Guildford and Waverley CCG
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Fairlands Practice the Fairlands Practice Is a Partnership of Seven Doctors with a Complement of Nurses
The Fairlands Practice Dr Kerry Angiolini ➢ Chronic Disease management clinics for diabetes, asthma, high www.fairlands.co.uk MB BS. MRCGP. Southampton 2007 blood pressure and chest conditions ➢ Minor Surgery and cryotherapy Salaried GP’s ➢ Travel advice and vaccinations ➢ Smoking cessation advisors Dr Alexandra Standring MB BS. MRCGP. DFFP ➢ Seasonal flu vaccinations Bristol 1990 ➢ Emergency contraception, contraception implants Dr Caty Taussig Privately offered services MB BS. MRCGP 1996, Diploma of Geriatric Medicine 1996 ➢ Osteopathy & cranial osteopathy Dr Fiona Chadd ➢ Physiotherapy MB BSMRCGP, Guildford 2015 ➢ Acupuncture ➢ Chiropody Dr James Edmeades ➢ Counselling Nurse Practitioners Please see our website for more information on all of these services at www.fairlands.co.uk Natasha Wasum The Fairlands Practice is a partnership of seven doctors with a Michelle Carter Out of hours services complement of nurses, health visitors and other health professionals practicing from the main premises on the Fairlands estate in Practice Manager/Business Development Manager Outside normal working hours there are several ways of receiving Worplesdon, near Guildford and a branch surgery in the nearby village medical help: of Normandy. Isata Green Care UK – can give medical advice and may be contacted 24 hours a The surgeries are modern purpose built medical centres offering both Nurses day on: 111 NHS and private services. The branch surgery at Glaziers Lane also has a dispensary. All of our consulting rooms are on the ground floor Carol Corning Lead Nurse Walk-in centres (staffed by nurses for all medical needs of the over and the surgeries provide baby changing and disabled facilities. Debbie Garland Practice Nurse 2’s) Jane Graham Practice Nurse We are a GP training practice and have GP registrars in their final year Rebecca Phoenix Practice Nurse ➢ Woking Community Hospital, Heathside Road, Woking GU22 of training with us. -

Guildford Borough Mapset
from from from WOKING LONDON WOKING A247 A3 A322 Pitch Place Jacobswell A247 A320 GUILDFORD WEST Bellfields ey BOROUGH Slyfield r W CLANDON ve APPROACH MAP Green Ri Abbots- Stoughton wood A3 Burpham A3100 N A323 Bushy Hill from A25 Park A25 LEATHERHEAD Barn Merrow A25 A322 A25 SURREY H UNIVERSITY A320 GUILDFORD CATHEDRAL Guildford A246 Park Onslow A3 Village GUILDFORD A31 DORKING from HOGS BACK from D O W N S FARNHAM A31 T H O R N A281 A3 ARTINGTON A248 LITTLETON A3100 CHILWORTH SHALFORD ALBURY LOSELEY COMPTON HOUSE A248 B3000 from from from PORTSMOUTH MILFORD HORSHAM PRODUCED BY BUSINESS MAPS LTD FROM DIGITAL DATA - COPYRIGHT BARTHOLOMEW(1996) TEL: 01483 422766 FAX: 01483 422747 M25 Pibright Bisley Camp GUILDFORD Camp BOROUGH MAP B367 OCKHAM B3012 SEND EFFINGHAM Pirbright B368 JUNCTION B2215 B2039 B3032 WORPLESDON A247 B380 EAST NORTH CAMP Worplesdon A3 HORSLEY ASH VALE Jacobswell A247 Common WEST EFFINGHAM Ash Vale A322 WEST A324 CLANDON HORSLEY Slyfield A323 EAST A246 A246 AshCommon Fairlands Green Burpham CLANDON CLANDON Wood Street A323 A320 A321 Village B2234 ASH Wyke Merrow A25 Park Barn A25 ASH WANBOROUGH B3009 AshGreen Onslow Village Wanborough TONGHAM Chantries HOGS BACK A25 A31 A281 Chilworth ALBURY GOMSHALL Littleton A3100 Seale PUTTENHAM B3000 A248 COMPTON SHERE from The DORKING Sands CHILWORTH B3000 B2128 Brook Sutton A3 Farley Abinger Green PEASLAKE Eashing N HOLMBURY ST MARY B2126 BOROUGH BOUNDARY from OCKLEY PRODUCED BY BUSINESS MAPS LTD FROM DIGITAL DATA - COPYRIGHT BARTHOLOMEW(1996) BUSINESS MAPS LTD TEL: 01483 422766 -

Complaints Procedure
What to do if you are dissatisfied with the Outcome of your complaint If however you are ultimately not happy with how we have dealt with your complaint, and would like to take the matter further, you can contact the You may approach Health Watch Surrey for help Parliamentary and Health Service Ombudsman or advice; who make final decisions on unresolved Healthwatch Surrey provide confidential advice and complaints about the NHS in England. It is an support, helping you to sort out any concerns you may independent service which is free for everyone to have about the care we provide and guiding you use. through the different services available from the NHS. Please find below contact details for Healthwatch Contact Details of the Ombudsman: Surrey: Complaints The Parliamentary and Health Service Ombudsman Health Watch Surrey Millbank Tower The Annexe Procedure Millbank Lockwood Day Centre London Westfield Road Guildford SW1P 4QP The Fairlands Medical Centre GU1 1RR Tel: 0345 015 4033 Fairlands Avenue Tel: 0303 303 0023 Website: www.ombudsman.org.uk/make –a-complaint Worplesdon Guildford Email: [email protected] Surrey, GU3 3NA Tel: 01483 594250 You can also seek advice and support about making an NHS complaint from the Independent Health Advocacy Service, Surrey Independent Living Council Glaziers Lane Branch Surgery 19 Glaziers Lane Telephone: 01483 310 500 Normandy Surrey, GU3 2DD Text: 07704 265 377 Responsible Person for Complaints Tel: 01483 813274 Email: [email protected] Dr Christopher Lukaszewicz Post: Surrey Independent Living Council (SILC) Astolat Complaint Managers Coniers Way Please also see Guildford Dr Christopher Lukaszewicz (Clinical) separate Surrey Complaint Form GU4 7HL Mrs Isata Green (non-clinical) available at Reception Making a Complaint What We Do Next Complaining on Behalf of Someone Else and Sharing of Data We aim to settle complaints as soon as possible. -

Latest News from the Team
www.fairlands.co.uk Email: [email protected] Practice Newsletter – SPRING/SUMMER 2019 Latest News from the Team Practice Updates Dr Fiona Chadd will be on maternity and annual leave from mid-June 2019 to 2nd week of June 2020. Dr Sukrti Nagpal left the Practice in February 2019. We are in the process of recruiting a new GP to take over her list of patients and aim to have someone in place by July 2019. In the meantime the partners will share workload for Dr Nagpal’s list of patients. We would like to welcome 2 new receptionists to the surgery, Tracy Edwards and Chloe Brown. Primary Care Networks A key part of the NHS long-term plan is Primary Care Networks (PCN); these PCN’s will bring general practices together to work at scale. This is for a range of reasons including: staff recruitment, to provide a wider range of services and to more easily integrate the wider health and care system. All practices are expected to come together in geographical networks covering populations of approximately 30-50,000 patients by June 2019. PCN’s will eventually be required to deliver a set of seven national service specifications. Five will start by April 2020: structured medication reviews, enhanced health in care homes, anticipatory care (with community services), personalised care and supporting early cancer diagnosis. The remaining two will start by 2021: cardiovascular disease case-finding and locally agreed action to tackle inequalities. In order to do this they will be expected to provide a wider range of primary care services to patients, for example first contact physiotherapy, extended access and social prescribing. -

The Fairlands Practice
The Fairlands Practice Privately offered services www.fairlands.co.uk Dr Caty Taussig MB BS. MRCGP 1996, Diploma of Geriatric Medicine 1996 ➢ Osteopathy & cranial osteopathy ➢ Physiotherapy Dr Fiona Chadd ➢ Acupuncture MB BSMRCGP, Guildford 2015 ➢ Chiropody ➢ Counselling Dr James Edmeades Please see our website for more information on all of these services at Nurse Practitioners www.fairlands.co.uk Natasha Wasum Out of hours services Sally Collins Outside normal working hours there are several ways of receiving medical Practice Manager/Business Development Manager help: Isata Green Care UK – can give medical advice and may be contacted 24 hours a day on: 111 The Fairlands Practice is a partnership of seven doctors with a Nurses complement of nurses, health visitors and other health professionals Walk-in centres (staffed by nurses for all medical needs of the over 2’s) practicing from the main premises on the Fairlands estate in Worplesdon, Jane Graham Lead Nurse near Guildford and a branch surgery in the nearby village of Normandy. Rebecca Phoenix Lead Nurse ➢ Woking Community Hospital, Heathside Road, Woking GU22 7HS Debbie Garland Practice Nurse 01483 846209 Mon-Friday (7am -7:30pm) weekends & Bank The surgeries are modern purpose built medical centres offering both NHS Carol Corning Practice Nurse Holidays 9am-7pm and private services. The branch surgery at Glaziers Lane also has a Jenny Wilson Practice Nurse dispensary. All of our consulting rooms are on the ground floor and the Karen Coxell Practice Nurse Harmoni for a GP or nurse - 111. When you call this number a receptionist surgeries provide baby changing and disabled facilities. -

Download the Guildford Local Plan
Schedule of proposed main modifications to the Submission Local Plan (2017) The proposed main modifications to the Submission Local Plan: Strategy and Sites are set out below. Text added is shown as underlined and deleted text is shown as strikethrough. Where maps have been modified, the area of change is shown within a yellow box and additions and deletions are shown on small inset maps. Contents Policies 2 Sites 46 Appendices 61 Appendix 1: Housing Trajectory 64 Appendix 2: Maps 67 1 Policies Mod Paragraph Proposed Modification No. or Section Policy S1: Presumption in favour of sustainable development MM1 Policy para (3) Where there are no policies relevant to the application or relevant policies are out of date at the time of (3)(a) making the decision, then the Council will grant permission unless material considerations indicate otherwise, taking into account whether: a) Specific policies in that Framework indicate that development should be restricted.The application of policies in the National Planning Policy Framework that protect areas or assets of particular importance provides a clear reason for refusing the development proposed; or MM1 Reasoned 4.1.4 Local Planning Authorities are encouraged to include a policy within their Local Plan that embraces the Justification presumption in favour of sustainable development. Policy S1 meets this requirement and adopts the para 4.1.4 model wording suggested. When implementing Policy S1, local circumstances will be taken into account to respond to different opportunities for achieving -
Maps Archive Part 2
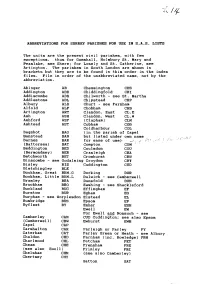
ABBREVIATIONS F O R S U R R E Y P A R I S H E S F O R U S E I N S . A . S . L I S T S T h e u n i t s a r e the present civil parishes. with few exceptions. t h u s f o r G o m s h a l l , H o l m b u r y S t . M a r y a n d Peaslake, see Shere; for L o s e l y a n d S t . C a t h e r i n e , s e e Artington. The parishes in South London are shown in b r a c k e t s b u t t h e y a r e t o be found in thisi o r d e r i n t h e i n d e x files. File in o r d e r o f t h e u n a b b r e v i a t e d n a m e , n o t b y t h e abbreviat ion. Ab i nger AB Chessington CHS Addington ADD Chiddingfold CHI Add i scombe ADS C h i l w o r t h - s e e St. Martha Addlestone ADL Chipstead CHP A1bury ALB C h u r t - s e e F a r n h a m Alfold ALF Chobham CHB Artington ART Clandon, East CL.E Ash ASH Clandon, West CL.W Ashford ASF (Clapham) CLM Ashtead AST Cobham COB Coldharbour COL Bagshot BAG (in the parish of Capel Banstead BAN but listed under own name Barnes BAR f o r e a s e o f u s e > (Battersea) BAT Compton COM Beddington BED Cou1sdon COU (Bermondsey) BER Cranleigh CRA Betchworth BET Crowhurst CRW B i n s c o m b e - s e e Godalming Croydon CRY Bisley BIS Cuddington CUD Bletchingley BLE Bookham, Great BKM.G Dorking DOR Bookham, Little BKM.L D u l w i c h - s e e C a m b e r w e l 1 Bramley BRA Dunsfold DUN Brockham BRO E a s h i n g - s e e S h a c k l e f o r d Buckland BUC Effingham EF Burstow BUR Egham EG B u r p h a m - s e e Worplesdon Elstead EL Busbridge BUS Epsom EP Byfleet BY Esher ESH Ewel 1 EW F o r E w e l l a n d N o n s u c h - s e e Camberley CAM CUD Cuddington; see also Epsom (Camberwel1) CBW Ewhurst EWH Capel CAP Carshalton CAR F a r l e i g h o r F a r l e y F Y Caterharo CAT F a r l e y G r e e n o r H e a t h - s e e A l b u r y Chaldon CHD F a r n h a m ( i n c . -

PCC Situation of Polling Stations
Police and Crime Commissioner election Situation of polling stations Police area name: Surrey Voting area name: Guildford Borough Council No. of polling Situation of polling station Description of station persons entitled to vote 1 / A1 Sutherland Memorial Hall, Clay Lane, Burpham, Surrey, GU4 7JU 2 / A2 Burpham Village Hall, Burpham Lane, Guildford, Surrey, GU4 7LP 3 / B1 Burchetts Farm Barn, Stoke Park, London Road, Guildford, GU1 1TU 4 / B2 Boxgrove Primary School, Boxgrove Lane, Guildford, Surrey, GU1 2TD 5 / C1 Guildford United Reformed Church (***PORTSMOUTH ROAD ENTRANCE***), Jubilee Room, Portsmouth Road, Guildford, Surrey, GU2 4BS 6 / C2 Guildford Park Church, Guildford Park Road, Guildford, Surrey, GU2 7NF 7 / C3 Shaftesbury Hall (*** NEW POLLING STATION ***), Artillery Terrace, Guildford, GU1 4NL 7 / C4 Shaftesbury Hall (*** NEW POLLING STATION ***), Artillery Terrace, Guildford, GU1 4NL 8 / C5 The Stirling Centre, St John's Church, Stoke Road, Guildford, GU1 1HB 9 / D1 The Studio, Guildford Adult & Community Learning Centre, Sydenham Road, Guildford, GU1 3RX 10 / D2-1 The Spike, Warren Road, Guildford, Surrey, GU1 3JH 11 / D2-2, D3 The Spike, Warren Road, Guildford, Surrey, GU1 3JH 12 / E1 Bushy Hill Junior School, Sheeplands Avenue, Merrow, Guildford, GU1 2SG 13 / E2 Merrow C E Infant School, Kingfisher Drive, Guildford, Surrey, GU4 7EA 14 / E3 Merrow Village Hall, 177 Epsom Road, Guildford, Surrey, GU1 2QY 15 / F1 Queen Eleanor's C of E Junior School (Main Hall) (Main Hall), Queen Eleanor's Road, Onslow Village, Guildford, -

Flood Forum Meeting
Approved minutes Flood Forum Meeting Minutes of the Flood Forum meeting held on Friday 7 February 2014 From 10.30am – 12.15pm Fairlands Community Centre, Fairlands 1. Present: Mrs Anne Milton MP – Chair, Mrs Gaynor White - Clerk to WPC, Mr John Burt - Resident Jacobs Well, Dr Paul Cragg, WPC – Mr Derek Slaymaker, WPC, Cllr David Elms – WPC/GBC, Mrs Eileen Peacock and Mr Chris Peacock – Residents Fairlands, Mrs Sandra Morgan - WPC, Mr Alex Lees - Resident Burdenshott Road, Mr John Phillips - Resident Whitmoor Common, Miss Shirley Brown - Resident Fairlands, Mr Ali Cotton – Halcrow, Mr Geoff Fowler - GBC, Ms Charlotte Williams - SWT, Mr Jason Lewis - SCC, Mrs Ann Brock - Resident Fairlands, Mr R Everest - Resident Littlefield Common, Mr Alan Dillon - Resident Fairlands, Mr Keith Crossman - Burpham Community Association, Mr Peter Trevena - Groundsman WPC, Mrs Justine Glyn Environment Agency, Paul Kenny - Group Commander - Operational Assurance & Community Impact, West Area Command Surrey Fire and Rescue Service , John Snare - Resident Pine Park , Mr Mark Havler – SWT, Francis Egleton – Thames Water, Dan Trenchard - Thames Water, Keith Herbert - Thames Water, Will Randall – Thames Water, John Morley - Resident Wood Street Village, Mr Chris Venables – WPC, Miss Helen Parkin – SCC, Mr Larry Rose - Resident Jacobs Well, Mr Geoff Timmins - Resident Wood Street Village. Mrs Milton thanked all of the officers from the various organisations for attending the meeting. Since its inauguration in 2005 the Worplesdon Flood Forum has gone from strength to strength. The format has been rolled out across the County and a number of new Flood Forums have now been established the latest being at Alfold, Surrey. -

Appendix 1: Delivery Document
APPENDIX 1: DELIVERY DOCUMENT LAND TO THE WEST OF FAIRLANDSA NEW NEIGHBOURHOOD MAY 2018 Contacts Contents Thakeham Homes London Studio Thakeham 1 Our Vision 3 Thakeham House, Summers Place, Stane Street 23-25 Great Sutton Street, Billingshurst, West Sussex RH14 9GN London EC1V 0DN The Site 4 T. +44(0)1403 787300 T. +44 (0)20 7017 1780 Location & Access 5 www.thakeham.com www.jtp.co.uk Local Character 6 Planning Context 7 Constraints & Opportunities 8 Design Principles 16 Barton Willmore RPS Planning & Development Design Concept 18 Masterplan 20 7 Soho Square, 321 Bradford Street, London W1D 3QB Birmingham, B5 6ET Landscape Strategy 24 T. +44 (0)20 7446 6888 T. +44 (0)121 213 5500 SANG Strategy 25 www.bartonwillmore.co.uk www.rpsgroup.com Access Strategy 26 Delivery 28 The Benefits of Development 33 EAD CgMs 3 Colleton Crescent, 140 London Wall, Exeter EX2 4DG London, EC2Y 5DN T. +44 (0)1392 260420 T. +44 (0)20 7832 1481 www.eadconsult.co.uk www.cgms.co.uk PROJECT CODE 01399 DISCLAIMER:DISCLAIMER: PROJECT CODE 01165 This report has been prepared for the sole use of Thakeham Homes and for the This report has been prepared for the sole use of Thakeham Homes and for the intended CREATEDCREATED BY BYNL/LW SXM/ SS intended purposes as stated in the agreement between Thakeham Homes and JTP. purposes as stated in the agreement between Thakeham Homes and JTP. No responsibility or No responsibility or liability is accepted towards any other person in respect of the CHECKEDCHECKED BY BYADAD liability is accepted towards any other person in respect of the use of this report or for use of this report or for reliance on the information contained in this report by any ISSUE TYPE FINAL reliance on the information contained in this report by any other person or for any other ISSUE TYPE FINAL DRAFT other person or for any other purpose. -

<Election Title>
Guildford Borough Council Election of Borough Councillors for the Burpham Ward STATEMENT OF PERSONS NOMINATED The following is a statement as to the persons nominated for the election of TWO Borough Councillors on Thursday, 7th May 2015 for the Burpham Ward. PERSONS NOMINATED 5. REASONS FOR WHICH THE 1. SURNAME, 2. HOME ADDRESS 3. DESCRIPTION 4. PROPOSER’S NAME RETURNING OFFICER HAS OTHER NAMES IN (if any) SECONDER’S NAME DECLARED A NOMINATION FULL INVALID Glassberg 12 Green Lane, Merrow, The Labour Party M P Hornsby-Smith(P), Ian B Barry Thomas Guildford, Surrey, GU1 Candidate Formby(S) 2LZ Holliday 72 Belmont Avenue, The Conservative P A Kelly(P), Elizabeth Christian John Guildford, Surrey, GU2 Party Candidate Critchfield(S) 9UF Kale Fairwater, Brook Lane, Liberal D Hurlow(P), N Hurlow(S) Nicole Jade Lucy Send, Woking, Surrey, Democrats GU23 7EH Mayne 1 Gatley Drive, Liberal D Hurlow(P), Nicky Hurlow(S) Ted Guildford, GU4 7JJ Democrats Newton 2 Fennell Close, The Labour Party H J A Cant(P), M P Hornsby- Adrian Charles Burpham, Guildford, Candidate Smith(S) Surrey, GU1 1YE Piper 1 Weylea Avenue, The Conservative P A Kelly(P), E Critchfield(S) Mike Burpham, Guildford, Party Candidate Surrey, GU4 7YN The persons opposite whose names no entry is made in column 5 have been and stand validly nominated Dated: Friday, 10 April 2015 Satish Mistry Returning Officer Guildford Borough Council Millmead House Millmead Guildford Surrey GU2 4BB Published and printed by Satish Mistry, Returning Officer, Guildford Borough Council, Millmead House, Millmead, Guildford, Surrey, GU2 4BB Guildford Borough Council Election of Borough Councillors for the Christchurch Ward STATEMENT OF PERSONS NOMINATED The following is a statement as to the persons nominated for the election of TWO Borough Councillors on Thursday, 7th May 2015 for the Christchurch Ward. -

Guildford Times
Guildford Times Conservatives keeping Guildford on the right track New hospital Guildford Electric buses station on track help for the help Park and A new bus fleet that is smoother, for arrival homeless a big Ride stay clean quieter, much better for the environment and runs on electricity priority and green GREEN PARK AND GLIDE - that is the latest innovation brought >> Page 2 >> Page 3 >> Page 4 to the town by the Conservatives. LAUNCHES IN GUILDFORD The single-decker buses are also built by Guildford-based Alexander Dennis, meaning that by using the buses, residents are also supporting Spring 2019 a local manufacturing business. Matt Furniss, Deputy Leader of Guildford Guildford Borough Council, said: “It’s easy to Park and Ride in Guildford. “From just £1.40 a day, it has always been cheaper than using a town centre car park. “Now it’s even more kind to the environment with green vehicles produced locally. Times “This all contributes to an improvement in air quality that we Serving the people of Guildford, Burpham, Merrow, Worplesdon, Pilgrims, Shalford, Onslow, Stoke, are also delivering for residents.” Stoughton, Park Barn, Compton, Artington, Peasmarsh, Fairlands, Jacobs Well and Charlotteville LOCAL ELECTIONS - Above: Conservative Councillors Philip Brooker, Christian Holliday, Matt Furniss, Nikki Nelson-Smith, Mike Piper and Graham Ellwood at the Spectrum Park and Glide, and right: one of the new Glide buses ALL ABOUT CONTACT BINS, NOT BREXIT Rt Hon Anne Milton MP On May 2, we have an Sometimes things have not Member of Parliament for Guildford opportunity to elect a Council worked out - and there have that delivers on key services.