TINU (3, 4), and interstitial nephritis may Thyroid crisis is defined as thyroid function that is ex- contribute to aggravation of the thyroid function.