Pdf 2.09 MB Angola Severe Malaria Assessment Report 2020
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
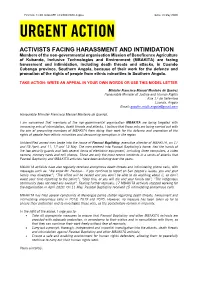
Angola: Activists Facing Harassment and Intimidation
First UA: 71/20 Index:AFR 12/2302/2020 Angola Date: 13 May 2020 URGENT ACTION ACTIVISTS FACING HARASSMENT AND INTIMIDATION Members of the non-governmental organisation Mission of Beneficence Agriculture of Kubando, Inclusive Technologies and Environment (MBAKITA) are facing harassment and intimidation, including death threats and attacks, in Cuando Cubango province, Southern Angola, because of their work for the defence and promotion of the rights of people from ethnic minorities in Southern Angola. TAKE ACTION: WRITE AN APPEAL IN YOUR OWN WORDS OR USE THIS MODEL LETTER Minister Francisco Manuel Monteiro de Queiroz Honourable Minister of Justice and Human Rights Rua 17 de Setembro Luanda, Angola Email: [email protected] Honourable Minister Francisco Manuel Monteiro de Queiroz, I am concerned that members of the non-governmental organisation MBAKITA are being targeted with increasing acts of intimidation, death threats and attacks. I believe that these acts are being carried out with the aim of preventing members of MBAKITA from doing their work for the defence and promotion of the rights of people from ethnic minorities and denouncing corruption in the region. Unidentified armed men broke into the house of Pascoal Baptistiny, executive director of MBAKITA, on 17 and 23 April, and 11, 12 and 13 May. The men entered into Pascoal Baptistiny’s home, tied the hands of the two security guards and took several items of electronic equipment, including three computers, a video camera, memory cards and cell phones. These are only the most recent incidents in a series of attacks that Pascoal Baptistiny and MBAKITA activists have been enduring over the years. -

Regional Project Proposal
ADSWAC Full Proposal [V.1] January 18, 2021 REGIONAL PROJECT PROPOSAL ADSWAC PROJECT RESILIENCE BUILDING AS CLIMATE CHANGE ADAPTATION IN DROUGHT-STRUCK SOUTH-WESTERN AFRICAN COMMUNITIES ANGOLA AND NAMIBIA Title of Project: RESILIENCE BUILDING AS CLIMATE CHANGE ADAPTATION IN DROUGHT-STRUCK SOUTH-WESTERN AFRICAN COMMUNITIES Countries: ANGOLA AND NAMIBIA Thematic Focal Area1: FOOD SECURITY Type of Implementing Entity: REGIONAL IMPLEMENTING ENTITY (RIE) Implementing Entity: SAHARA AND SAHEL OBSERVATORY (OSS) Executing Entities: REGIONAL: ADPP (AJUDA DE DESENVOLVIMENTO DE POVO PARA POVO) NATIONAL : ANGOLA: ADPP (AJUDA DE DESENVOLVIMENTO DE POVO PARA POVO) NAMIBIA: DAPP (DEVELOPMENT AID FROM PEOPLE TO PEOPLE) Amount of Financing Requested: 11,941,038 US DOLLARS 1 Thematic areas are: Food security; Disaster risk reduction and early warning systems; Transboundary water management; Innovation in adaptation finance. 1 ADSWAC Full Proposal [V.1] January 18, 2021 CONTENT PART PROJECT INFORMATION ................................................................................................................................... 5 1. Project Background and Context ................................................................................................................................. 5 1.1 Project Area Context .................................................................................................................................................... 5 1.2 Description of the Project sites ................................................................................................................................... -

CORB Homogeneous Units
Cubango-Okavango River Basin Homogenous Units Livelihoods vulnerability hotspot mapping July 2018 FINAL Acronyms Acronym Long Form CBNRM Community Based Natural Resource Management CORB Cubango Okavango River Basin CRIDF Climate Resilient Infrastructure Development Facility CSIR Council for Scientific and Industrial Research EU European Union GCM General Circulation Model HWC Human Wildlife Conflict KAZA Kavango-Zambezi RCM Regional Circulation Models RCP Representative Concentration Pathway SADC Southern African Development Community TNC The Nature Conservancy UNDP United Nations Development Programme WASH Water, Sanitation and Hygiene WDA Wildlife Dispersal Area www.cridf.com 1 Contents Acronyms 1 Preface 4 1 Preamble to Discussion 5 2 Climate model downscaling and climate impact assessment method 9 3 Homogenous unit 1: Menongue - Far northern part of CORB 12 3.1 Socio-Economic 12 3.2 Population 13 3.3 Infrastructure 15 3.4 Environmental 15 3.5 Transboundary impacts 16 3.6 Climate future 16 3.7 Understanding the vulnerabilities 17 3.8 Potential suitable technologies/interventions 17 4 Homogenous unit 2: Cuangar/Calai/Rundu - Angola/Namibia border sharing 18 4.1 Socio-Economic 18 4.2 Population 20 4.3 Infrastructure 20 4.4 Environmental 22 4.5 Transboundary impacts 22 4.6 Climate future 22 4.7 Understanding the vulnerabilities 23 4.8 Potential suitable technologies/interventions 23 5 Homogenous unit 3: Tsumkwe - ‘Dry’ Namibia/Botswana 24 5.1 Socio-Economic 24 5.2 Population 26 5.3 Infrastructure narrative 27 5.4 Environmental 29 5.5 -

Working Paper Reference
Working Paper Civil wars and state formation: violence and the politics of legitimacy in angola, côte d'ivoire and south sudan PECLARD, Didier, et al. Abstract Civil wars do not only destroy existing political orders. They contribute to shaping new ones, and thereby play a crucial role in dynamics of state formation. This working paper is based on a 2-year research project funded by the Swiss Network of International Studies and conducted by a consortium of five research institutions in Switzerland and Africa. It reflects on the social construction of order and legitimacy during and after violent conflict by focusing on political orders put in place by armed groups, their strategies to legitimize their (violent) action as well as their claim to power, and on the extent to which they strive and manage to institutionalize their military power and transform it into political domination. Drawing on case studies in Angola, Côte d'Ivoire and South Sudan, it shows how strategies of legitimization are central to understanding the politics of armed groups and their relation to the state, how international aid agencies impact on the legitimacy of armed groups and state actors, and how continuities between war and peace, especially in key sectors such as security forces, need to be taken [...] Reference PECLARD, Didier, et al. Civil wars and state formation: violence and the politics of legitimacy in angola, côte d'ivoire and south sudan. Geneva : University of Geneva / Swiss Network of International Studies (SNIS), 2019, 29 p. Available at: http://archive-ouverte.unige.ch/unige:134632 Disclaimer: layout of this document may differ from the published version. -

The Chronic Congestion in Luanda Is Dismissed by Some Experts
68 BUSINESS 69 ANGOLA TOO FAST FOR COMFORT The chronic congestion in Luanda is dismissed by some experts as a “small inconvenience”, with more and more investors piling in for a piece of the action in this rapidly growing economy Cars fill the roads and parking lots as ships queue to enter FRANÇOIS MISSER IN LUANDA the port of Luanda n some days, the aircraft arriving in Luanda disgorge hundreds of Chinese workers, all wea- ring the uniforms and hats of the construction firms that have hired them to work on the many construction sites around Angola. OBut any impression that this apparent ‘invasion’ is evidence of China’s scramble to control Africa’s new oil Eldorado is dis- missed as “a major misconception” by Ary Carvalho, a board member of Angola’s Agência Nacional para o Investimento Privado (ANIP). “The investment you see is the Angolan government’s investment in its own country,” he says. “People forget this. It is a credit line, which Angola is paying for on very good terms, for the railways, roads, schools and hospitals.” Carvalho estimates that China’s credit lines to Angola total $4bn. Others put the figure at $6bn, if funds via the China International Fund are included, even if not all of this has been spent, as evidenced by the delay in construction of the Benguela railway between Lobito and Katanga in the Democratic Republic of Congo. Talk of asset-stripping is certainly misplaced and China’s direct share of Angola’s oil exploration permits is modest. In 2007, Sinopec had to withdraw from a bid to build a 240,000- barrel per day (b/d) refinery in Lobito because it could not reach agreement with state oil company Sonangol, which wan- ted a facility that would produce export-quality petrol and diesel for the European and US markets. -

2.3 Angola Road Network
2.3 Angola Road Network Distance Matrix Travel Time Matrix Road Security Weighbridges and Axle Load Limits For more information on government contact details, please see the following link: 4.1 Government Contact List. Page 1 Page 2 Distance Matrix Uige – River Nzadi bridge 18 m-long and 4 m-wide near the locality of Kitela, north of Songo municipality destroyed during civil war and currently under rehabilitation (news 7/10/2016). Road Details Luanda The Government/MPLA is committed to build 1,100 km of roads in addition to 2,834 km of roads built in 2016 and planned rehabilitation of 7,083 km of roads in addition to 10,219 km rehabilitated in 2016. The Government goals will have also the support from the credit line of the R. of China which will benefit inter-municipality links in Luanda, Uige, Malanje, Cuanza Norte, Cuanza Sul, Benguela, Huambo and Bié provinces. For more information please vitsit the Website of the Ministry of Construction. Zaire Luvo bridge reopened to trucks as of 15/11/2017, this bridge links the municipality of Mbanza Congo with RDC and was closed for 30 days after rehabilitation. Three of the 60 km between MCongo/Luvo require repairs as of 17/11/2017. For more information please visit the Website of Agencia Angola Press. Works of rehabilitation on the road nr, 120 between Mbanza Congo (province Zaire) and the locality of Lukunga (province of Uige) of a distance of 111 km are 60% completed as of 29/9/2017. For more information please visit the Website of Agencia Angola Press. -

Praziquantel Mass Drug Administration Campaign for School-Aged Children in 3 Provinces of Angola November 2014. Provinces: Huamb
PRAZIQUANTEL MASS DRUG ADMINISTRATION CAMPAIGN FOR SCHOOL-AGED CHILDREN IN 3 PROVINCES OF ANGOLA NOVEMBER 2014. PROVINCES: HUAMBO, UÍGE E ZAIRE DISTRIBUTION CAMPAIGN FROM: 27 OCTOBER TO 08 NOVEMBER 2014 IMPLEMENTING PARTNERS: PROVINCIAL HEALTH DEPARTMENTS OF HUAMBO, UÍGE E ZAIRE PROVINCIAL EDUCATION DEPARTMENTS OF HUAMBO, UÍGE E ZAIRE THE MENTOR-INITIATIVE MUNICIPAL DEPARTMENTS OF HEALTH AND EDUCATION OF THE PROVINCES HUAMBO, UÍGE E ZAIRE. 1 JANUARY 2015 I. INTRODUCTION 3 II. PLANNING AND COORDINATION OF THE CAMPAIGN 4 III. SCHOOL-BASED TREATMENT CAMPAIGN PRAZIQUANTEL 7 1 - Methodology 7 2 – Distribution of the drugs 8 3- Treatment data collection and management 10 4- Results k10 IV. CHALLENGES 19 V. OPPORTUNITIES 20 VI. SUMMARY 21 2 I. INTRODUCTION The MENTOR Initiative is an international non-governmental organization dedicated to reducing death and suffering from malaria and neglected tropical diseases (NTDs) in humanitarian crises. Currently MENTOR is providing support to the most vulnerable communities in Angola, Liberia, Kenya, Central African Republic, South Sudan and Chad. The MENTOR is present in Angola since 2002, working with the National Malaria Control Program to reduce the burden of disease in the provinces of Huambo, Uíge and Zaire. Since 2011, MENTOR is implementing a private health sector malaria program in partnership with the Government and the NGO Population Services International (PSI), introducing combination therapies based on artemisinin (ACTs) and Rapid Diagnostic Tests (TDR) in private pharmacies. In partnership with the Government and the NGO World Learning, a public health malaria programme based on case management and capacity building within the National Health Structure is being implemented. In 2013, the MENTOR Initiative started the Neglected Tropical Disease control programme with the overall purpose to support the Ministry of Health of Angola to achieve a significant reduction in infections of Schistosomiasis, Soil Transmitted Helminths and Lymphatic Filariasis, in areas of high endemicity. -

Dismantled Poaching Net and Gun Snipers
27/07/2020 Dismantled poaching net and weapon snipers | Provinces | Jornal de Angola - Online Monday, 27 July 2020 17:56 Director: Victor Silva Deputy Director: Caetano Júnior PROVINCES Dismantled poaching net and gun snipers Carlos Paulino | Menongue July 27, 2020 In all, 11 nationals, including firearm suppliers, poachers and game vendors, were arrested last week in Luengue-Luiana National Park, Cuando Cubango province. jornaldeangola.sapo.ao/provincias/desmantelada-rede-de-caca-furtiva-e-passadores-de-armas?fbclid=IwAR34siY1W8LVKBKs-xJPGWRuiejZh2k… 1/2 27/07/2020 Dismantled poaching net and weapon snipers | Provinces | Jornal de Angola - Online Approximately 300 young people were recruited in various locations to reinforce inspection in the two national parks Photo: Edições Novembro According to the director of the Provincial Environment Office, Júlio Bravo, among the detainees, seven were dedicated to the slaughter of animals of various species, two supplied firearms and ammunition and two ladies were in charge of the sale of meat. The alleged criminals, detained during a joint operation between National Police officers and environmental inspectors deployed in Luengue-Luiana Park, had two mauser weapons in their possession, a PKM machine gun, a shotgun, 91 ammunition and 200 kilograms of animal meat. slaughtered. Júlio Bravo, who headed a multisectoral commission, which worked for two weeks in the municipalities of Mavinga, Rivungo, Dirico and Cuangar, announced that during the tour in these regions 300 young people were selected who live near the national parks of Mavinga and Luengue- Luiana to strengthen the brigades of environmental inspectors. The official informed that the selected young people will be trained at the Environmental Inspector Training Institute “31 de Janeiro ”, based in the city of Menongue, after the constraints caused by the pandemic ended. -

Yellow Fever Outbreak in Angola, 01 September 2016
YELLOW FEVER OUTBREAK WEEKLY SITUATION REPORT, INCIDENT MANAGEMENT TEAM—ANGOLA YELLOW FEVER OUTBREAK IN ANGOLA INCIDENT MANAGEMENT Vol: 8-03 SITUATION REPORT W35, 01 September 2016 I. Key Highlights A total of 2,807,628 (94 %) individuals 6 months and above have been vaccinated in the 22 most recently vaccinated districts as of 01 September 2016, 15 districts out of 22 achieved 90% or more of vaccination coverage. 4 districts achieved between 80-90%. Three districts did not reach 80% coverage and the vaccination campaign was extended there for another one week : Dirico, Namacunde and Sumbe in Currently the IM System is supporting the Ministry of Health in the preparation of the upcoming campaign in 21 districts in 12 provinces. The total population targeted in this new phase is 3,189,392 and requires 3,986,019 doses of vaccines. Is expected the arrival of 1.98 M doses from the last request approved by ICG. The ICG did not communicate yet the date of shipment but is already on process. The preparation of the coverage survey is ongoing. Table 1: National Summary of Yellow Fever Outbreak II. Epidemiological Situation as of 01 September 2016 Yellow Fever Outbreak Summary 26 Aug — 01 Sep 2016, (W35) Reported cases 24 Samples tested 24 Week 35 statistics (26 August to 1 September 2016): Confirmed cases 0 Of 24 suspected cases reported, all of them were tested by the National Total Deaths 1 Laboratory. None of them was positive for yellow fever Total provinces that reported cases 8 One(1) death was reported among the suspected cases during this period. -

Inventário Florestal Nacional, Guia De Campo Para Recolha De Dados
Monitorização e Avaliação de Recursos Florestais Nacionais de Angola Inventário Florestal Nacional Guia de campo para recolha de dados . NFMA Working Paper No 41/P– Rome, Luanda 2009 Monitorização e Avaliação de Recursos Florestais Nacionais As florestas são essenciais para o bem-estar da humanidade. Constitui as fundações para a vida sobre a terra através de funções ecológicas, a regulação do clima e recursos hídricos e servem como habitat para plantas e animais. As florestas também fornecem uma vasta gama de bens essenciais, tais como madeira, comida, forragem, medicamentos e também, oportunidades para lazer, renovação espiritual e outros serviços. Hoje em dia, as florestas sofrem pressões devido ao aumento de procura de produtos e serviços com base na terra, o que resulta frequentemente na degradação ou transformação da floresta em formas insustentáveis de utilização da terra. Quando as florestas são perdidas ou severamente degradadas. A sua capacidade de funcionar como reguladores do ambiente também se perde. O resultado é o aumento de perigo de inundações e erosão, a redução na fertilidade do solo e o desaparecimento de plantas e animais. Como resultado, o fornecimento sustentável de bens e serviços das florestas é posto em perigo. Como resposta do aumento de procura de informações fiáveis sobre os recursos de florestas e árvores tanto ao nível nacional como Internacional l, a FAO iniciou uma actividade para dar apoio à monitorização e avaliação de recursos florestais nationais (MANF). O apoio à MANF inclui uma abordagem harmonizada da MANF, a gestão de informação, sistemas de notificação de dados e o apoio à análise do impacto das políticas no processo nacional de tomada de decisão. -
Evaluation of Norweegian Refugee Councils Distribution and Food Security Programmes - Southern Angola 1997-2007
T R O P E R E T E L P M O C NORWEGIAN REFUGEE COUNCIL EVALUATION REPORT EVALUATION OF NORWEEGIAN REFUGEE COUNCILS DISTRIBUTION AND FOOD SECURITY PROGRAMMES - SOUTHERN ANGOLA 1997-2007 DISTRIBUTION AND FOOD SECURITY PROGRAMME IN ANGOLA BY CHRISTIAN LARSSEN JUNE 2008 Evaluation of Norwegian Refugee Council Distribution Programmes – Southern Angola, 1999-2007 FINAL REPORT 12 March 2008 Evaluator Christian Larssen Evaluation of NRC Distribution Programme – Angola Page 1 of 53 Content Executive Summary 3 Map of Angola 5 1. Project Description and Summary of Activities 6 2. Evaluation of project impact, effectiveness and efficiency 20 3. Evaluation of project sustainability 27 4. Conclusions, Lessons Learned and Recommendations 31 5. Evaluation purpose, scope and methodology 35 Annexes: A. Distribution Tables, NRC-Angola 2002-2007 B. Evaluation team and Programme C. Terms of Reference D. List of meetings/people contacted E. List of documents used F. Glossary and Abbreviations G. UN OCHA Access Map for Angola 2002 and 2003 The observations, conclusions and recommendations contained in this report are the exclusive responsibility of the evaluator/consultant, meaning that they do not necessarily reflect the views of the Norwegian Refugee Council or its staff Evaluation of NRC Distribution Programme – Angola Page 2 of 53 Executive Summary 1. Project Description and Summary of Project Activities Towards the end of the 1990’s, when the people had to flee their villages for Matala, through the emergency phase in the reception centres, NRC in collaboration with WFP and FAO provided necessary food-aid and essential distribution of non-food items. The IDPs also received support for subsistence farming and reconstruction of schools and health-post, providing education and basic health care in the centres. -

EPSMO-BIOKAVANGO Okavango River Basin Environmental Flow Assessment Hydrology Report: Data and Models Report No: 05/2009
E-Flows Hydrology Report: Data and models EPSMO-BIOKAVANGO Okavango River Basin Environmental Flow Assessment Hydrology Report: Data and Models Report No: 05/2009 H. Beuster, et al. April 2010 1 E-Flows Hydrology Report: Data and models DOCUMENT DETAILS PROJECT Environment protection and sustainable management of the Okavango River Basin: Preliminary Environmental Flows Assessment TITLE: Hydrology Report: Data and models DATE: June 2009 LEAD AUTHORS: H. Beuster REPORT NO.: 05/2009 PROJECT NO: UNTS/RAF/010/GEF FORMAT: MSWord and PDF. CONTRIBUTING AUTHORS: K Dikgola, A N Hatutale, M Katjimune, N Kurugundla, D Mazvimavi, P E Mendes, G L Miguel, A C Mostert, M G Quintino, P N Shidute, F Tibe, P Wolski .THE TEAM Project Managers Celeste Espach Keta Mosepele Chaminda Rajapakse Aune-Lea Hatutale Piotr Wolski Nkobi Moleele Mathews Katjimune Geofrey Khwarae assisted by Penehafo EFA Process Shidute Management Angola Andre Mostert Jackie King Manual Quintino (Team Shishani Nakanwe Cate Brown Leader and OBSC Cynthia Ortmann Hans Beuster member) Mark Paxton Jon Barnes Carlos Andrade Kevin Roberts Alison Joubert Helder André de Andrade Ben van de Waal Mark Rountree e Sousa Dorothy Wamunyima Amândio Gomes assisted by Okavango Basin Steering Filomena Livramento Ndinomwaameni Nashipili Committee Paulo Emilio Mendes Tracy Molefi-Mbui Gabriel Luis Miguel Botswana Laura Namene Miguel Morais Casper Bonyongo (Team Mario João Pereira Leader) Rute Saraiva Pete Hancock Carmen Santos Lapologang Magole Wellington Masamba Namibia Hilary Masundire Shirley Bethune