Phototherapy with PUVA: Versatility and Efficacy in Dermatoses
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Mutagenesis by 8-Methoxypsoralen and 5-Methylangelicin Photoadducts in Mouse Fibroblasts: Mutations at Cross-Linkable Sites Indu
[CANCER RESEARCH 55, 1283-1288, March 15, 1995] Mutagenesis by 8-Methoxypsoralen and 5-Methylangelicin Photoadducts in Mouse Fibroblasts: Mutations at Cross-Linkable Sites Induced by Monoadducts as well as Cross-Links1 Edward J. Günther,Toni M. Yeasky, Francis P. Gasparro, and Peter M. Glazer2 Departments of Therapeutic Radiology ¡E.J. G., T. M. Y.. P. M. G.] and Dermatology ¡F.P. G.I, Yale University School of Medicine, New Haven, Connecticut 06520-8040 ABSTRACT center PUVA trial, Stem et al. (4) showed a statistically significant increase in the incidence of squamous cell carcinoma in PUVA Psoralens are used clinically in the treatment of several skin diseases, patients. A comparative analysis of the incidence of squamous cell including psoriasis, vitÃligo,and cutaneous T cell lymphoma. However, psoralen treatment has been associated with an increased risk of squa- carcinoma in the U.S. and European trials was recently reported (5). nious cell carcinoma of the skin. To elucidate molecular events that may While in earlier comparisons there appeared to be differences between play a role in the psoralen-related carcinogenesis, we examined psoralen- the European and American experience with PUVA-induced inci induced mutagenesis in a mouse fibroblast cell line carrying a recoverable, dence of squamous cell carcinoma, the ongoing periodic reanalysis of chromosomally integrated A phage shuttle vector. Using the stipi- gene as each set of data with a longer follow-up period now indicates com a mutation reporter gene, we determined the spectrum of mutations parable findings. induced by photoactivation of 8-methoxypsoralen and of 5-methylangeli- It is likely that these cancers arise from the mutagenic psoralen cin. -
Update on Challenging Disorders of Pigmentation in Skin of Color Heather Woolery-Lloyd, M.D
Update on Challenging Disorders of Pigmentation in Skin of Color Heather Woolery-Lloyd, M.D. Director of Ethnic Skin Care Voluntary Assistant Professor Miller/University of Miami School of Medicine Department of Dermatology and Cutaneous Surgery What Determines Skin Color? What Determines Skin Color? No significant difference in the number of melanocytes between the races 2000 epidermal melanocytes/mm2 on head and forearm 1000 epidermal melanocytes/mm2 on the rest of the body differences present at birth Jimbow K, Quevedo WC, Prota G, Fitzpatrick TB (1999) Biology of melanocytes. In I. M. Freedberg, A.Z. Eisen, K. Wolff,K.F. Austen, L.A. Goldsmith, S. I. Katz, T. B. Fitzpatrick (Eds.), Dermatology in General Medicine 5th ed., pp192-220, New York, NY: McGraw Hill Melanosomes in Black and White Skin Black White Szabo G, Gerald AB, Pathak MA, Fitzpatrick TB. Nature1969;222:1081-1082 Jimbow K, Quevedo WC, Prota G, Fitzpatrick TB (1999) Biology of melanocytes. In I. M. Freedberg, A.Z. Eisen, K. Wolff, K.F. Austen, L.A. Goldsmith, S. I. Katz, T. B. Fitzpatrick (Eds.), Dermatology in General Medicine 5th ed., pp192- 220, New York, NY: McGraw Hill Role of Melanin-Advantages Melanin absorbs and scatters energy from UV and visible light to protect epidermal cells from UV damage Disadvantages Inflammation or injury to the skin is almost immediately accompanied by alteration in pigmentation Hyperpigmentation Hypopigmentation Dyschromias Post-Inflammatory hyperpigmentation Acne Melasma Lichen Planus Pigmentosus Progressive Macular Hypomelanosis -

Pityriasis Alba Revisited: Perspectives on an Enigmatic Disorder of Childhood
Pediatric ddermatologyermatology Series Editor: Camila K. Janniger, MD Pityriasis Alba Revisited: Perspectives on an Enigmatic Disorder of Childhood Yuri T. Jadotte, MD; Camila K. Janniger, MD Pityriasis alba (PA) is a localized hypopigmented 80 years ago.2 Mainly seen in the pediatric popula- disorder of childhood with many existing clinical tion, it primarily affects the head and neck region, variants. It is more often detected in individuals with the face being the most commonly involved with a darker complexion but may occur in indi- site.1-3 Pityriasis alba is present in individuals with viduals of all skin types. Atopy, xerosis, and min- all skin types, though it is more noticeable in those with eral deficiencies are potential risk factors. Sun a darker complexion.1,3 This condition also is known exposure exacerbates the contrast between nor- as furfuraceous impetigo, erythema streptogenes, mal and lesional skin, making lesions more visible and pityriasis streptogenes.1 The term pityriasis alba and patients more likely to seek medical atten- remains accurate and appropriate given the etiologic tion. Poor cutaneous hydration appears to be a elusiveness of the disorder. common theme for most riskCUTIS factors and may help elucidate the pathogenesis of this disorder. The Epidemiology end result of this mechanism is inappropriate mel- Pityriasis alba primarily affects preadolescent children anosis manifesting as hypopigmentation. It must aged 3 to 16 years,4 with onset typically occurring be differentiated from other disorders of hypopig- between 6 and 12 years of age.5 Most patients are mentation, such as pityriasis versicolor alba, vitiligo, younger than 15 years,3 with up to 90% aged 6 to nevus depigmentosus, and nevus anemicus. -

A New Insight on Atopic Skin Diathesis: Is It Correlated with the Severity of Melasma
A New Insight on Atopic Skin Diathesis: Is It Correlated with the Severity of Melasma Danar Wicaksono1*, Rima Mustafa2, Sri Awalia Febriana1, Kristiana Etnawati1 1 Dermatovenereology Department, Faculty of Medicine Universitas Gadjah Mada – Dr. Sardjito General Hospital, Yogyakarta-Indonesia 2 Clinical Epidemiology and Biostatistics Unit, Faculty of Medicine Universitas Gadjah Mada –Dr. Sardjito General Hospital, Yogyakarta-Indonesia Keywords: Melasma, atopic skin diathesis (ASD), MASI score, atopic dermatitis (AD) Abstract: Melasma is a macular lesion of light brown to dark on the sun-exposed area, especially on the face. Atopic Skin Diathesis (ASD) is a clinical term to describe skin atopics with previous, present or future atopic dermatitis (AD). Dennie-Morgan infraorbital folds are secondary creases in the skin below the lower eyelids with a sensitivity of 78% and a specificity of 76% to diagnose AD. Melasma skin is characterized by impaired stratum corneum integrity and a delayed barrier recovery rate. Barrier dysfunction will stimulate keratinocyte to secrete keratinocyte-derived factor, which plays role in skin pigmentation process in melasma. To analyze correlation between ASD and Melasma Area Severity Index (MASI) score in melasma patient. This study is an observational analytic study with cross sectional design. Measurement of ASD and MASI score were done in 60 subjects with melasma who went to dermatology outpatient clinic Dr. Sardjito General Hospital from July 2017 to Januari 2018. The correlation between ASD and MASI score was analyzed using Pearson correlation. The result of this study showed no significant correlation between ASD and MASI scores (r: 0.02, p: 0,85). Crude Relative Risk (RR) for Dennie-Morgan infraorbital folds and MASI score was 4 (1.01-15.87). -

Comparative Study of Therapeutic Efficacy of Puva, Nbuvb and Puvasol in the Treatment of Chronic Plaque Type Psoriasis
COMPARATIVE STUDY OF THERAPEUTIC EFFICACY OF PUVA, NBUVB AND PUVASOL IN THE TREATMENT OF CHRONIC PLAQUE TYPE PSORIASIS Dissertation Submitted in Partial fulfillment of the University regulations for MD DEGREE IN DERMATOLOGY, VENEREOLOGY AND LEPROSY (BRANCH XX) MADRAS MEDICAL COLLEGE THE TAMILNADU DR.M.G.R. MEDICAL UNIVERSITY CHENNAI, INDIA. APRIL 2013 CERTIFICATE Certified that this dissertation titled “COMPARATIVE STUDY OF THERAPEUTIC EFFICACY OF PUVA, NBUVB AND PUVASOL IN THE TREATMENT OF CHRONIC PLAQUE TYPE PSORIASIS” is a bonafide work done by Dr.R.AKILA, Post graduate student of the Department of Dermatology, Venereology and Leprosy, Madras Medical College, Chennai – 3, during the academic year 2010 – 2013. This work has not previously formed the basis for the award of any degree. Prof.Dr.K.MANOHARAN MD.,D.D., Professor and Head of the Department, Department of Dermatology, Madras Medical College& Rajiv Gandhi Govt.General Hospital,Chennai-3. Prof. Dr.V. KANAGASABAI, M.D., Dean, Madras Medical College& Rajiv Gandhi Govt. General Hospital,Chennai-3. DECLARATION I, Dr.R.AKILA solemnly declare that this dissertation titled “COMPARATIVE STUDY OF THERAPEUTIC EFFICACY OF PUVA, NBUVB AND PUVASOL IN THE TREATMENT OF CHRONIC PLAQUE TYPE PSORIASIS” is a bonafide work done by me at Madras Medical College during 2010-2013 under the guidance and supervision of Prof. K.MANOHARAN, M.D.,D.D., Professor and head of the department of Dermatology, Madras Medical College,Chennai-600003. This dissertation is submitted to The Tamil Nadu Dr.M.G.R.Medical University, Chennai towards partial fulfillment of the rules and regulations for the award of M.D Degree in Dermatology, Venereology and Leprosy (BRANCH – XX) PLACE : DATE : (Dr. -

Phototherapy in Pediatric Patients: Choosing the Appropriate Treatment Option Rupa Pugashetti, BA* and John Koo, MD†
Phototherapy in Pediatric Patients: Choosing the Appropriate Treatment Option Rupa Pugashetti, BA* and John Koo, MD† Phototherapeutic modalities, including narrowband-UVB, broadband-UVB, PUVA photo- chemotherapy, and excimer laser therapy are valuable tools that can be used for photore- sponsive dermatoses in children. As a systematically safer alternative compared with internal agents, including the prebiologic and biological therapies, phototherapy should be considered a possible treatment option for children with diseases including psoriasis, atopic dermatitis, pityriasis lichenoides chronica, and vitiligo. Semin Cutan Med Surg 29:115-120 © 2010 Published by Elsevier Inc. hen choosing appropriate therapies for dermatologic adults. NBUVB represents a notable advance in phototherapy Wconditions in the pediatric population, clinicians and is considered more efficacious than BBUVB in the treat- must not only consider disease severity and morphology but ment of psoriasis, mycosis fungoides (MF), and vitiligo. also the general systemic safety profile of the treatment. For- NBUVB also has been increasingly tested in the pediatric tunately, many diseases, including psoriasis, atopic dermati- population as a therapy for diseases, including psoriasis, viti- tis, vitiligo, and pityriasis lichenoides, are photoresponsive ligo, pityriasis lichenoides, MF, and atopic dermatitis. dermatoses for which phototherapy represents an especially valuable treatment option. The pediatric population is a spe- Psoriasis cial population for whom it is important to avoid systemic agents and their associated potential risks whenever possible. Psoriasis is a chronic inflammatory skin disease that can be- Phototherapy represents a safe alternative for appropriately gin at any age and accounts for approximately 2% of visits to selected cases. There are 4 phototherapeutic options: nar- pediatric dermatologists. -

Light Therapy for Vitiligo
MEDICAL COVERAGE GUIDELINES ORIGINAL EFFECTIVE DATE: 06/11/14 SECTION: MEDICINE LAST REVIEW DATE: LAST CRITERIA REVISION DATE: ARCHIVE DATE: LIGHT THERAPY FOR VITILIGO Coverage for services, procedures, medical devices and drugs are dependent upon benefit eligibility as outlined in the member's specific benefit plan. This Medical Coverage Guideline must be read in its entirety to determine coverage eligibility, if any. The section identified as “Description” defines or describes a service, procedure, medical device or drug and is in no way intended as a statement of medical necessity and/or coverage. The section identified as “Criteria” defines criteria to determine whether a service, procedure, medical device or drug is considered medically necessary or experimental or investigational. State or federal mandates, e.g., FEP program, may dictate that any drug, device or biological product approved by the U.S. Food and Drug Administration (FDA) may not be considered experimental or investigational and thus the drug, device or biological product may be assessed only on the basis of medical necessity. Medical Coverage Guidelines are subject to change as new information becomes available. For purposes of this Medical Coverage Guideline, the terms "experimental" and "investigational" are considered to be interchangeable. BLUE CROSS®, BLUE SHIELD® and the Cross and Shield Symbols are registered service marks of the Blue Cross and Blue Shield Association, an association of independent Blue Cross and Blue Shield Plans. All other trademarks and service marks contained in this guideline are the property of their respective owners, which are not affiliated with BCBSAZ. Description: Vitiligo is an idiopathic skin disorder that causes depigmentation of sections of skin, most commonly on the extremities. -
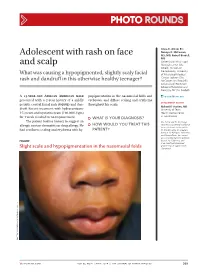
Adolescent with Rash on Face and Scalp
Photo RoUNDS Anna K. Allred, BS; Nancye K. McCowan, Adolescent with rash on face MS, MD; Robert Brodell, MD University of Mississippi and scalp Medical Center (Ms. Allred); Division of Dermatology, University What was causing a hypopigmented, slightly scaly facial of Mississippi Medical Center, Jackson (Drs. rash and dandruff in this otherwise healthy teenager? McCowan and Brodell); University of Rochester School of Medicine and Dentistry, NY (Dr. Brodell) A 13-year-old African American male popigmentation in the nasomesial folds and [email protected] presented with a 2-year history of a mildly eyebrows, and diffuse scaling and erythema DEpartment EDItOR pruritic central facial rash (FIGURE) and dan- throughout his scalp. Richard p. Usatine, MD druff. Recent treatment with hydrocortisone University of Texas 1% cream and nystatin cream (100,000 U/gm) Health Science Center at San Antonio for 1 week resulted in no improvement. ● What is youR diAgnosis? The patient had no history to suggest an Ms. Allred and Dr. McCowan allergic contact dermatitis or drug allergy. He ● HoW Would you TReAT THIS reported no potential conflict of interest relevant to this article. had confluent scaling and erythema with hy- pATIENT? Dr. Brodell serves on speaker’s bureaus for Allergan, Galderma, and PharmaDerm, has served as a consultant and on advisory Figure boards for Galderma, and is an investigator/received grant/research support from Slight scale and hypopigmentation in the nasomesial folds Genentech. PHO T o COU RT ESY OF : R o B e RT BR ODELL , MD jfponline.com Vol 63, no 4 | ApRIL 2014 | The jouRnAl of Family PracTice 209 PHOTO RoUNDS Diagnosis: the Malassezia yeast and topical steroids are Seborrheic dermatitis used to suppress inflammation. -

Pattern of Skin Diseases in a Rural Village Development Community of Nepal Shrestha R1, Lama L2, Gurung D3, Shrestha DP4, Rosdahl I5
Vol. 12, No. 1, 2014 Original Article Pattern Of Skin Diseases In A Rural Village Development Community Of Nepal Shrestha R1, Lama L2, Gurung D3, Shrestha DP4, Rosdahl I5 1,2Clinical Tutor, Department of Dermatology, Abstract National Academy of Medical Sciences, Bir Introduction: Skin diseases are a common cause of morbidity in Hospital, Kathmandu, Nepal; 3Consultant Nepal as per the health services report. There is limited information Dermatologist, DI Skin Hospital and Research on the prevalence and pattern of skin diseases in the community. Center, Kathmandu, Nepal; 4Professor, Department of Dermatology & Venereology, Institute of Objectives: This study was conducted to determine the pattern of Medicine, Maharajgunj Medical Campus, skin diseases in a rural village development community of Nepal. Kathmandu, Nepal; 5Visiting Professor, Department of Dermatology, Kathmandu Medical College, Material and methods: Two dermatologic health camps were Kathmandu, Nepal. conducted, during which, the villagers were examined by dermatologists. The skin diseases diagnosed were recorded in a Address for correspondence proforma. Dr. Dwarika P Shrestha Results: There were 433 individuals examined and 359 (male-47.9%; female-52.1%) had skin disease identified clinically (camp prevalence- Department of Dermatology, IOM, 83%). The age of patients ranged from 1 to 80 years (mean-24.5; Kathmandu, Nepal SD±15.9), with majority in the age group of 10-19 years. The most Telephone: 5592217; common skin disease category was eczemas (36.4%), followed by E-mail: [email protected] infections (28.4%), acne (22%), pigment disorders (34%) and urticaria (12.3%). Citation Conclusion: Skin diseases were common in the community. The Shrestha R, Lama L, Gurung D, Shrestha DP, five most common Skin disease categories were eczemas, infections, Rosdahl I. -

Discoid Lupus Erythematosus: First Clue to ……
Discoid lupus erythematosus: First clue to ……. Sri Lanka Journal of Child Health , 2016; 45 (4): 279-280 Case Reports Discoid lupus erythematosus: First clue to autoimmune haemolytic anaemia in a child *K M D Mallesh 1, Arun Basavanahalli Chandregowda 2, Prakash Javarappa 2 Sri Lanka Journal of Child Health , 2016; 45 (4): 279-280 DOI: http://dx.doi.org/10.4038/sljch.v45i4.8185 (Key words: Discoid lupus erythematosus; autoimmune haemolytic anaemia; cutaneous lupus) Introduction Criteria for diagnosing SLE. Child was treated with Discoid lupus erythematosus (DLE) is uncommon pulsed methyl prednisone (30mg/kg) for five days in the first decade of life. It has been described as followed by prednisone 1mg/kg/day for 4 weeks part of systemic lupus erythematosus (SLE) or in tapering over next 4 weeks. Congestive heart isolation in adults1. We report a case of severe failure was managed with furosemide and enalapril. haemolytic anaemia with discoid lesions that gave Discoid lesions were treated with topical a clue to diagnosis and management. triamcinolone acetonide 0.1% cream and sun screening. Lesions responded to treatment over 4 Case report weeks (Figure B). Haemoglobin level improved A 10 year old girl presented with headache, fever, and child was asymptomatic at latest follow up. weakness and skin lesions over face for 1 month. Child had been transfused with blood earlier for severe anaemia. Examination revealed severe pallor, jaundice, hepatosplenomegaly and congestive heart failure. There were two discoid, scaly macules with irregular margins and peripheral hyperpigmentation in the left side of the face below lower eyelid (Figure A). Investigations revealed a haemoglobin level of 4.7g/dl, dimorphic anaemia, positive direct Coombs test, positive antinuclear antibodies, negative venereal disease laboratory test, negative double stranded deoxyribonucleic acid, negative anti- phospholipid antibodies and negative ribonucleoprotein. -

Light Therapy for Dermatologic Conditions
Corporate Medical Policy Light Therapy for Dermatologic Conditions File Name: light_therapy_for_dermatologic_conditions Origination: 5/2012 Last CAP Review: 10/2020 Next CAP Review: 10/2021 Last Review: 10/2020 Description of Procedure or Service Light therapy for psoriasis and vitiligo includes both targeted phototherapy and photochemotherapy with psoralen plus ultraviolet A (PUVA). Targeted phototherapy describes the use of ultraviolet light that can be focused on specific body areas or lesions. PUVA uses a psoralen derivative in conjunction with long wavelength ultraviolet A (UVA) light (sunlight or artificial) for photochemotherapy of skin conditions. Psoriasis is a common chronic immune-mediated disease characterized by skin lesions ranging from minor localized patches to complete body coverage. There are several types of psoriasis; most common is plaque psoriasis which is associated with red and white scaly patches on the skin. In addition to being a skin disorder, psoriasis can negatively impact many organ systems and is associated with an increased risk of cardiovascular disease, some types of cancer, and autoimmune diseases such celiac disease and Crohn disease. Psoralens are tricyclic furocoumarins that occur in certain plants and can also be synthesized. They are available in oral and topical forms. Oral PUVA is generally given 1.5 hours before exposure to UVA radiation. Topical PUVA therapy refers to directly applying the psoralen to the skin with subsequent exposure to UVA light. Bath PUVA is used in some European countries for generalized psoriasis, but the agent used, trimethylpsoralen, is not approved by the U.S. Food and Drug Administration (FDA). Paint PUVA and soak PUVA are other forms of topical application of psoralen and are often used for psoriasis localized to the palms and soles. -

A Rare Case of a Subepidermal Bullous Disorder in a Child
Pediatric dermatology Series Editor: Camila K. Janniger, MD Bullous Systemic Lupus Erythematosus With Lupus Nephritis: A Rare Case of a Subepidermal Bullous Disorder in a Child Shital Poojary, MD, FCPS, DNB; Sama Rais, MBBS Bullous systemic lupus erythematosus (BSLE) characterized by a distinct constellation of clini- is a rare subset of systemic lupus erythemato- cal, histologic, and immunologic features.1 Bullous sus (SLE) with bullous lesions in a case fulfilling the systemic lupus erythematosus is extremely rare in American Rheumatism Association (Atlanta) crite- children.2 We report a case of a 9-year-old Indian girl ria, histologically characterized by a neutrophil- with BSLE and lupus nephritis; we review the clinical predominant infiltrate in theCUTIS upper dermis with features as well as the etiopathogenesis of BSLE. immunoglobulin (IgG, IgA, IgM) and C3 deposi- tion at the basement membrane zone (BMZ). It Case Report often is associated with autoimmunity to type VII A 9-year-old girl presented with a blistering eruption collagen (NC1 [noncollagenous domain 1] over her chest, back, arms, and neck of 15 days’ dura- domain), although occasionally other antigens tion; swelling around the eyes and feet of 15 days’ such as laminin 5, laminin 6, and BP230 (bullous duration; and a low-grade fever of 2 months’ dura- pemphigoidDo antigen) have beenNot described. Bullous tion. PhysicalCopy examination revealed multiple tense systemic lupus erythematosus is extremely rare vesicles and bullae overlying urticarial plaques on in children. the neck, chest (Figure 1), back, and arms with no We report here a case of a 9-year-old girl with mucous membrane involvement.