Anatomy of the Heart
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Direct Examination of Papillary Muscle Function in the Canine Left Ventricle
Loyola University Chicago Loyola eCommons Master's Theses Theses and Dissertations 1968 A Direct Examination of Papillary Muscle Function in the Canine Left Ventricle Robert Emmet Cronin Loyola University Chicago Follow this and additional works at: https://ecommons.luc.edu/luc_theses Part of the Medicine and Health Sciences Commons Recommended Citation Cronin, Robert Emmet, "A Direct Examination of Papillary Muscle Function in the Canine Left Ventricle" (1968). Master's Theses. 2081. https://ecommons.luc.edu/luc_theses/2081 This Thesis is brought to you for free and open access by the Theses and Dissertations at Loyola eCommons. It has been accepted for inclusion in Master's Theses by an authorized administrator of Loyola eCommons. For more information, please contact [email protected]. This work is licensed under a Creative Commons Attribution-Noncommercial-No Derivative Works 3.0 License. Copyright © 1968 Robert Emmet Cronin A DIRECT EXAMINATION OF PAPILLARY MUSCLE FUNCTION IN THE CANINE LEFT VENTRICLE by Robert Emmet Cronin A Thesis Submitted to the Faculty of the Graduate School of Loyola University in Partial Fulfillment of the Requirements for the Degree of Master of Science June 1968 LIFE Robert E. Cronin was born in Chicago, Illinois, on March 26, 1942. He attended St. Ignatius High School, in Chicago, Illinois, and then Holy Cross College in Worcester, Massachusetts, where he received his Bachelor of Arts degree in 1964. Since September, 1964, he has been a medical student at Loyola Uni versity, Stritch School of Medicine, and will receive his M.D. degree in June, 1968. For the past three years he has been enrolled in the combined Master of Science - Medical . -

Physiology of Heart Unit-4 (ZOOA-CC4-9-TH)
Physiology of Heart Unit-4 (ZOOA-CC4-9-TH) Coronary Circulation: The heart muscle, like every other organ or tissue in your body, needs oxygen-rich blood to survive. Blood is supplied to the heart by its own vascular system, called coronary circulation. The aorta (the main blood supplier to the body) branches off into two main coronary blood vessels (also called arteries). These coronary arteries branch off into smaller arteries, which supply oxygen-rich blood to the entire heart muscle. The right coronary artery supplies blood mainly to the right side of the heart. The right side of the heart is smaller because it pumps blood only to the lungs. The left coronary artery, which branches into the left anterior descending artery and the circumflex artery, supplies blood to the left side of the heart. The left side of the heart is larger and more muscular because it pumps blood to the rest of the body. Coronary circulation is the circulation of blood in the blood vessels that supply the heart muscle (myocardium). Coronary arteries supply oxygenated blood to the heart muscle, and cardiac veins drain away the blood once it has been deoxygenated. Because the rest of the body, and most especially the brain, needs a steady supply of oxygenated blood that is free of all but the slightest interruptions, the heart is required to function continuously. Therefore its circulation is of major importance not only to its own tissues but to the entire body and even the level of consciousness of the brain from moment to moment. -

4B. the Heart (Cor) 1
Henry Gray (1821–1865). Anatomy of the Human Body. 1918. 4b. The Heart (Cor) 1 The heart is a hollow muscular organ of a somewhat conical form; it lies between the lungs in the middle mediastinum and is enclosed in the pericardium (Fig. 490). It is placed obliquely in the chest behind the body of the sternum and adjoining parts of the rib cartilages, and projects farther into the left than into the right half of the thoracic cavity, so that about one-third of it is situated on the right and two-thirds on the left of the median plane. Size.—The heart, in the adult, measures about 12 cm. in length, 8 to 9 cm. in breadth at the 2 broadest part, and 6 cm. in thickness. Its weight, in the male, varies from 280 to 340 grams; in the female, from 230 to 280 grams. The heart continues to increase in weight and size up to an advanced period of life; this increase is more marked in men than in women. Component Parts.—As has already been stated (page 497), the heart is subdivided by 3 septa into right and left halves, and a constriction subdivides each half of the organ into two cavities, the upper cavity being called the atrium, the lower the ventricle. The heart therefore consists of four chambers, viz., right and left atria, and right and left ventricles. The division of the heart into four cavities is indicated on its surface by grooves. The atria 4 are separated from the ventricles by the coronary sulcus (auriculoventricular groove); this contains the trunks of the nutrient vessels of the heart, and is deficient in front, where it is crossed by the root of the pulmonary artery. -

Euler's Elastica-Based Biomechanics of the Papillary Muscle
materials Article Euler’s Elastica-Based Biomechanics of the Papillary Muscle Approximation in Ischemic Mitral Valve Regurgitation: A Simple 2D Analytical Model Francesco Nappi 1,*, Angelo Rosario Carotenuto 2, Sanjeet Singh Avtaar Singh 3, Christos Mihos 4 and Massimiliano Fraldi 2 1 Centre Cardiologique du Nord de Saint-Denis, Paris 36 Rue des Moulins Gmeaux, 93200 Saint-Denis, France 2 Department of Structures for Engineering and Architecture, University of Napoli Federico II, 80125 Naples, Italy; [email protected] (A.R.C.); [email protected] (M.F.) 3 Department of Cardiac Surgery, Golden Jubilee National Hospital, Clydebank G81 4DY, UK; [email protected] 4 Columbia University Division of Cardiology at the Mount Sinai Heart Institute, Miami Beach, FL 33140, USA; [email protected] * Correspondence: [email protected]; Tel.: +33-149-334-104; Fax: +33-149-334-119 Received: 16 March 2019; Accepted: 30 April 2019; Published: 9 May 2019 Abstract: Ischemic mitral regurgitation (IMR) occurs as an adverse consequence of left ventricle remodeling post-myocardial infarction. A change in mitral valve configuration with an imbalance between closing and tethering forces underlie this pathological condition. These abnormalities lead to impaired leaflet coaptation and a variable degree of mitral regurgitation, which can in turn influence the ventricular filling status, the heart rhythm and the afterload regardless of the residual ischemic insult. The IMR correction can be pursued through under-sizing mitral annuloplasty and papillary muscle approximation to restore the mitral valve and left ventricle physiological geometry to, consequently, achieve normalization of the engaged physical forces. Because the structures involved undergo extremely large deformations, a biomechanics model based on the Euler’s Elastica –the mitral leaflet– interlaced with nonlinear chordae tendineae anchored on papillary muscles has been constructed to elucidate the interactions between closing and tethering forces. -
Chapter 12 the Cardiovascular System: the Heart Pages
CHAPTER 12 THE CARDIOVASCULAR SYSTEM: THE HEART PAGES 388 - 411 LOCATION & GENERAL FEATURES OF THE HEART TWO CIRCUIT CIRCULATORY SYSTEM DIVISIONS OF THE HEART FOUR CHAMBERS Right Atrium Left Atrium Receives blood from Receives blood from the systemic circuit the pulmonary circuit FOUR CHAMBERS Right Ventricle Left Ventricle Ejects blood into the Ejects blood into the pulmonary circuit systemic circuit FOUR VALVES –ATRIOVENTRICULAR VALVES Right Atrioventricular Left Atrioventricular Valve (AV) Valve (AV) Tricuspid Valve Bicuspid Valve and Mitral Valve FOUR VALVES –SEMILUNAR VALVES Pulmonary valve Aortic Valve Guards entrance to Guards entrance to the pulmonary trunk the aorta FLOW OF BLOOD MAJOR VEINS AND ARTERIES AROUND THE HEART • Arteries carry blood AWAY from the heart • Veins allow blood to VISIT the heart MAJOR VEINS AND ARTERIES ON THE HEART Coronary Circulation – Supplies blood to the muscle tissue of the heart ARTERIES Elastic artery: Large, resilient vessels. pulmonary trunk and aorta Muscular artery: Medium-sized arteries. They distribute blood to skeletal muscles and internal organs. external carotid artery of the neck Arteriole: Smallest of arteries. Lead into capillaries VEINS Large veins: Largest of the veins. Superior and Inferior Vena Cava Medium-sized veins: Medium sized veins. Pulmonary veins Venules: the smallest type of vein. Lead into capillaries CAPILLARIES Exchange of molecules between blood and interstitial fluid. FLOW OF BLOOD THROUGH HEART TISSUES OF THE HEART THE HEART WALL Pericardium Outermost layer Serous membrane Myocardium Middle layer Thick muscle layer Endocardium Inner lining of pumping chambers Continuous with endothelium CARDIAC MUSCLE Depend on oxygen to obtain energy Abundant in mitochondria In contact with several other cardiac muscles Intercalated disks – interlocking membranes of adjacent cells Desmosomes Gap junctions CONNECTIVE TISSUE Wrap around each cardiac muscle cell and tie together adjacent cells. -

The Biomechanical Puncture Study of the Fossa Ovalis in Human and Porcine Hearts Daniel S
The Biomechanical Puncture Study of the Fossa Ovalis in Human and Porcine Hearts Daniel S. Balto, Steven A. Howard, BMEn., Paul A. Iaizzo, Ph.D.2 Departments of Biomedical Engineering1 and Surgery2 University of Minnesota, Minneapolis, MN 55455 Introduction Apparatus Conclusion Approximately 1 in 4 humans on this earth is born with a congenital heart •The apparatus designed for this study was great for initial testing of the defect that involves the failure of the complete formation of the fossa ovalis tissue properties of the fossa ovalis of large mammalian hearts, either of membrane between the left and right atria1. This defect, better known as a PFO research animals or of human donor hearts. However, physiological or Patent Fossa Ovalis is an opening in the fossa ovalis membrane that results properties weren’t really observed in the testing and so that is a starting from the failure of the fetal structures (septum primum and septum secundum) point for advancing the quality of this research. The ability for the system to from closing together at the moment of birth2. The opening can be classified in have interchangeable depression, puncture, and dilation devices adds to the a variety of ways, but the most common are “shunts” which cause blood to flexibility of the current setup. The visualization of the inside of the heart flow from one atria to the other. A shunt that results in the blood flowing from adds a new dimension to this research as well since it is able to visualize all the left to right atria will cause the blood pressure to increase in the right side cardiac structures under ~10 mmHg of pressure. -

Premature Obliteration of the Foramen Ovale by G
PREMATURE OBLITERATION OF THE FORAMEN OVALE BY G. AUSTIN GRESHAM From the Department of Pathology, University of Cambridge Received August 16, 1955 Obliteration of the foramen ovale occurring during intrauterine life is a rare condition. It throws some light on the mechanism of development of endocardial fibroelastosis and also upon the factors concerned in determining the size of the aorta and of the cardiac chambers. CASE HISTORY The patient was the second child of a mother (aet. 21) whose previous obstetric history was normal. Apart from two periods of rather rapid gain of weight for which no cause could be found, the pregnancy was uneventful. The child was eleven days postmature; labour was induced with an enema and lasted forty-five minutes. The infant cried lustily but was cyanosed: the heart was clinically normal. Abnormalities were present in all four limbs. The left radius and ulna were absent and rudimentary digits were present on the skin over the distal end of the limb. Terminal phalanges were absent in the fingers of the right hand, and four toes were present on each foot with a rudimentary fifth digit on the left foot. Cyanosis and dyspniea became more intense and the child died three hours after birth despite the use of oxygen. NECROPSY The body was that of a full-term male infant (weight 3430 g.). The limbs were abnormal as previously described. The lips were blue-black in colour. On the septal wall of the right atrium a hemispherical grey-white area (10x 12 x 4 mm. deep) with a central dimple filled in the usual site of the fossa ovalis (Fig. -

Cardiology Self Learning Package
Cardiology Self Learning Package Module 1: Anatomy and Physiology of the Module 1: Anatomy and Physiology of the Heart Heart. Page 1 Developed by Tony Curran (Clinical Nurse Educator) and Gill Sheppard (Clinical Nurse Specialist) Cardiology (October 2011) CONTENT Introduction…………………………………………………………………………………Page 3 How to use the ECG Self Learning package………………………………………….Page 4 Overview of the Heart…………………………………………………...…………..…….Page 5 Location, Size and Shape of the Heart…………………………………………………Page 5 The Chambers of the Heart…………….………………………………………..……….Page 7 The Circulation System……………………………………….………………..…………Page 8 The Heart Valve Anatomy………………………….…………………………..…………Page 9 Coronary Arteries…………………………………………….……………………..……Page 10 Coronary Veins…………………………………………………………………..……….Page 11 Cardiac Muscle Tissue……………………………………………………………..……Page 12 The Conduction System………………………………………………………………...Page 13 Cardiac Cycle……………………………………………………………………………..Page 15 References…………………………………………………………………………………Page 18 Module Questions………………………………………………………………………..Page 19 Module Evaluation Form………………………………………………………………..Page 22 [Module 1: Anatomy and Physiology of the Heart Page 2 Developed by Tony Curran (Clinical Nurse Educator) and Gill Sheppard (Clinical Nurse Specialist) Cardiology (October 2011) INTRODUCTION Welcome to Module 1: Anatomy and Physiology of the Heart. This self leaning package is designed to as tool to assist nurse in understanding the hearts structure and how the heart works. The goal of this module is to review: Location , size and shape of the heart The chambers of the heart The circulation system of the heart The heart’s valve anatomy Coronary arteries and veins Cardiac muscle tissue The conduction system The cardiac cycle This module will form the foundation of your cardiac knowledge and enable you to understand workings of the heart that will assist you in completing other modules. Learning outcomes form this module are: To state the position of the heart, the size and shape. -
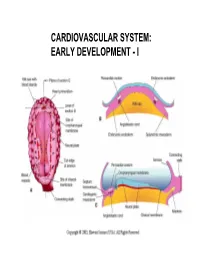
Cardiovascular System: Early Development
CARDIOVASCULAR SYSTEM: EARLY DEVELOPMENT - I CARDIOVASCULAR SYSTEM: EARLY DEVELOPMENT - II HEART AND ITS NEIGHBORHOOD- I HEART AND ITS NEIGHBORHOOD- II BLOOD VESSELS OF THE EMBRYO (at 26 days) FROM TUBE TO FOUR CHAMBERS EXTERNAL VIEW NORMAL : Loop to the RIGHT: Levocardia! ABNORMAL: Loop to the LEFT: Dextrocardia! FROM TUBE TO FOUR CHAMBERS INTERNAL VIEW FOUR CHAMBERS- ULTRASOUND VIEW @ 20 wks ATRIAL SEPTUM FORMATION- I ATRIAL SEPTUM FORMATION- II ATRIAL SEPTUM FORMATION- III ATRIAL SEPTUM FORMATION- IV ATRIAL SEPTUM FORMATION- V THE DEFINITIVE RIGHT ATRIUM **NOTE: In 25% of normal population, the foramen ovale remains ‘probe patent’. THE DEFINITIVE LEFT ATRIUM ATRIAL SEPTAL DEFECTS- “Fossa Ovalis” type ATRIAL SEPTAL DEFECTS- Unrelated to Foramen Ovale AORTIC ARCHES AND DERIVATIVES - I AORTIC ARCHES AND DERIVATIVES - II RECURRENT LARYNGEAL NERVES Right vs Left PATENT DUCTUS ARTERIOSUS Prostaglandin: Keeps the duct Patent Indomethacin: Closes the duct. RIGHT AORTIC ARCH: Mirror image branching ABERRANT RIGHT SUBCLAVIAN ARTERY: Occurs in 0.5% of people. Usually asymptomatic. DOUBLE AORTIC ARCH: “Vascular ring” Causes airway obstruction, stridor in infancy. COARCTATION OF THE AORTA THE CARDINAL VEINS AND THE VENAE CAVAE THE CARDINAL VEINS AND THE VENAE CAVAE SINUS VENOSUS AND THE CORONARY SINUS PERSISTENT LEFT SVC 0.3% of general population. 4 % of patients with Cong. Ht Dis. Usually drains to Coronary sinus. Usually asymptomatic. Enlarged coronary sinus is a clue. Left SVC to coronary sinus UMBILICAL AND VITELLINE VEINS- I: Liver, portal vein and ductus venosus. © 2005 Elsevier UMBILICAL AND VITELLINE VEINS- II: Liver, portal vein and ductus venosus. LYMPHATIC SYSTEM- I LYMPHATIC SYSTEM- II FETAL CIRCULATION POSTNATAL CIRCULATION. -

The Functional Anatomy of the Heart. Development of the Heart, Anomalies
The functional anatomy of the heart. Development of the heart, anomalies Anatomy and Clinical Anatomy Department Anastasia Bendelic Plan: Cardiovascular system – general information Heart – functional anatomy Development of the heart Abnormalities of the heart Examination in a living person Cardiovascular system Cardiovascular system (also known as vascular system, or circulatory system) consists of: 1. heart; 2. blood vessels (arteries, veins, capillaries); 3. lymphatic vessels. Blood vessels Arteries are blood vessels that carry blood away from the heart. Veins carry blood back towards the heart. Capillaries are tiny blood vessels, that connect arteries to veins. Lymphatic vessels: lymphatic capillaries; lymphatic vessels (superficial and deep lymph vessels); lymphatic trunks (jugular, subclavian, bronchomediastinal, lumbar, intestinal trunks); lymphatic ducts (thoracic duct and right lymphatic duct). Lymphatic vessels Microcirculation Microcirculatory bed comprises 7 components: 1. arterioles; 2. precapillaries or precapillary arterioles; 3. capillaries; 4. postcapillaries or postcapillary venules; 5. venules; 6. lymphatic capillaries; 7. interstitial component. Microcirculation The heart Heart is shaped as a pyramid with: an apex (directed downward, forward and to the left); a base (facing upward, backward and to the right). There are four surfaces of the heart: sternocostal (anterior) surface; diaphragmatic (inferior) surface; right pulmonary surface; left pulmonary surface. External surface of the heart The heart The heart has four chambers: right and left atria; right and left ventricles. Externally, the atria are demarcated from the ventricles by coronary sulcus (L. sulcus coronarius). The right and left ventricles are demarcated from each other by anterior and posterior interventricular sulci (L. sulci interventriculares anterior et posterior). Chambers of the heart The atria The atria are thin-walled chambers, that receive blood from the veins and pump it into the ventricles. -

Unit 1 Lecture 2
Unit 1 Lecture 2 Unit 1 Lecture 2 THE HEART Anatomy of the Heart The heart rests on the diaphragm in a space called the mediastinum. It weighs @ 300 grams and is about as big as a clenched fist. The pointed end is called the apex and the opposite end is called the base but is really the top of the heart. The bulk of the heart tissue is made up of the left ventricle. A pericardium (a 3-layered bag) surrounds the heart and composed of fibrous pericardium (that provides protection to the heart, prevents overstretching, and anchors the heart in the mediastinum), a serous pericardium which is composed of two layers (the parietal layer or outer layer that is fused to the fibrous pericardium and the visceral layer or the inner layer that adheres to heart muscle). The visceral pericardium is also called the epicardium. Pericardial fluid is found in the pericardial cavity, which is located between the two layers, helps lubricate and reduces friction between membranes as the heart moves. The heart wall is composed of three layers: the epicardium (see visceral pericardium above), the myocardium which is cardiac muscle tissue and the bulk of mass in the heart, and endocardium or the innermost layer of the heart. This lining is continuous through all of the blood vessels except for the capillaries. The Heart Chambers and Valves Internally the heart is divided into four chambers. The two upper chambers are the right and left atria. Each has an appendage (auricle) whose function is to increase the volume of the atria. -

THE HEART Study Objectives
THE HEART Study Objectives: You are responsible to understand the basic structure of the four chambered heart, the position and structure of the valves, and the path of blood flow through the heart. Structure--The Outer Layer pericardium: a specialized name for the celomic sac that surrounds the heart. fibrous pericardium: the most outer, fibrous layer of the pericardium. serous pericardium: there are two surfaces (layers) to this tissue a) parietal layer: the outer layer of the serosa surrounding the heart. Lines the fibrous pericardium, and the combination of the two layers is also called the parietal pericardium. b) visceral layer: the inner layer of the serosa surrounding and adhering to the heart. Also called the visceral pericardium or epicardium. pericardial cavity: the potential space between the parietal and visceral layers of the serous pericardium. The cavity is filled with serous fluid Structure--The Heart: Blood is delivered to the right atrium from the coronary sinus, inferior vena cava and superior vena cava Blood travels to the right ventricle from the right atrium via the right atrioventricular valve Blood travels from the left atrium to the left ventricle via the left atrioventricular valve Blood leaves the heart via the pulmonary valve to the pulmonary trunk, is delivered to the lungs for oxygenation and returns via the pulmonary veins to the left atrium a) crista terminalis: separates the anterior rough-walled and posterior smooth-walled portions of the right atrium. b) right auricle: small, conical, muscular, pouch-like appendage. c) musculi pectinate (pectinate muscles): internal muscular ridges that fan out anteriorly from the crista terminalis.