An Update on the Management of Severe Crush Injury to the Forearm and Hand
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Crush Injuries Pathophysiology and Current Treatment Michael Sahjian, RN, BSN, CFRN, CCRN, NREMT-P; Michael Frakes, APRN, CCNS, CCRN, CFRN, NREMT-P
LWW/AENJ LWWJ331-02 April 23, 2007 13:50 Char Count= 0 Advanced Emergency Nursing Journal Vol. 29, No. 2, pp. 145–150 Copyright c 2007 Wolters Kluwer Health | Lippincott Williams & Wilkins Crush Injuries Pathophysiology and Current Treatment Michael Sahjian, RN, BSN, CFRN, CCRN, NREMT-P; Michael Frakes, APRN, CCNS, CCRN, CFRN, NREMT-P Abstract Crush syndrome, or traumatic rhabdomyolysis, is an uncommon traumatic injury that can lead to mismanagement or delayed treatment. Although rhabdomyolysis can result from many causes, this article reviews the risk factors, symptoms, and best practice treatments to optimize patient outcomes, as they relate to crush injuries. Key words: crush syndrome, traumatic rhabdomyolysis RUSH SYNDROME, also known as ology, pathophysiology, diagnosis, and early traumatic rhabdomyolysis, was first re- management of crush syndrome. Cported in 1910 by German authors who described symptoms including muscle EPIDEMIOLOGY pain, weakness, and brown-colored urine in soldiers rescued after being buried in struc- Crush injuries may result in permanent dis- tural debris (Gonzalez, 2005). Crush syn- ability or death; therefore, early recognition drome was not well defined until the 1940s and aggressive treatment are necessary to when nephrologists Bywaters and Beal pro- improve outcomes. There are many known vided descriptions of victims trapped by mechanisms inducing rhabdomyolysis includ- their extremities during the London Blitz ing crush injuries, electrocution, burns, com- who presented with shock, swollen extrem- partment syndrome, and any other pathology ities, tea-colored urine, and subsequent re- that results in muscle damage. Victims of nat- nal failure (Better & Stein, 1990; Fernan- ural disasters, including earthquakes, are re- dez, Hung, Bruno, Galea, & Chiang, 2005; ported as having up to a 20% incidence of Gonzalez, 2005; Malinoski, Slater, & Mullins, crush injuries, as do 40% of those surviving to 2004). -

With Crush Injury Syndrome
Crush Syndrome Made Simple Malta & McConnelsville Fire Department Division of Emergency Medical Service Objectives Recognize the differences between Crush Injury and Crush Syndrome Understand the interventions performed when treating someone with Crush Syndrome Assessing the Crush Injury victim S&S of crush injuries Treatment of crush injury Malta & McConnelsville Fire Department Division of Emergency Medical Service INJURY SYNDROME • Cell Disruption/ • Systemic effects injury at the point of when muscle is impact. RELEASED from Compression • Occurs < 1 hour • Occurs after cells have been under pressure >4 hours* • Suspect Syndrome with lightening strikes Malta & McConnelsville Fire Department Division of Emergency Medical Service CRUSHING MECHANISM OF INJURY • Building and Structure Collapse • Bomb Concussions • MVAs’ and Farm Accidents • Assault with blunt weapon Malta & McConnelsville Fire Department Division of Emergency Medical Service AKA: COMPRESSION SYNDROME First described by Dr. Minami in 1940 Malta & McConnelsville Fire Department Division of Emergency Medical Service INVOLVED ANATOMY Upper Arms Upper Legs Thorax and Buttocks Malta & McConnelsville Fire Department Division of Emergency Medical Service Crush Injuries Crush injuries occur when a crushing force is applied to a body area. Sometimes they are associated with internal organ rupture, major fractures, and hemorrhagic shock. Early aggressive treatment of patients suspected of having a crush injury is crucial. Along with the severity of soft tissue damage and fractures, a major concern of a severe crush injury is the duration of the compression/entrapment. Malta & McConnelsville Fire Department Division of Emergency Medical Service Crush Injuries Prolonged compression of a body region or limb may lead to a dangerous syndrome that can become fatal. Crush Syndrome is difficult to diagnose and treat in the pre-hospital setting because of the many complex variables involved. -

Approach to the Trauma Patient Will Help Reduce Errors
The Approach To Trauma Author Credentials Written by: Nicholas E. Kman, MD, The Ohio State University Updated by: Creagh Boulger, MD, and Benjamin M. Ostro, MD, The Ohio State University Last Update: March 2019 Case Study “We have a motor vehicle accident 5 minutes out per EMS report.” 47-year-old male unrestrained driver ejected 15 feet from car arrives via EMS. Vital Signs: BP: 100/40, RR: 28, HR: 110. He was initially combative at the scene but now difficult to arouse. He does not open his eyes, withdrawals only to pain, and makes gurgling sounds. EMS placed a c-collar and backboard, but could not start an IV. What do you do? Objectives Upon completion of this self-study module, you should be able to: ● Describe a focused rapid assessment of the trauma patient using an organized primary and secondary survey. ● Discuss the components of the primary survey. ● Discuss possible pathology that can occur in each domain of the primary survey and recommend treatment/stabilization measures. ● Describe how to stabilize a trauma patient and prioritize resuscitative measures. ● Discuss the secondary survey with particular attention to head/central nervous system (CNS), cervical spine, chest, abdominal, and musculoskeletal trauma. ● Discuss appropriate labs and diagnostic testing in caring for a trauma patient. ● Describe appropriate disposition of a trauma patient. Introduction Nearly 10% of all deaths in the world are caused by injury. Trauma is the number one cause of death in persons 1-50 years of age and results in significant life years lost. According to the National Trauma Data Bank, falls were the leading cause of trauma followed by motor vehicle collisions (MVCs) and firearm related injuries with an overall mortality rate of 4.39% in 2016. -

Ad Ult T Ra Uma Em E Rgen Cies
Section SECTION: Adult Trauma Emergencies REVISED: 06/2017 4 ADULT TRAUMA EMERGENCIES TRAUMA ADULT 1. Injury – General Trauma Management Protocol 4 - 1 2. Injury – Abdominal Trauma Protocol 4 - 2 (Abdominal Trauma) 3. Injury – Burns - Thermal Protocol 4 - 3 4. Injury – Crush Syndrome Protocol 4 - 4 5. Injury – Electrical Injuries Protocol 4 - 5 6. Injury – Head Protocol 4 - 6 7. Exposure – Airway/Inhalation Irritants Protocol 4 - 7 8. Injury – Sexual Assault Protocol 4 - 8 9. General – Neglect or Abuse Suspected Protocol 4 - 9 10. Injury – Conducted Electrical Weapons Protocol 4 - 10 (i.e. Taser) 11. Injury - Thoracic Protocol 4 - 11 12. Injury – General Trauma Management Protocol 4 – 12 (Field Trauma Triage Scheme) 13. Spinal Motion Restriction Protocol 4 – 13 14. Hemorrhage Control Protocol 4 – 14 Section 4 Continued This page intentionally left blank. ADULT TRAUMA EMERGENCIES ADULT Protocol SECTION: Adult Trauma Emergencies PROTOCOL TITLE: Injury – General Trauma Management 4-1 REVISED: 06/2015 PATIENT TRAUMA ASSESSMENT OVERVIEW Each year, one out of three Americans sustains a traumatic injury. Trauma is a major cause of disability in the United States. According to the Centers for Disease Control (CDC) in 2008, 118,021 deaths occurred due to trauma. Trauma is the leading cause of death in people under 44 years of age, accounting for half the deaths of children under the age of 4 years, and 80% of deaths in persons 15 to 24 years of age. As a responder, your actions within the first few moments of arriving on the scene of a traumatic injury are crucial to the success of managing the situation. -

Crush Injury Management
Crush Injury Management In the Underground Environment Background • 1910 - Messina Earthquake • WW2 - Air Raid Shelters fell on people crushing limbs - First time called Crush Syndrome • Granville Rail Disaster - Sydney Australia • Chain Valley Bay Colliery fatality 2011 What is it? Definition: Crush Injury • Injury that occurs because of pressure from a heavy object onto a body part • Squeezing of a body part between two objects Definition: Crush Syndrome The shock-like state following release of a limb or limbs, trunk and pelvis after a prolonged period of compression Crush Syndrome Basic Science • Muscle groups are covered by a tough membrane (fascia) that does not readily expand • Damage to these muscle groups cause swelling and/or bleeding; due to inelasticity of fascia, swelling occurs inward resulting in compressive force • Compressive force leads to vascular compromise with collapse of blood vessels, nerves and muscle cells • Without a steady supply of oxygen and nutrients, nerve and muscle cells die in a matter of hours • Problem is local to a limb or body area Traumatic • Crush syndrome - loss of blood to supply muscle tissue rhabdomyolysis toxins produced from muscle metabolism without oxygen as well as normal intracellular contents • Muscles can withstand approx. 4 hours without blood flow before cell death occurs • Toxins may continue to leak into body for as long as 60 hours after release of crush injury • The major problem is not recognising the potential for its existence, then removing the compressive force prior to arrival -

Crush Injury by an Elephant: Life-Saving Prehospital Care Resulting in a Good Recovery
Case reports Crush injury by an elephant: life-saving prehospital care resulting in a good recovery We present the first case of severe injuries caused by an elephant in an Australian zoo. Although the patient sustained potentially life-threatening injuries, excellent prehospital care allowed her to make a full recovery without any long-term complications. Clinical record it was difficult to interpret because of the extensive sub- cutaneous emphysema over the chest and abdominal A 41-year-old female zookeeper was urgently transferred walls. to the Royal North Shore Hospital Emergency Depart- ment (ED) by ambulance after a severe crush injury to the She was intubated and bilateral 32 Fr intercostal chest caused by a 2-year-old male elephant. catheters were inserted, which improved ventilation and haemodynamic stability; the bilateral decompres- The 1200 kg male Asian elephant was born in captivity sion needle catheters were removed. Chest x-rays and was well known to the keeper. On the day of the (Box 1) showed extensive subcutaneous emphysema, incident, they were involved in a training session when multiple rib fractures and a persistent small right apical the elephant challenged an instruction. The keeper rec- PTx. ognised this change in his behaviour and tried to leave the Computed tomography of the cervical spine, chest (Box 2) training area, but the elephant used his trunk to pin her by and abdomen showed injuries involving the spine, ribs, the chest against a bollard in the barn, resulting in im- sternum, lungs and liver (Box 3). mediate dyspnoea and brief loss of consciousness for 20e30 seconds. -

THE MEDICAL MANAGEMENT of the ENTRAPPED PATIENT with CRUSH SYNDROME REVISED: October 2019
MEDICAL GUIDANCE NOTE TITLE: THE MEDICAL MANAGEMENT OF THE ENTRAPPED PATIENT WITH CRUSH SYNDROME REVISED: October 2019 INTRODUCTION The following clinical guideline has been developed by the International Search and Rescue Advisory Group (INSARAG), Medical Working Group (MWG), which consists of medical professionals actively involved in the Urban Search and Rescue (USAR) medicine. The MWG is comprised of representatives from multiple countries and organisations drawn from the three INSARAG regional groups. This clinical guideline outlines a recommended approach to the management of crush syndrome in the austere environment of collapse structure response. While this is not intended to be a prescriptive medical protocol, USAR teams are encouraged to develop or review their own crush syndrome protocols within the context of this document. There is a lack of evidence-based research into prehospital treatment of crush syndrome in the collapsed structure environment. This document is to be considered as a consensus statement by members of the MWG based on current medical literature, expertise, and experience. In addition, it must be understood that these guidelines have been developed for application in a specific environment that may be complicated by factors such as: • Hazards to rescuers and patients e.g., secondary collapse; hazardous material; • Limited access to entrapped patient; • Limitations of medical and rescue equipment within the confined space;1 • Prolonged extrication and evacuation of patient; • Delayed access to definitive care. DEFINITIONS & BACKGROUND Crush Injury: Entrapment of parts of the body due to a compressive force that results in physical injury and or ischaemic injury to the muscle of the affected area. If significant muscle mass is involved, it can lead to crush syndrome following release of the compressive force. -

Discuss Crush Injuries And
Outline The Crush Syndrome Discuss crush injuries and the Crush Syndrome Define treatment Andre Campbell, MD, FACS, FCCM, FACP Discuss the treatment and Professor of Surgery UCSF, School of Medicine management mangled extremities San Francisco General Hospital Discuss vascular injury and assessment Case discussions The Crush Syndrome is the presence of localized crush injury with systemic manifestations: incidence 2-15% Crush Injury is compression of body parts Kobe Armenia causing localized muscle damage bombings, industrial accidents, building Bangladesh collapse, earthquake tornadoes Fukushima Haiti Page 1 Crush Injury Crush Injuries Muscle ischemia and Necrosis from Prolonged Pressure (Local effects) Injuries typically associated with disasters that include muscle injury, renal failure and death Crush Syndrome Man made-war and natural- earthquake (Systemic Effects) Earthquakes 3-20% of crush injuries Building collapse up to 40% of extricated victims Vehicular Disaster Fluid Retention in Extremities Myoglobinuria Metabolic Secondary Terrorist Acts- Oklahoma City, 9/11 (third spacing) Abnormalities Complications (electrolytes) Systemic manifestations of muscular cell damage resulting from pressure of crushing Hypotension Renal Failure Cardiac Arrhythmias Compartment Syndrome Crush Injuries The Crush Syndrome Recognized after the Messina earthquake of Characteristic Syndrome the results in 1909 and during WWI by German MDs rhadomyolysis, myoglobinuria, ARF. First described in the English literature by Three criteria Bywaters -
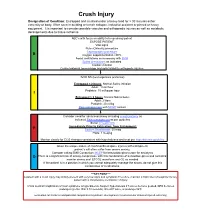
Crush Injury Designation of Condition: Entrapped and Crushed Under a Heavy Load for > 30 Minutes Either Extremity Or Body
Crush Injury Designation of Condition: Entrapped and crushed under a heavy load for > 30 minutes either extremity or body. Often seen in building or trench collapse, industrial accident or pinned or heavy equipment. It is important to consider possible vascular and orthopeadic injuries as well as metabolic derangements due to tissue ischemia. ABC’s with focus on ability to keep airway patent EXPOSE PATIENT Vital signs Pulse Oximetry procedure Capnography procedure B Oxygen supplementation >90% Assist ventilations as necessary with BVM Spinal precautions as indicated Cardiac monitor Control external hemorrhage and splint/stabilize orthopedic injuries IV/IO NS (two large bore preferred) Entrapped < 2 hours: Normal Saline infusion Adult: 1 liter/hour Pediatric: 10 ml/kg per hour I Entrapped > 2 hours: Normal Saline bolus Adult: 2 liters Pediatric: 20 ml/kg Pain management with MCEP contact Consider need for advanced airway including cricothyrotomy as indicated Pain management as per guideline Serial 12 lead ECG Immediately Prior to Extrication from Entrapment: P Sodium Bicarbonate: 50 meq Peds: 1 meq/kg Monitor closely for ECG changes consistent with hyperkalemia and treat per hyperkalemia guideline Given the unique nature of crush/confined space injuries with entrapment, patient’s will often suffer from severe anxiety. Consider calling EMS Consortium MCEP for benzodiazepines order for anxiolysis D There is a significant risk of airway compromise with this combination of benzodiazepines and narcotics; monitor airway and ETCO2 waveform and O2 as needed If the patient is in a position in which you cannot adequately manage the airway, do not give this combination of medications. ***KEY POINT*** A patient with a crush injury may initially present with very few signs and symptoms Therefore, maintain a high index of suspicion for any patient with a compressive mechanism of injury A fatal medical complication of crush syndrome is hyperkalemia. -

Fat Embolism Syndrome and Crush Syndrome
The Journal of Maharashtra Orthopaedic Association September / December - 2006 Fat Embolism Syndrome And Crush Syndrome Dr. Shivaprasad D. Khot M.S. Orth., D. Orth. ( Mumbai) Dr. Rahul S. Khot M.B.B.S., D. Orth., D.N.B. v Introduction v v Causes v Fat Embolism syndrome is a major cause of FES occurs most commonly as an early morbidity and mortality after multiple long bone complication of fractures of the pelvis and long fractures and is an important cause of ARDS. bones. FES is also reported in other entities: FES may be defined as, “a complex alteration l As a complication of reaming of medullary of homeostasis that occurs as an infrequent canals of long bones complication of fractures of long bones and pelvis l As a complication of reaming and cementation and manifests clinically as acute respiratory during joint replacement ? Massive soft tissue insufficiency”. injury ? Severe burns FES develops when fat emboli become l Liposuction impacted in pulmonary microcirculation and other l Chronic osteomyelitis microvascular beds such as the brain and is l Metabolic disorders characterized by respiratory failure, cerebral l dysfunction and petechiae. In-patients with pre Neoplasms existing pulmonary disease the addition of FES can l Renal transplant be life threatening. FES is an a important cause of l Bone infarcts in hemoglobinopathoies acute respiratory distress syndrome. With prompt l Collagen disease recognition, the treatment of the fat embolism l syndrome has become more specific and less empiric, Diabetes resulting in decrease morbidity and mortality. In l Severe infection recent years prevention of fat embolism syndrome l Inhalation anesthesia by early fracture fixation and patient mobilization l Blood transfusion has become the focus of a wave of clinical v Historical Aspects v investigation. -

Blunt Trauma
Multisystem Trauma Objectives Describe the pathophysiology and clinical manifestations of multisystem trauma complications. Describe the risk factors and criteria for the multisystem trauma patient. Describe the nursing management of the patient recovering from multisystem trauma. Describe the collaboration with the interdisciplinary teams caring for the multisystem trauma patient. Multisystem Trauma Facts Leading cause of death among children and adults below the age of 45 4th leading cause of death for all ages Accounts for approximately 170,000 deaths each year and over 400 deaths per day Affects mostly the young and the old Kills more Americans than stroke and AIDS combined Leading cause of disability Costs: 100 billion dollars to U.S. society annually Research dollars only 4% of U.S. federal research dollars Most traumas are preventable! Who Is a Trauma Patient? Evidence-Based Categories: Physiologic Criteria Mechanism of Injury Criteria Patient/Environmental Criteria Anatomic Criteria mc.vanderbilt.edu Umm.edu Physiologic Criteria Systolic blood pressure <90mm HG Respiratory rate 10 or >29 per minute Glasgow Coma Scale score <14 Nremtacademy.com Anatomic Criteria Penetrating injuries to the head, neck, torso or proximal extremities 2 or more obvious femur or humerus fractures Amputation above the waist or ankle Crushed, de-gloved or mangled extremities Open or depressed skull fracture Unstable chest wall (flail chest) Paralysis Pelvic fracture www.pulmccrn.org Mechanism of Injury Criteria Blunt Trauma: -

Objectives Case Study I. INTRODUCTION
Chapter 9: DISASTERS PRO D UCE D BY NATURAL PHE N OME N A Ruben J. Azocar, MD Dauryne Shaffer, RN, BS Objectives ■ Explain the health-related and economic impacts of natural disasters. ■ Identify common types of natural disasters and the injuries specific to each. ■ Outline general aspects of managing casualties after a natural disaster. ■ Discuss the intensivist’s role after a natural disaster. ■ Describe the management of crush injuries. Case Study Sixteen hours after an earthquake, a 35-year-old male is found trapped under his home. His left lower extremity is compressed from the mid-thigh down. Rescuers are preparing to extricate him from the rubble. - What kind of secondary injury is the man most likely to develop? - What is the most important therapeutic maneuver that should take place prior to extrication? - To what other injury is the pathophysiology of crush injury mostly closely related? I. INTRODUCTION Disasters produced by natural phenomena are sudden ecological events of sufficient magnitude to require external assistance. In recent years, these events have been affecting increasing numbers of people throughout the world. Since 2000, an average of 400 natural disasters a year have occurred worldwide, which is close to twice the occurrence in the 1980s and early 1990s. The chaos that accompanied Hurricane Katrina in 2005 illustrates how these phenomena can Fundamental Disaster Management affect even the most developed societies. Moreover, a natural disaster may precipitate a serious technological ! catastrophe by damaging nuclear power plants, buildings From 1991 to 2005, 3,470,162,961 that house dangerous biological or chemical products, people were affected by natural dams, or hydrocarbon-storage areas, thus becoming a disasters; 960,502 people were killed; natural and technological disaster.