Obstructive Sleep Apnea and Dementia-Common Gene Associations Through Network-Based Identification of Common Driver Genes
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Human Artificial Chromosome (Hac) Vector
Europäisches Patentamt *EP001559782A1* (19) European Patent Office Office européen des brevets (11) EP 1 559 782 A1 (12) EUROPEAN PATENT APPLICATION published in accordance with Art. 158(3) EPC (43) Date of publication: (51) Int Cl.7: C12N 15/09, C12N 1/15, 03.08.2005 Bulletin 2005/31 C12N 1/19, C12N 1/21, C12N 5/10, C12P 21/02 (21) Application number: 03751334.8 (86) International application number: (22) Date of filing: 03.10.2003 PCT/JP2003/012734 (87) International publication number: WO 2004/031385 (15.04.2004 Gazette 2004/16) (84) Designated Contracting States: • KATOH, Motonobu, Tottori University AT BE BG CH CY CZ DE DK EE ES FI FR GB GR Yonago-shi, Tottori 683-8503 (JP) HU IE IT LI LU MC NL PT RO SE SI SK TR • TOMIZUKA, Kazuma, Designated Extension States: Kirin Beer Kabushiki Kaisha AL LT LV MK Takashi-shi, Gunma 370-1295 (JP) • KUROIWA, Yoshimi, (30) Priority: 04.10.2002 JP 2002292853 Kirin Beer Kabushiki Kaisha Takasaki-shi, Gunma 370-1295 (JP) (71) Applicant: KIRIN BEER KABUSHIKI KAISHA • KAKEDA, Minoru, Kirin Beer Kabushiki Kaisha Tokyo 104-8288 (JP) Takasaki-shi, Gunma 370-1295 (JP) (72) Inventors: (74) Representative: HOFFMANN - EITLE • OSHIMURA, Mitsuo, Tottori University Patent- und Rechtsanwälte Yonago-shi, Tottori 683-8503 (JP) Arabellastrasse 4 81925 München (DE) (54) HUMAN ARTIFICIAL CHROMOSOME (HAC) VECTOR (57) The present invention relates to a human arti- ing a cell which expresses foreign DNA. Furthermore, ficial chromosome (HAC) vector and a method for pro- the present invention relates to a method for producing ducing the same. -

Journal of Pediatric Gastroenterology and Nutrition, Publish Ahead of Print
Journal of Pediatric Gastroenterology and Nutrition, Publish Ahead of Print DOI : 10.1097/MPG.0000000000002462 Serologic, but not genetic, markers are associated with impaired anthropometrics at diagnosis of pediatric Crohn’s disease Authors: Sara K. Naramore, MD1, William E. Bennett, Jr., MD, MS1,2, Guanglong Jiang, MS3,4, Subra Kugathasan, MD5, Lee A. Denson, MD6, Jeffrey S. Hyams, MD7, Steven J. Steiner, MD1, and PRO-KIIDS Research Group8† 1Department of Pediatrics, Division of Pediatric Gastroenterology, Hepatology, and Nutrition, Indiana University School of Medicine, Indianapolis, IN 2Department of Pediatrics, Division of Pediatric and Adolescent Comparative Effectiveness Research, Indiana University School of Medicine, Indianapolis, IN 3Department of Medical & Molecular Genetics, Indiana University School of Medicine, Indianapolis, IN 4Department of BioHealth Informatics, Indiana University-Purdue University−Indianapolis, Indianapolis, IN 5Department of Pediatrics, Emory University School of Medicine, Atlanta, GA 6Department of Pediatrics, Cincinnati Children’s Hospital Medical Center, Cincinnati, OH 7Department of Pediatrics, Connecticut Children’s Medical Center, Hartford, CT 8PRO-KIIDS Research Group, New York, NY †Membership of the PRO-KIIDS Research Group is listed in the Acknowledgements. Principal Investigator and Corresponding Author: Sara Naramore, MD Department of Pediatrics Indiana University School of Medicine Riley Hospital for Children ____________________________________________________ This is the author's manuscript of the article published in final edited form as: Naramore, S. K., Bennett, W. E. J., Jiang, G., Kugathasan, S., Denson, L. A., Hyams, J. S., … Group, and P.-K. R. (2019). Serologic, but not Genetic, Markers are Associated with Impaired Anthropometrics at Diagnosis of Pediatric Crohn’s Disease. Journal of Pediatric Gastroenterology and Nutrition, Publish Ahead of Print. -

LETTER Doi:10.1038/Nature09515
LETTER doi:10.1038/nature09515 Distant metastasis occurs late during the genetic evolution of pancreatic cancer Shinichi Yachida1*, Siaˆn Jones2*, Ivana Bozic3, Tibor Antal3,4, Rebecca Leary2, Baojin Fu1, Mihoko Kamiyama1, Ralph H. Hruban1,5, James R. Eshleman1, Martin A. Nowak3, Victor E. Velculescu2, Kenneth W. Kinzler2, Bert Vogelstein2 & Christine A. Iacobuzio-Donahue1,5,6 Metastasis, the dissemination and growth of neoplastic cells in an were present in the primary pancreatic tumours from which the meta- organ distinct from that in which they originated1,2, is the most stases arose. A small number of these samples of interest were cell lines common cause of death in cancer patients. This is particularly true or xenografts, similar to the index lesions, whereas the majority were for pancreatic cancers, where most patients are diagnosed with fresh-frozen tissues that contained admixed neoplastic, stromal, metastatic disease and few show a sustained response to chemo- inflammatory, endothelial and normal epithelial cells (Fig. 1a). Each therapy or radiation therapy3. Whether the dismal prognosis of tissue sample was therefore microdissected to minimize contaminat- patients with pancreatic cancer compared to patients with other ing non-neoplastic elements before purifying DNA. types of cancer is a result of late diagnosis or early dissemination of Two categories of mutations were identified (Fig. 1b). The first and disease to distant organs is not known. Here we rely on data gen- largest category corresponded to those mutations present in all samples erated by sequencing the genomes of seven pancreatic cancer meta- from a given patient (‘founder’ mutations, mean of 64%, range 48–83% stases to evaluate the clonal relationships among primary and of all mutations per patient; Fig. -

(A) TCGA-LUAD, (B) TCGA-LUSC, (C) Database from Rizvi H, Et Al
Figure S1. The correlations of TMB value between panel sequencing and WES in published databases. (A) TCGA-LUAD, (B) TCGA-LUSC, (C) Database from Rizvi H, et al. J Clin Oncol, 2018;36. Abbreviations: TMB, tumor mutational burden; TCGA, The Cancer Genome Atlas; LUAD, lung adenocarcinoma; LUSC, lung squamous cell carcinoma; WES, wholeexome sequencing A B C 1 / 3 Figure S2. The comparison of multi-region tTMB among different NSCLC subtypes. Abbreviations: TMB, tumor mutational burden; tTMB, tissue TMB 2 / 3 Figure S3. The comparisons and overlaps of tumor-derived mutational profiles among tumor tissues in each region and the corresponding ctDNA. The P0XX was the patient No. shown at the top. Each tumor region (T1, T2, T3…) with plasma (P) were arranged in the x axis. ctDNA was isolated from plasma (more details in Supplementary Methods). Right y axis displayed tumor-derived mutational profiles in detail. The detected mutations were shown in red, while undetected cases were shown in gray. 3 / 3 P001 P004 P005 P006 P007 P009 P015 P018 KRAS.p.G12C ATG9B.p.R298C MORC1.p.G97V MLH1.p.L658V EGFR.p.L747_E749del SPTA1.p.S444C VAV1.p.R548W TP53.p.Y163C BAX.p.E41G CSMD3.p.H1455Y FAT1.p.R4481L CHI3L1.p.G37S DDR2.p.R478C APC.p.E2184K EPOR.p.R45P PTCH2.p.E854K TENM3.p.S44I EGFR.p.L858R U2AF1.p.S34F STK11.p.I238F MAEL.c.703.1G.C PIK3CA.p.R108H MSH6.p.S1340C EGFR.p.E746_A750del TSC1.p.R779. FLT1.p.K37E XRCC1.p.E455Q TP53.c.443.2A.C EGFR.p.A750P PPEF1.p.R348Q NTRK3.p.D208E TP53.p.Q105_S110delinsP DNMT3A.p.F563I NF1.p.A1228T CDK13.p.K852Nfs.23 POLR3B.c.1102.3_1102.2delTA COL6A6.p.P1542S MYD88.p.L265P FLT4.p.A601V TERT.c..58.u3403C.A ACIN1.p.K1047N ERBB2.p.G746delinsVC PRKCD.p.G210V EPHA3.p.T519M NOTCH1.p.Q2361. -

Deep Sequencing of the Human Retinae Reveals the Expression of Odorant Receptors
fncel-11-00003 January 20, 2017 Time: 14:24 # 1 CORE Metadata, citation and similar papers at core.ac.uk Provided by Frontiers - Publisher Connector ORIGINAL RESEARCH published: 24 January 2017 doi: 10.3389/fncel.2017.00003 Deep Sequencing of the Human Retinae Reveals the Expression of Odorant Receptors Nikolina Jovancevic1*, Kirsten A. Wunderlich2, Claudia Haering1, Caroline Flegel1, Désirée Maßberg1, Markus Weinrich1, Lea Weber1, Lars Tebbe2, Anselm Kampik3, Günter Gisselmann1, Uwe Wolfrum2, Hanns Hatt1† and Lian Gelis1† 1 Department of Cell Physiology, Ruhr-University Bochum, Bochum, Germany, 2 Department of Cell and Matrix Biology, Johannes Gutenberg University of Mainz, Mainz, Germany, 3 Department of Ophthalmology, Ludwig Maximilian University of Munich, Munich, Germany Several studies have demonstrated that the expression of odorant receptors (ORs) occurs in various tissues. These findings have served as a basis for functional studies that demonstrate the potential of ORs as drug targets for a clinical application. To the best of our knowledge, this report describes the first evaluation of the mRNA expression of ORs and the localization of OR proteins in the human retina that set a Edited by: stage for subsequent functional analyses. RNA-Sequencing datasets of three individual Hansen Wang, University of Toronto, Canada neural retinae were generated using Next-generation sequencing and were compared Reviewed by: to previously published but reanalyzed datasets of the peripheral and the macular Ewald Grosse-Wilde, human retina and to reference tissues. The protein localization of several ORs was Max Planck Institute for Chemical Ecology (MPG), Germany investigated by immunohistochemistry. The transcriptome analyses detected an average Takaaki Sato, of 14 OR transcripts in the neural retina, of which OR6B3 is one of the most highly National Institute of Advanced expressed ORs. -

A Rose Extract Protects the Skin Against Stress Mediators: a Potential Role of Olfactory Receptors
Supplementary data A Rose extract protects the skin against stress mediators: a potential role of olfactory receptors Romain Duroux 1,*, Anne Mandeau 1, Gaelle Guiraudie-Capraz 2, Yannick Quesnel 3 and Estelle Loing 4 1 IFF-Lucas Meyer Cosmetics, Toulouse, France 2 Aix-Marseille University, CNRS, INP, Marseille, France 3 ChemCom S.A., Brussels, Belgium 4 IFF-Lucas Meyer Cosmetics, Quebec, Canada * Correspondence: [email protected] Supplemental methods Keratinocytes cell culture and skin explants Skin organ cultures were prepared from tissues samples derived from volunteers undergoing routine therapeutic procedures, in collaboration with Alphenyx (Marseille). For this study, skin samples were derived from abdominal or breast tissues of healthy women (30-40 years old). Samples were received 1 day post-surgery and used directly for microdissection or cell extraction. Microdissected human skin was cultured at 37°C under 5% CO2, in DMEM (Dutscher, #L0060-500) plus 10% FBS (Sigma Aldrich, #F7524), 1% Penicillin/Streptomycin (Sigma Aldrich, #P0781-100), and 1% of minimum medium non-essential amino acids 10X (Gibco, #11140-035). For keratinocyte culture, cells were isolated from human skin epidermis. Briefly, skin samples were cut into small pieces and immersed in Thermolysin (Sigma Aldrich, #T7902-100mg) at 4°C overnight. Epidermis was then carefully detached from dermis before being incubated with Trypsin-EDTA for 15 minutes at 37°C. Trypsin inhibitor was next added, the mixture centrifuged and the supernatant discarded before adding KGM2 Medium (Promocell, #C- 20011) with 1% Penicillin/Streptomycin (Sigma Aldrich, #P0781-100). NHEK were then maintained in culture at 37 °C under 5 % CO2 and 95 % relative humidity. -
European Patent Office of Opposition to That Patent, in Accordance with the Implementing Regulations
(19) TZZ Z_T (11) EP 2 884 280 B1 (12) EUROPEAN PATENT SPECIFICATION (45) Date of publication and mention (51) Int Cl.: of the grant of the patent: G01N 33/566 (2006.01) 09.05.2018 Bulletin 2018/19 (21) Application number: 13197310.9 (22) Date of filing: 15.12.2013 (54) Method for evaluating the scent performance of perfumes and perfume mixtures Verfahren zur Bewertung des Duftverhaltens von Duftstoffen und Duftstoffmischungen Procédé d’evaluation de senteur performance du parfums et mixtures de parfums (84) Designated Contracting States: (56) References cited: AL AT BE BG CH CY CZ DE DK EE ES FI FR GB WO-A2-03/091388 GR HR HU IE IS IT LI LT LU LV MC MK MT NL NO PL PT RO RS SE SI SK SM TR • BAGHAEI KAVEH A: "Deorphanization of human olfactory receptors by luciferase and Ca-imaging (43) Date of publication of application: methods.",METHODS IN MOLECULAR BIOLOGY 17.06.2015 Bulletin 2015/25 (CLIFTON, N.J.) 2013, vol. 1003, 19 June 2013 (2013-06-19), pages229-238, XP008168583, ISSN: (73) Proprietor: Symrise AG 1940-6029 37603 Holzminden (DE) • KAVEH BAGHAEI ET AL: "Olfactory receptors coded by segregating pseudo genes and (72) Inventors: odorants with known specific anosmia.", 33RD • Hatt, Hanns ANNUAL MEETING OF THE ASSOCIATION FOR 44789 Bochum (DE) CHEMORECEPTION, 1 April 2011 (2011-04-01), • Gisselmann, Günter XP055111507, 58456 Witten (DE) • TOUHARA ET AL: "Deorphanizing vertebrate • Ashtibaghaei, Kaveh olfactory receptors: Recent advances in 44801 Bochum (DE) odorant-response assays", NEUROCHEMISTRY • Panten, Johannes INTERNATIONAL, PERGAMON PRESS, 37671 Höxter (DE) OXFORD, GB, vol. -

A Multispecific Investigation of the Metal Effect in Mammalian Odorant
Chemical Senses, 2018, Vol 00, 1–10 doi:10.1093/chemse/bjy022 Original Article Advance Access Publication Date: 06 April 2018 Original Article A Multispecific Investigation of the Metal Effect in Mammalian Odorant Receptors for Sulfur- Containing Compounds Ruina Zhang1,*, Yi Pan1,*, Lucky Ahmed2, Eric Block3, Yuetian Zhang1, Victor S. Batista2 and Hanyi Zhuang1,4 1Department of Pathophysiology, Key Laboratory of Cell Differentiation and Apoptosis of the Chinese Ministry of Education, Shanghai Jiaotong University School of Medicine, 227 South Chongqing Road, Huangpu District, Shanghai 200025, P. R. China, 2Department of Chemistry, Yale University, 225 Prospect Street, New Haven, CT 06520, USA, 3Department of Chemistry, University at Albany, State University of New York, 1400 Washington Avenue Albany, NY 12222, USA and 4Institute of Health Sciences, Shanghai Jiaotong University School of Medicine/Shanghai Institutes for Biological Sciences of Chinese Academy of Sciences, 320 Yueyang Road, Xuhui District, Shanghai 200031, P. R. China *These authors contributed equally to the work. Correspondence to be sent to: Hanyi Zhuang, Department of Pathophysiology, Key Laboratory of Cell Differentiation and Apoptosis of the Chinese Ministry of Education, Shanghai Jiaotong University School of Medicine, Shanghai 200025, P. R. China. e-mail: [email protected] and Victor S. Batista, Department of Chemistry, Yale University, New Haven, CT 06520, USA. e-mail: [email protected] Editorial Decision 15 March 2018. Abstract Metal-coordinating compounds are generally known to have strong smells, a phenomenon that can be attributed to the fact that odorant receptors for intense-smelling compounds, such as those containing sulfur, may be metalloproteins. We previously identified a mouse odorant receptor (OR), Olfr1509, that requires copper ions for sensitive detection of a series of metal-coordinating odorants, including (methylthio)methanethiol (MTMT), a strong-smelling component of male mouse urine that attracts female mice. -

Single Cell Derived Clonal Analysis of Human Glioblastoma Links
SUPPLEMENTARY INFORMATION: Single cell derived clonal analysis of human glioblastoma links functional and genomic heterogeneity ! Mona Meyer*, Jüri Reimand*, Xiaoyang Lan, Renee Head, Xueming Zhu, Michelle Kushida, Jane Bayani, Jessica C. Pressey, Anath Lionel, Ian D. Clarke, Michael Cusimano, Jeremy Squire, Stephen Scherer, Mark Bernstein, Melanie A. Woodin, Gary D. Bader**, and Peter B. Dirks**! ! * These authors contributed equally to this work.! ** Correspondence: [email protected] or [email protected]! ! Supplementary information - Meyer, Reimand et al. Supplementary methods" 4" Patient samples and fluorescence activated cell sorting (FACS)! 4! Differentiation! 4! Immunocytochemistry and EdU Imaging! 4! Proliferation! 5! Western blotting ! 5! Temozolomide treatment! 5! NCI drug library screen! 6! Orthotopic injections! 6! Immunohistochemistry on tumor sections! 6! Promoter methylation of MGMT! 6! Fluorescence in situ Hybridization (FISH)! 7! SNP6 microarray analysis and genome segmentation! 7! Calling copy number alterations! 8! Mapping altered genome segments to genes! 8! Recurrently altered genes with clonal variability! 9! Global analyses of copy number alterations! 9! Phylogenetic analysis of copy number alterations! 10! Microarray analysis! 10! Gene expression differences of TMZ resistant and sensitive clones of GBM-482! 10! Reverse transcription-PCR analyses! 11! Tumor subtype analysis of TMZ-sensitive and resistant clones! 11! Pathway analysis of gene expression in the TMZ-sensitive clone of GBM-482! 11! Supplementary figures and tables" 13" "2 Supplementary information - Meyer, Reimand et al. Table S1: Individual clones from all patient tumors are tumorigenic. ! 14! Fig. S1: clonal tumorigenicity.! 15! Fig. S2: clonal heterogeneity of EGFR and PTEN expression.! 20! Fig. S3: clonal heterogeneity of proliferation.! 21! Fig. -
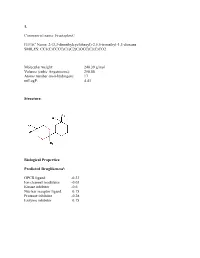
Sean Raspet – Molecules
1. Commercial name: Fructaplex© IUPAC Name: 2-(3,3-dimethylcyclohexyl)-2,5,5-trimethyl-1,3-dioxane SMILES: CC1(C)CCCC(C1)C2(C)OCC(C)(C)CO2 Molecular weight: 240.39 g/mol Volume (cubic Angstroems): 258.88 Atoms number (non-hydrogen): 17 miLogP: 4.43 Structure: Biological Properties: Predicted Druglikenessi: GPCR ligand -0.23 Ion channel modulator -0.03 Kinase inhibitor -0.6 Nuclear receptor ligand 0.15 Protease inhibitor -0.28 Enzyme inhibitor 0.15 Commercial name: Fructaplex© IUPAC Name: 2-(3,3-dimethylcyclohexyl)-2,5,5-trimethyl-1,3-dioxane SMILES: CC1(C)CCCC(C1)C2(C)OCC(C)(C)CO2 Predicted Olfactory Receptor Activityii: OR2L13 83.715% OR1G1 82.761% OR10J5 80.569% OR2W1 78.180% OR7A2 77.696% 2. Commercial name: Sylvoxime© IUPAC Name: N-[4-(1-ethoxyethenyl)-3,3,5,5tetramethylcyclohexylidene]hydroxylamine SMILES: CCOC(=C)C1C(C)(C)CC(CC1(C)C)=NO Molecular weight: 239.36 Volume (cubic Angstroems): 252.83 Atoms number (non-hydrogen): 17 miLogP: 4.33 Structure: Biological Properties: Predicted Druglikeness: GPCR ligand -0.6 Ion channel modulator -0.41 Kinase inhibitor -0.93 Nuclear receptor ligand -0.17 Protease inhibitor -0.39 Enzyme inhibitor 0.01 Commercial name: Sylvoxime© IUPAC Name: N-[4-(1-ethoxyethenyl)-3,3,5,5tetramethylcyclohexylidene]hydroxylamine SMILES: CCOC(=C)C1C(C)(C)CC(CC1(C)C)=NO Predicted Olfactory Receptor Activity: OR52D1 71.900% OR1G1 70.394% 0R52I2 70.392% OR52I1 70.390% OR2Y1 70.378% 3. Commercial name: Hyperflor© IUPAC Name: 2-benzyl-1,3-dioxan-5-one SMILES: O=C1COC(CC2=CC=CC=C2)OC1 Molecular weight: 192.21 g/mol Volume -

Chromophobe Renal Cell Carcinoma with and Without Sarcomatoid Change: a Clinicopathological, Comparative Genomic Hybridization, and Whole-Exome Sequencing Study
Am J Transl Res 2015;7(11):2482-2499 www.ajtr.org /ISSN:1943-8141/AJTR0014993 Original Article Chromophobe renal cell carcinoma with and without sarcomatoid change: a clinicopathological, comparative genomic hybridization, and whole-exome sequencing study Yuan Ren1*, Kunpeng Liu1*, Xueling Kang3, Lijuan Pang1, Yan Qi1, Zhenyan Hu1, Wei Jia1, Haijun Zhang1, Li Li1, Jianming Hu1, Weihua Liang1, Jin Zhao1, Hong Zou1*, Xianglin Yuan2, Feng Li1* 1Department of Pathology, School of Medicine, First Affiliated Hospital, Shihezi University, Key Laboratory of Xinjiang Endemic and Ethnic Diseases, Ministry of Education of China, Shihezi, China; 2Tongji Hospital Cancer Center, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China; 3Department of Pathology, Shanghai General Hospital, Shanghai, China. *Equal contributors. Received August 24, 2015; Accepted October 13, 2015; Epub November 15, 2015; Published November 30, 2015 Abstract: Chromophobe renal cell carcinomas (CRCC) with and without sarcomatoid change have different out- comes; however, fewstudies have compared their genetic profiles. Therefore, we identified the genomic alteration- sin CRCC common type (CRCC C) (n=8) and CRCC with sarcomatoid change (CRCC S) (n=4) using comparative genomic hybridization (CGH) and whole-exome sequencing. The CGH profiles showed that the CRCC C group had more chromosomal losses (72 vs. 18) but fewer chromosomal gains (23 vs. 57) than the CRCC S group. Losses of chromosomes 1p, 8p21-23, 10p16-20, 10p12-ter, 13p20-30, and 17p13 and gains of chromosomes 1q11, 1q21-23, 1p13-15, 2p23-24, and 3p21-ter differed between the groups. Whole-exome sequencing showed that the mutational status of 270 genes differed between CRCC (n=12) and normal renal tissues (n=18). -

Downloaded Per Proteome Cohort Via the Web- Site Links of Table 1, Also Providing Information on the Deposited Spectral Datasets
www.nature.com/scientificreports OPEN Assessment of a complete and classifed platelet proteome from genome‑wide transcripts of human platelets and megakaryocytes covering platelet functions Jingnan Huang1,2*, Frauke Swieringa1,2,9, Fiorella A. Solari2,9, Isabella Provenzale1, Luigi Grassi3, Ilaria De Simone1, Constance C. F. M. J. Baaten1,4, Rachel Cavill5, Albert Sickmann2,6,7,9, Mattia Frontini3,8,9 & Johan W. M. Heemskerk1,9* Novel platelet and megakaryocyte transcriptome analysis allows prediction of the full or theoretical proteome of a representative human platelet. Here, we integrated the established platelet proteomes from six cohorts of healthy subjects, encompassing 5.2 k proteins, with two novel genome‑wide transcriptomes (57.8 k mRNAs). For 14.8 k protein‑coding transcripts, we assigned the proteins to 21 UniProt‑based classes, based on their preferential intracellular localization and presumed function. This classifed transcriptome‑proteome profle of platelets revealed: (i) Absence of 37.2 k genome‑ wide transcripts. (ii) High quantitative similarity of platelet and megakaryocyte transcriptomes (R = 0.75) for 14.8 k protein‑coding genes, but not for 3.8 k RNA genes or 1.9 k pseudogenes (R = 0.43–0.54), suggesting redistribution of mRNAs upon platelet shedding from megakaryocytes. (iii) Copy numbers of 3.5 k proteins that were restricted in size by the corresponding transcript levels (iv) Near complete coverage of identifed proteins in the relevant transcriptome (log2fpkm > 0.20) except for plasma‑derived secretory proteins, pointing to adhesion and uptake of such proteins. (v) Underrepresentation in the identifed proteome of nuclear‑related, membrane and signaling proteins, as well proteins with low‑level transcripts.