United States Patent (19) 20
Total Page:16
File Type:pdf, Size:1020Kb

Load more
Recommended publications
-

(CD-P-PH/PHO) Report Classification/Justifica
COMMITTEE OF EXPERTS ON THE CLASSIFICATION OF MEDICINES AS REGARDS THEIR SUPPLY (CD-P-PH/PHO) Report classification/justification of medicines belonging to the ATC group D07A (Corticosteroids, Plain) Table of Contents Page INTRODUCTION 4 DISCLAIMER 6 GLOSSARY OF TERMS USED IN THIS DOCUMENT 7 ACTIVE SUBSTANCES Methylprednisolone (ATC: D07AA01) 8 Hydrocortisone (ATC: D07AA02) 9 Prednisolone (ATC: D07AA03) 11 Clobetasone (ATC: D07AB01) 13 Hydrocortisone butyrate (ATC: D07AB02) 16 Flumetasone (ATC: D07AB03) 18 Fluocortin (ATC: D07AB04) 21 Fluperolone (ATC: D07AB05) 22 Fluorometholone (ATC: D07AB06) 23 Fluprednidene (ATC: D07AB07) 24 Desonide (ATC: D07AB08) 25 Triamcinolone (ATC: D07AB09) 27 Alclometasone (ATC: D07AB10) 29 Hydrocortisone buteprate (ATC: D07AB11) 31 Dexamethasone (ATC: D07AB19) 32 Clocortolone (ATC: D07AB21) 34 Combinations of Corticosteroids (ATC: D07AB30) 35 Betamethasone (ATC: D07AC01) 36 Fluclorolone (ATC: D07AC02) 39 Desoximetasone (ATC: D07AC03) 40 Fluocinolone Acetonide (ATC: D07AC04) 43 Fluocortolone (ATC: D07AC05) 46 2 Diflucortolone (ATC: D07AC06) 47 Fludroxycortide (ATC: D07AC07) 50 Fluocinonide (ATC: D07AC08) 51 Budesonide (ATC: D07AC09) 54 Diflorasone (ATC: D07AC10) 55 Amcinonide (ATC: D07AC11) 56 Halometasone (ATC: D07AC12) 57 Mometasone (ATC: D07AC13) 58 Methylprednisolone Aceponate (ATC: D07AC14) 62 Beclometasone (ATC: D07AC15) 65 Hydrocortisone Aceponate (ATC: D07AC16) 68 Fluticasone (ATC: D07AC17) 69 Prednicarbate (ATC: D07AC18) 73 Difluprednate (ATC: D07AC19) 76 Ulobetasol (ATC: D07AC21) 77 Clobetasol (ATC: D07AD01) 78 Halcinonide (ATC: D07AD02) 81 LIST OF AUTHORS 82 3 INTRODUCTION The availability of medicines with or without a medical prescription has implications on patient safety, accessibility of medicines to patients and responsible management of healthcare expenditure. The decision on prescription status and related supply conditions is a core competency of national health authorities. -

Steroids Topical
Steroids, Topical Therapeutic Class Review (TCR) September 18, 2020 No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, digital scanning, or via any information storage or retrieval system without the express written consent of Magellan Rx Management. All requests for permission should be mailed to: Magellan Rx Management Attention: Legal Department 6950 Columbia Gateway Drive Columbia, Maryland 21046 The materials contained herein represent the opinions of the collective authors and editors and should not be construed to be the official representation of any professional organization or group, any state Pharmacy and Therapeutics committee, any state Medicaid Agency, or any other clinical committee. This material is not intended to be relied upon as medical advice for specific medical cases and nothing contained herein should be relied upon by any patient, medical professional or layperson seeking information about a specific course of treatment for a specific medical condition. All readers of this material are responsible for independently obtaining medical advice and guidance from their own physician and/or other medical professional in regard to the best course of treatment for their specific medical condition. This publication, inclusive of all forms contained herein, is intended to be educational in nature and is intended to be used for informational purposes only. Send comments and suggestions to [email protected]. September -

Formulary Updates Effective January 1, 2021
Formulary Updates Effective January 1, 2021 Dear Valued Client, Please see the following lists of formulary updates that will apply to the HometownRx Formulary effective January 1 st , 2021. As the competition among clinically similar products increases, our formulary strategy enables us to prefer safe, proven medication alternatives and lower costs without negatively impacting member choice or access. Please note: Not all drugs listed may be covered under your prescription drug benefit. Certain drugs may have specific restrictions or special copay requirements depending on your plan. The formulary alternatives listed are examples of selected alternatives that are on the formulary. Other alternatives may be available. Members on a medication that will no longer be covered may want to talk to their healthcare providers about other options. Medications that do not have alternatives will be available at 100% member coinsurance . Preferred to Non -Preferred Tier Drug Disease State /Drug Class Preferred Alternatives ALREX Eye inflammation loteprednol (generic for LOTEMAX) APRISO 1 Gastrointestinal agent mesalamine (generic for APRISO) BEPREVE Eye allergies azelastine (generic for OPTIVAR) CIPRODEX 1 Ear inflammation ciprofloxacin-dexamethasone (generic for CIPRODEX) COLCRYS 1 Gout colchicine (generic for COLCRYS) FIRST -LANSOPRAZOLE Gastrointestinal agent Over-the-counter lansoprazole without a prescription FIRST -MOUTHWASH BLM Mouth inflammation lidocaine 2% viscous solution (XYLOCAINE) LOTEMAX 1 Eye inflammation loteprednol etabonate (generic -
HALOG® SOLUTION (Halcinonide Topical Solution, USP) 0.1 %
4.5" FRONT HALOG® SOLUTION 0.75" (Halcinonide Topical Solution, USP) 0.1 % For Topical Use Only. Not For Ophthalmic Use. Rx Only PPK-8860-0 29 DESCRIPTION Laboratory Tests The topical corticosteroids constitute a class of primarily synthetic steroids used as A urinary free cortisol test and ACTH stimulation test may be helpful in evaluating HPA anti-inflammatory and antipruritic agents. The steroids in this class include halcinonide. axis suppression. Halcinonide is designated chemically as 21-Chloro-9-fluoro-11β,16α, 17-trihydroxypregn- 4-ene-3,20-dione cyclic 16,17-acetal with acetone. Structural formula: Carcinogenesis, Mutagenesis, and Impairment of Fertility Long-term animal studies have not been performed to evaluate the carcinogenic potential or the effect on fertility of topical corticosteroids. Studies to determine mutagenicity with prednisolone and hydrocortisone showed negative results. Pregnancy Teratogenic Effects Corticosteroids are generally teratogenic in laboratory animals when administered systemically at relatively low dosage levels. The more potent corticosteroids have been C24H32ClFO5, MW 454.96, CAS-3093-35-4 shown to be teratogenic after dermal application in laboratory animals. There are no Each mL of 0.1% HALOG SOLUTION (Halcinonide Topical Solution, USP) contains 1 mg adequate and well-controlled studies in pregnant women on teratogenic effects from halcinonide, edetate disodium, polyethylene glycol 300, and purified water with butylated topically applied corticosteroids. Therefore, topical corticosteroids should be used during hydroxytoluene as an antioxidant. pregnancy only if the potential benefit justifies the potential risk to the fetus. Drugs of this class should not be used extensively on pregnant patients, in large amounts, or for CLINICAL PHARMACOLOGY prolonged periods of time. -
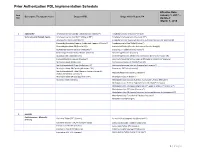
Prior Authorization PDL Implementation Schedule
Prior Authorization PDL Implementation Schedule Effective Date: Item January 1, 2017 – Descriptive Therapeutic Class Drugs on PDL Drugs which Require PA Nbr Updated: March 1, 2018 1 ADD/ADHD Amphetamine Salt Combo Tablet ( Generic Adderall®) Amphetamine ODT (Adzenys® XR ODT) Stimulants and Related Agents Amphetamine Salt Combo ER (Adderall XR®) Amphetamine Suspension (Dyanavel XR®) Atomoxetine Capsule (Strattera®) Amphetamine Salt Combo ER (Generic; Authorized Generic for Adderall XR) Dexmethylphenidate (Generic; Authorized Generic of Focalin®) Amphetamine Sulfate Tablet (Evekeo®) Dexmethylphenidate ER (Focalin XR®) Armodafinil Tablet (Generic; Authorized Generic; Nuvigil®) Dextroamphetamine Solution (Procentra®) Clonidine ER Tablet (Generic; Kapvay®) Dextroamphetamine Sulfate Tablet (Generic) Dexmethylphenidate (Focalin®) Guanfacine ER Tablet (Generic) Dexmethylphenidate XR (Generic; Authorized Generic for Focalin XR) Lisdexamfetamine Capsule (Vyvanse®) Dextroamphetamine Sulfate Capsule ER (Generic; Dexedrine®Spansule) Methylphenidate IR (Generic) Dextroamphetamine IR Tablet (Zenzedi®) Methylphenidate ER Chew (Quillichew ER®) Dextroamphetamine Solution (Generic for Procentra®) Methylphenidate ER Capsule (Metadate CD®) Guanfacine ER Tablet (Intuniv®) Methylphenidate ER Tablet (Generic; Generic Concerta®; Methamphetamine (Generic; Desoxyn®) Authorized Generic Concerta®) Methylphenidate ER Susp (Quillivant XR®) Methylphenidate IR (Ritalin®) Modafinil Tablet (Generic) Methylphenidate Solution (Generic; Authorized Generic; Methylin®) Methylphenidate -

Wo 2008/127291 A2
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (43) International Publication Date PCT (10) International Publication Number 23 October 2008 (23.10.2008) WO 2008/127291 A2 (51) International Patent Classification: Jeffrey, J. [US/US]; 106 Glenview Drive, Los Alamos, GOlN 33/53 (2006.01) GOlN 33/68 (2006.01) NM 87544 (US). HARRIS, Michael, N. [US/US]; 295 GOlN 21/76 (2006.01) GOlN 23/223 (2006.01) Kilby Avenue, Los Alamos, NM 87544 (US). BURRELL, Anthony, K. [NZ/US]; 2431 Canyon Glen, Los Alamos, (21) International Application Number: NM 87544 (US). PCT/US2007/021888 (74) Agents: COTTRELL, Bruce, H. et al.; Los Alamos (22) International Filing Date: 10 October 2007 (10.10.2007) National Laboratory, LGTP, MS A187, Los Alamos, NM 87545 (US). (25) Filing Language: English (81) Designated States (unless otherwise indicated, for every (26) Publication Language: English kind of national protection available): AE, AG, AL, AM, AT,AU, AZ, BA, BB, BG, BH, BR, BW, BY,BZ, CA, CH, (30) Priority Data: CN, CO, CR, CU, CZ, DE, DK, DM, DO, DZ, EC, EE, EG, 60/850,594 10 October 2006 (10.10.2006) US ES, FI, GB, GD, GE, GH, GM, GT, HN, HR, HU, ID, IL, IN, IS, JP, KE, KG, KM, KN, KP, KR, KZ, LA, LC, LK, (71) Applicants (for all designated States except US): LOS LR, LS, LT, LU, LY,MA, MD, ME, MG, MK, MN, MW, ALAMOS NATIONAL SECURITY,LLC [US/US]; Los MX, MY, MZ, NA, NG, NI, NO, NZ, OM, PG, PH, PL, Alamos National Laboratory, Lc/ip, Ms A187, Los Alamos, PT, RO, RS, RU, SC, SD, SE, SG, SK, SL, SM, SV, SY, NM 87545 (US). -

List of Formulary Drug Removals
July 2021 Formulary Drug Removals Below is a list of medicines by drug class that have been removed from your plan’s formulary. If you continue using one of the drugs listed below and identified as a Formulary Drug Removal, you may be required to pay the full cost. If you are currently using one of the formulary drug removals, ask your doctor to choose one of the generic or brand formulary options listed below. Category Formulary Drug Formulary Options Drug Class Removals Acromegaly SANDOSTATIN LAR SOMATULINE DEPOT SIGNIFOR LAR SOMAVERT Allergies dexchlorpheniramine levocetirizine Antihistamines Diphen Elixir RyClora CARBINOXAMINE TABLET 6 MG Allergies BECONASE AQ flunisolide spray, fluticasone spray, mometasone spray, DYMISTA Nasal Steroids / Combinations OMNARIS QNASL ZETONNA Anticonvulsants topiramate ext-rel capsule carbamazepine, carbamazepine ext-rel, clobazam, divalproex sodium, (generics for QUDEXY XR only) divalproex sodium ext-rel, gabapentin, lamotrigine, lamotrigine ext-rel, levetiracetam, levetiracetam ext-rel, oxcarbazepine, phenobarbital, phenytoin, phenytoin sodium extended, primidone, rufinamide, tiagabine, topiramate, valproic acid, zonisamide, FYCOMPA, OXTELLAR XR, TROKENDI XR, VIMPAT, XCOPRI BANZEL SUSPENSION clobazam, lamotrigine, rufinamide, topiramate, TROKENDI XR ONFI SABRIL vigabatrin ZONEGRAN carbamazepine, carbamazepine ext-rel, divalproex sodium, divalproex sodium ext-rel, gabapentin, lamotrigine, lamotrigine ext-rel, levetiracetam, levetiracetam ext-rel, oxcarbazepine, phenobarbital, phenytoin, phenytoin sodium -

Bryhali (Halobetasol Propionate)
UnitedHealthcare Pharmacy Clinical Pharmacy Programs Program Number 2021 P 3033-10 Program Step Therapy – Topical Steroids Medication Topical Steroids: Cordran (flurandrenolide) cream 0.05%, Cordran (flurandrenolide) lotion 0.05%, Cordran (flurandrenolide) ointment 0.05%, Cloderm (clocortolone pivalate) cream 0.1%, Halog (halcinonide) cream 0.1%, Halog (halcinonide) ointment 0.1%, Desonate (desonide gel) gel 0.05% Cultivate lotion (fluticasone propionate 0.05% lotion), Ultravate (halobetasol propionate) lotion 0.05%, Bryhali (halobetasol propionate) lotion 0.01% P&T Approval Date 8/2014, 7/2015, 10/2015, 3/2016, 1/2017, 2/2018, 2/2019, 3/2020, 6/2021 Effective Date 9/1/2021; Oxford only: 9/1/2021 1. Background: Topical steroids are commonly prescribed for the treatment of rash, eczema, and dermatitis. Topical steroids have anti-inflammatory properties, and are classified into different potency classes based on their vasoconstriction abilities. A vasoconstriction bioassay provides potency measurements that correlate with clinical potency. There are numerous topical steroid products. Step Therapy programs are utilized to encourage the use of lower cost alternatives for certain therapeutic classes. This program requires a member to try one or two lower cost alternative topical steroids before providing coverage for higher cost topical steroids. Generic equivalent medications for brands listed as a step 2 agent will also be targeted when available. Class 1: Super Potent Class 5: Lower Mid-Strength Class 2: Potent Class 6: Mild Class 3: Upper Mid- Strength Class 7: Least Potent Class 4:Mid-Strength © 2021 UnitedHealthcare Services Inc. 1 2. Coverage Criteria a: A. Topical steroids will be approved based on the following criterion: 1. -

Hydrocortisone-17-Butyrate
HYDROCORTISONE-17-BUTYRATE Your T.R.U.E. TEST results indicate that you have a contact allergy to hydrocortisone- WHAT SHOULD YOU LOOK FOR AND AVOID? 17-butyrate. This contact allergy may cause your skin to react when it is exposed Avoid products with the following names in the list of ingredients: to this substance, although it may take several days for the symptoms to appear. Typical symptoms include redness, swelling, itching and fluid-filled blisters. • h.17b • Laticort • locoid • hb(sub17) Hydrocortisone-17-butyrate is a mid-potent (Group D2) corticosteroid used in both prescription and nonprescription topical ointments, creams, tablets, or injection, to • Alfason • Cortisol 17-butyrate treat inflammatory skin diseases and psoriasis. Corticosteroid contact allergy may • Plancol • Hydrocortisone 17-butyrate by difficult to diagnose. Failure to improve when treated with corticosteroids can be • Hydrocortisone butyrate a symptom of contact allergy. You also may react to products such as: WHERE IS HYDROCORTISONE-17-BUTYRATE FOUND? • Amcinonide • Budesonide At work, you may find hydrocortisone-17-butyrate in or around: • Cloprednol • Cortifoam cortisol • Medicaments • Cortril • Desonide • Creams, lotions, ointments and powders • Efcorlin • Efcortelin • Elcorbin • Fludrocortisone acetate At home, you may find hydrocortisone-17-butyrate in or around: • Fluocinolone acetonide • Fluocinonide • Anti-inflammatory agents found in both prescription and nonprescription • Flurandrenolide • Halcinonide medications • Hydrocortisone • Hydrocortisone -

Preferred Drug List Drug Class Review Announcement
PDL Drug Class Review Announcement January 12, 2021 Drug Classes to be reviewed: Anti-Parkinson’s Agents; Calcitonin-Gene Receptor Protein (CGRP) Inhibitors; Atypical Antipsychotics – Oral; Anxiolytics; Bile salts; Cardiovascular – Alpha-Blockers, Beta-Blockers & Combinations, Calcium Channel Blockers; Diabetes Management – Insulins; Glucagon, Self-Administered; Growth Hormones; Hemorrhoidal, Anorectal and Related Topical Anesthetic Agents; Immune Globulins; Intranasal Rhinitis Agents; Leukotriene Modifiers; Lipotropics – Statins, Statin Combinations, Other; Lithium Agents; Multiple Sclerosis Agents; Neurocognitive Disorder Agents; Ophthalmics - Allergy Agents, Anti-Inflammatory Agents, Glaucoma Agents; Sedative/Hypnotics - Non-Benzodiazepine, Benzodiazepine; and Topical Steroids – Low, Medium, High, Very High Potency. These drug classes will be reviewed at the January 12, 2021 P&T Committee meeting from 1-5pm. The meeting will be held virtually. Dossiers and Supplemental Rebate offers are due to Magellan by December 8, 2020. Please provide your public comments to Jessica Czechowski, Clinical Account Manager ([email protected]) no later than January 5, 2021 to ensure they are included in the information supplied to the P&T Committee members. Please carbon copy Brittany Schock, PDL Pharmacist ([email protected]) on all clinical information and public comment submissions. Anti-Parkinson’s Agents Brand Name Generic Name Dopa Decarboxylase Inhibitors Carbidopa/Levodopa ER tablet, ODT Duopa Carbidopa/Levodopa enteral -

(12) Patent Application Publication (10) Pub. No.: US 2014/0234227 A1 Yelin Et Al
US 20140234227A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2014/0234227 A1 Yelin et al. (43) Pub. Date: Aug. 21, 2014 (54) FOAM FORMULATIONS Publication Classification (71) Applicant: OTIC PHARMA LTD, Rehovot (IL) (51) Int. C. A 6LX3/573 (2006.01) (72) Inventors: Rodrigo Yelin, Kfar Yona (IL); Jorge 469/12 (2006.01) Danziger, Rishon LeZion (IL); Eran A613 L/496 (2006.01) Eilat, Herzliya (IL) (52) U.S. C. CPC ............. A6 IK3I/573 (2013.01); A61 K3I/496 (73) Assignee: OTIC PHARMA LTD., Rehovot (IL) (2013.01); A61 K9/122 (2013.01) USPC ............................................................ 424/43 (21) Appl. No.: 14/350,948 (22) PCT Fled: Oct. 10, 2012 (57) ABSTRACT (86) PCT NO.: PCT/L2012/OSO4O1 The present invention provides foamable pharmaceutical compositions comprising water-soluble antibiotics and anti S371 (c)(1), inflammatory steroids and methods of preparing same. Par (2), (4) Date: Apr. 10, 2014 ticularly, the present invention relates to oil-free pharmaceu tical compositions comprising a quinolone, an anti Related U.S. Application Data inflammatory Steroid, a polar co-solvent, and propellant gas, (60) Provisional application No. 61/545.209, filed on Oct. administered to the ear in the form of foam for treating ear 10, 2011. disorders. US 2014/0234227 A1 Aug. 21, 2014 FOAM FORMULATIONS propyl-6-fluoro-1,4-dihydro-4-oxo-7-(1-piperazinyl)-3- quinolinecarboxylic acid with the following chemical struc FIELD OF THE INVENTION ture: 0001. The present invention relates to foamable pharma ceutical compositions comprising water-soluble antibiotics together with anti-inflammatory steroids and methods of pre F COOH paring same. -

Texas Children's Hospital Dermatology Service PCP Referral Guidelines- Psoriasis
Texas Children's Hospital Dermatology Service PCP Referral Guidelines- Psoriasis Diagnosis: PSORIASIS TREATMENT RECOMMENDATIONS: • Careful physical exam for possible strep infection (throat, perianal area, inguinal folds) and treatment if positive. • Careful history for persistent or frequent history of morning stiffness or joint pain Location Eyelids Elidel 1% cream (or other calcineurin inhibitor) Face, Axillae, Hydrocortisone 2.5% ointment (or other Class 6 or 7 topical steroid) Inguinal Folds Body Thin/mild: Triamcinolone 0.1% ointment (or other Class 3, 4 topical steroid) Thick/severe: Mometasone 0.1% ointment (or other Class 1 or 2 topical steroid) Scalp Mild (or patients with dry hair): Fluocinolone 0.01% (Derma-smoothe) oil Severe: Clobetasol 0.05 % solution Shampoo: (over-the-counter) • Salicylic acid containing shampoo (e.g. T sal shampoo) • Tar containing shampoo (e.g. T gel shampoo) • Baker’s P&S shampoo Nails Mometasone 0.1% ointment (or other Class 1 or 2 topical steroid) • Apply medication to nail folds/cuticle PATIENT RESOURCES: National Psoriasis Foundation www.psoriasis.org REFERRAL RECOMMENDATIONS: • Please refer patient if there is extensive involvement (>5-10% BSA), or localiZed involvement that has failed treatment recommendations above. • If patient has persistent morning stiffness or joint complaints, please also refer to rheumatology for evaluation for possible psoriatic arthritis Educational recommendations are made from the best evidence, expert opinions and consideration for the patients and families cared for by the service. This is NOT intended to impose standards of care preventing selective variation in practice that are necessary to meet the unique needs of individual patients. The physician must consider each patient’s circumstance to make the ultimate judgment regarding best care.