Chemical Analysis of Urine 37
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Technical Report the Vitek Analyser for Routine Bacterial Identification And
316 J Clin Pathol 1998;51:316–323 Technical report J Clin Pathol: first published as 10.1136/jcp.51.4.316 on 1 April 1998. Downloaded from The Vitek analyser for routine bacterial identification and susceptibility testing: protocols, problems, and pitfalls N Shetty, G Hill, G L Ridgway Abstract covered, maintenance and quality control Automated and semiautomated technol- costs, and the presence of a versatile software ogy in microbiology has seen great ad- package. This report describes our experiences vances in recent years. The choice of with the Vitek system (bioMerieux, UK) in the automated equipment for the identifica- one year since its inception into a busy micro- tion and susceptibility testing of bacteria biology diagnostic laboratory in the United in a routine diagnostic laboratory depends Kingdom. It is worth noting that the choice on speed, accuracy, ease of use, and cost and range of antibiotics on susceptibility factors. The Vitek analyser (bioMerieux, testing cards were custom made for the UK) was installed in a busy diagnostic University College London Hospitals teaching hospital laboratory in London. (UCLH). This report describes one year’s experience. Changes to work practice as a result of incorporating the equipment into Identification and susceptibility testing the laboratory, and the advantages and on the Vitek system disadvantages of automation in key areas Identification of microorganisms is accom- are described in detail, together with pos- plished by biochemical methods. A turbido- sible solutions to problems. The Vitek metrically controlled suspension of pure colo- analyser was found to be valuable for the nies in saline is inoculated into identification http://jcp.bmj.com/ speed and accuracy with which results cards. -

Hyperbilirubinemia
Porphyrins Porphyrins (Porphins) are cyclic tetrapyrol compounds formed by the linkage )). of four pyrrole rings through methenyl bridges (( HC In the reduced porphyrins (Porphyrinogens) the linkage of four pyrrole rings (tetrapyrol) through methylene bridges (( CH2 )) The characteristic property of porphyrins is the formation of complexes with the metal ion bound to nitrogen atoms of the pyrrole rings. e.g. Heme (iron porphyrin). Proteins which contain heme ((hemoproteins)) are widely distributed e.g. Hemoglobin, Myoglobin, Cytochromes, Catalase & Tryptophan pyrrolase. Natural porphyrins have substituent side chains on the eight hydrogen atoms numbered on the pyrrole rings. These side chains are: CH 1-Methyl-group (M)… (( 3 )) 2-Acetate-group (A)… (( CH2COOH )) 3-Propionate-group (P)… (( CH2CH2COOH )) 4-Vinyl-group (V)… (( CH CH2 )) Porphyrins with asymmetric arrangement of the side chains are classified as type III porphyrins while those with symmetric arrangement of the side chains are classified as type I porphyrins. Only types I & III are present in nature & type III series is more important because it includes heme. 1 Heme Biosynthesis Heme biosynthesis occurs through the following steps: 1-The starting reaction is the condensation between succinyl-CoA ((derived from citric acid cycle in the mitochondria)) & glycine, this reaction is a rate limiting reaction in the hepatic heme synthesis, it occurs in the mitochondria & is catalyzed by ALA synthase (Aminolevulinate synthase) enzyme in the presence of pyridoxal phosphate as a cofactor. The product of this reaction is α-amino-β-ketoadipate which is rapidly decarboxylated to form δ-aminolevulinate (ALA). 2-In the cytoplasm condensation reaction between two molecules of ALA is catalyzed by ALA dehydratase enzyme to form two molecules of water & one 2 molecule of porphobilinogen (PBG) which is a precursor of pyrrole. -
Basic Skills in Interpreting Laboratory Data
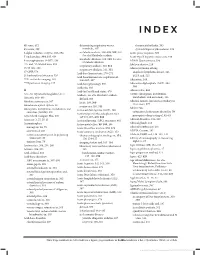
INDEX 4K score, 612 determining respiratory versus rheumatoid arthritis, 505 4Ts score, 399 metabolic, 307 systemic lupus erythematosus, 509 5-alpha reductase enzyme, 593–594 metabolic acidosis, 308–309, 309, 310. Acute phase response, 500 See also Metabolic acidosis 5' nucleotidase, 334, 335, 636 Acute type B hepatitis (minicase), 349 metabolic alkalosis, 309, 310. See also 6-mercaptopurine (6-MP), 138 ADAM Questionnaire, 596 Metabolic alkalosis 13C- and 14C-labeled urea, 353 Addison disease, 219 respiratory acidosis, 310, 311 15/15 rule, 208 Adenocarcinoma of lung respiratory alkalosis, 311, 311 17-OHP, 578 anaplastic lymphoma kinase, 526 Acid-base homeostasis, 270–271 21-hydroxylase deficiency, 526 EGFR and, 525 Acid-base homeostasis, regulation of, 99m Tc-sestamibi imaging, 165 306–307, 307 Adenosine, 164 201 TI perfusion imaging, 165 Acid-base physiology, 306 Adenosine diphosphate (ADP), 394, Acidemia, 303 394 A Acid-fast bacilli and stains, 470 Adenoviridae, 456 A1c. See Glycated hemoglobin (A1c) Acidosis. See also Metabolic acidosis ADME (absorption, distribution, metabolism, and excretion), 136 Abacavir, 468–469 defined, 303 Adnexal tumors, hirsutism secondary to Absolute neutropenia, 387 lactic, 308, 309 (minicase), 577 Absorbance optical system, 28 respiratory, 310, 311 Adolescents Absorption, distribution, metabolism, and Activated clotting time (ACT), 408 excretion (ADME), 136 categories of substances abused by, 70 Activated partial thromboplastin time prerequisite drug testing of, 82–83 Accu Check Compact Plus, 200 (aPTT), -

Bilirubin (Urine) Interpretive Summary
Bilirubin (Urine) Interpretive Summary Description: Bilirubinuria is an indicator of conjugated bilirubin in the urine. Excessive bilirubinuria in a dog or any bilirubinuria in a cat is an indication to evaluate serum bilirubin concentrations. Decreased Bilirubin Common Causes Normal Artifact o Exposure to UV light or room air o Delayed analysis o Centrifugation of urine prior to analysis o Ascorbic acid (Vitamin C) Increased Bilirubin Common Causes Normal dogs (especially males with concentrated urine) Liver disease, bile duct obstruction RBC destruction (hemolysis) o Immune-mediated hemolytic anemia o Zinc or onion toxicity o RBC parasites Uncommon Causes Hemoglobinuria Fever Prolonged anorexia False positive reactions due to medications o Phenothiazines (e.g., chlorpromazine) o Etodolac Related Findings Liver disease, biliary obstruction o Increased serum bilirubin, ALT, ALP, GGT, AST o Increased serum bile acids o Decreased albumin, cholesterol, BUN and glucose in severe cases o Abnormalities in liver and/or biliary tract on abdominal ultrasound RBC destruction o Decreased hematocrit, RBC, hemoglobin o Increased reticulocytes, increased MCV and decreased MCHC, polychromasia o Increased serum bilirubin o Spherocytosis (in dogs), autoagglutination o Hemoglobinuria o Positive Coombs or saline agglutination test may or may not be present with IMHA Generated by VetConnect® PLUS: Bilirubin (Urine) Page 1 of 2 Additional Information Physiology Conjugated bilirubin passes freely through the glomerular filtration barrier and is excreted in urine. Unconjugated bilirubin is bound to albumin and does not normally pass through the glomerular filtration barrier. Therefore, it is not detectable in urine (unless albuminuria or glomerular disease is present). Bilirubinuria usually precedes hyperbilirubinemia and icterus Dogs: Clinically normal dogs (especially males) may have detectable bilirubinuria in concentrated urine due to a low renal threshold for bilirubin. -

Leukocyte Esterase Activity in Vaginal Fluid of Pregnant and Non-Pregnant Women with Vaginitis/Vaginosis and in Controls
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by PubMed Central Infect Dis Obstet Gynecol 2003;11:19–26 Leukocyte esterase activity in vaginal fluid of pregnant and non-pregnant women with vaginitis/vaginosis and in controls Per-Anders Mårdh 1, Natalia Novikova 1, Ola Niklasson 1, Zoltan Bekassy 1 and Lennart Skude 2 1Department of Obstetrics and Gynecology, University Hospital, Lund and 2Department of Clinical Chemistry, County Hospital, Halmstad, Sweden Objectives: Todeterminethe leukocyteesterase (LE) activity invaginal lavage fluid ofwomen with acuteand recurrentvulvovaginal candidosis (VVC and RVVC respectively), bacterial vaginosis(BV), and in pregnant and non-pregnantwomen without evidenceof the threeconditions. Also tocompare the resultof LEtestsin women consultingat differentweeks inthe cycle andtrimesters of pregnancy.The LEactivity was correlatedto vaginal pH, numberof inflammatory cells instained vaginal smears,type of predominatingvaginal bacteria andpresence of yeast morphotypes. Methods: Onehundred and thirteen women with ahistoryof RVVC,i.e. with at least fourattacks of the conditionduring the previousyear and who had consultedwith anassumed new attack ofthe condition,were studied.Furthermore, we studied16 women with VVC,15 women with BV,and 27 women attendingfor control of cytological abnormalities, who all presentedwithout evidenceof either vaginitisor vaginosis. Finally, 73 pregnantwomen wereinvestigated. The LEactivity invaginal fluid duringdifferent weeks inthe cycle of 53 of the women was measured. Results: Inthe non-pregnantwomen, anincreased LE activity was foundin 96, 88, 73 and56% of those with RVVC,VVC and BV andin the non-VVC/BVcases,respectively. In 73% of pregnantwomen inthe second trimester,and 76% of thosein the third,the LEtestwas positive.In all groupsof non-pregnantwomen tested, the LEactivity correlatedwith the numberof leukocytesin vaginal smears,but it didnot in those who were pregnant.There was nocorrelation between LE activity andweek incycle. -

Porphyrins & Bile Pigments
Bio. 2. ASPU. Lectu.6. Prof. Dr. F. ALQuobaili Porphyrins & Bile Pigments • Biomedical Importance These topics are closely related, because heme is synthesized from porphyrins and iron, and the products of degradation of heme are the bile pigments and iron. Knowledge of the biochemistry of the porphyrins and of heme is basic to understanding the varied functions of hemoproteins in the body. The porphyrias are a group of diseases caused by abnormalities in the pathway of biosynthesis of the various porphyrins. A much more prevalent clinical condition is jaundice, due to elevation of bilirubin in the plasma, due to overproduction of bilirubin or to failure of its excretion and is seen in numerous diseases ranging from hemolytic anemias to viral hepatitis and to cancer of the pancreas. • Metalloporphyrins & Hemoproteins Are Important in Nature Porphyrins are cyclic compounds formed by the linkage of four pyrrole rings through methyne (==HC—) bridges. A characteristic property of the porphyrins is the formation of complexes with metal ions bound to the nitrogen atom of the pyrrole rings. Examples are the iron porphyrins such as heme of hemoglobin and the magnesium‐containing porphyrin chlorophyll, the photosynthetic pigment of plants. • Natural Porphyrins Have Substituent Side Chains on the Porphin Nucleus The porphyrins found in nature are compounds in which various side chains are substituted for the eight hydrogen atoms numbered in the porphyrin nucleus. As a simple means of showing these substitutions, Fischer proposed a shorthand formula in which the methyne bridges are omitted and a porphyrin with this type of asymmetric substitution is classified as a type III porphyrin. -

Proteinuria and Bilirubinuria As Potential Risk Indicators of Acute Kidney Injury During Running in Outpatient Settings
medicina Article Proteinuria and Bilirubinuria as Potential Risk Indicators of Acute Kidney Injury during Running in Outpatient Settings Daniel Rojas-Valverde 1,2,* , Guillermo Olcina 2,* , Braulio Sánchez-Ureña 3 , José Pino-Ortega 4 , Ismael Martínez-Guardado 2 and Rafael Timón 2,* 1 Centro de Investigación y Diagnóstico en Salud y Deporte (CIDISAD), Escuela Ciencias del Movimiento Humano y Calidad de Vida (CIEMHCAVI), Universidad Nacional, Heredia 86-3000, Costa Rica 2 Grupo en Avances en el Entrenamiento Deportivo y Acondicionamiento Físico (GAEDAF), Facultad Ciencias del Deporte, Universidad de Extremadura, 10005 Cáceres, Spain; [email protected] 3 Programa Ciencias del Ejercicio y la Salud (PROCESA), Escuela Ciencias del Movimiento Humano y Calidad de Vida (CIEMHCAVI), Universidad Nacional, Heredia 86-3000, Costa Rica; [email protected] 4 Departmento de Actividad Física y Deporte, Facultad Ciencias del Deporte, 30720 Murcia, Spain; [email protected] * Correspondence: [email protected] (D.R.-V.); [email protected] (G.O.); [email protected] (R.T.); Tel.: +506-8825-0219 (D.R.-V.) Received: 2 September 2020; Accepted: 19 October 2020; Published: 27 October 2020 Abstract: Background and objectives: The purpose of this study was to explore which urinary markers could indicate acute kidney injury (AKI) during prolonged trail running in outpatient settings. Materials and Methods: Twenty-nine experienced trail runners (age 39.1 8.8 years, weight 71.9 11 kg, ± ± height 171.9 8.3 cm) completed a 35 km event (cumulative positive ascend of 1815 m, altitude = 906 to ± 1178 m.a.s.l.) under a temperature of 25.52 1.98 C and humidity of 79.25 7.45%). -

Time-To-Positivity, Type of Culture Media and Oxidase Test Performed on Positive Blood Culture Vials to Predict Pseudomonas Aeru
Original Nazaret Cobos-Trigueros1 Time-to-positivity, type of culture media and oxidase Yuliya Zboromyrska2 Laura Morata1 test performed on positive blood culture vials to predict Izaskun Alejo2 Cristina De La Calle1 Pseudomonas aeruginosa in patients with Gram-negative Andrea Vergara2 Celia Cardozo1 bacilli bacteraemia 1 Maria P. Arcas 1 1 Department of Infectious Diseases, Hospital Clínic, IDIBAPS, Barcelona University, Barcelona, Spain. Alex Soriano 2Department of Clinical Microbiology, Hospital Clínic, Barcelona University, Barcelona, Spain. Francesc Marco2 Josep Mensa1 Manel Almela2 Jose A. Martinez1 ABSTRACT Tiempo de positividad, tipo de medio de cultivo y prueba de oxidasa realizada en Introduction. The aim of this study was to determine the viales de hemocultivo positivos para predecir usefulness of oxidase test and time-to-positivity (TTP) in aer- Pseudomonas aeruginosa en pacientes con obic and anaerobic blood culture vials to detect the presence bacteriemia por bacilos gramnegativos of Pseudomonas aeruginosa in patients with Gram-negative bacilli (GNB) bacteraemia. RESUMEN Material and methods. TTP was recorded for each aer- obic and anaerobic blood culture vial of monomicrobial bac- Introducción. El objetivo del estudio fue determinar la utili- teraemia due to GNB. Oxidase test was performed in a pellet dad de la prueba de oxidasa y del tiempo de positividad del hemo- of the centrifuged content of the positive blood culture. An cultivo (TPH) para detectar la presencia de Pseudomonas aerugino- algorithm was developed in order to perform the oxidase test sa en pacientes con bacteriemia por bacilos gramnegativos (BGN). efficiently taking into account TTP and type of vial. Material y métodos. Se registró el TPH de cada vial ae- Results. -

Ileal Neobladder: an Important Cause of Non-Anion Gap Metabolic Acidosis
The Journal of Emergency Medicine, Vol. 52, No. 5, pp. e179–e182, 2017 Ó 2017 Elsevier Inc. All rights reserved. 0736-4679/$ - see front matter http://dx.doi.org/10.1016/j.jemermed.2016.12.036 Clinical Communications: Adult ILEAL NEOBLADDER: AN IMPORTANT CAUSE OF NON-ANION GAP METABOLIC ACIDOSIS Jesse W. St. Clair, MD and Matthew L. Wong, MD, MPH Department of Emergency Medicine, Beth Israel Deaconess Medical Center, Boston, Massachusetts and Department of Emergency Medicine, Harvard Medical School, Boston, Massachusetts Reprint Address: Matthew L. Wong, MD, MPH, Department of Emergency Medicine, Beth Israel Deaconess Medical Center, Rosenberg Building, 2nd Floor, 1 Deaconess Road, Boston, MA 02446 , Abstract—Background: The differential diagnosis for a disease, or medications such as acetazolamide. non-anion gap metabolic acidosis is probably less well Commonly used mnemonics to remember the differential known than the differential diagnosis for an anion gap for the non-anion gap metabolic acidosis include metabolic acidosis. One etiology of a non-anion gap acidosis ‘‘ABCD’’ for ‘‘Addison’s, Bicarbonate loss, Chloride is the consequence of ileal neobladder urinary diversion (administration), and Drugs,’’ as well as ‘‘HARDUP’’ for the treatment of bladder cancer. Case Report: We pre- for ‘‘Hyperchloremia, Acetazolamide and Addison’s, sent a case of a patient with an ileal neobladder with a severe non-anion gap metabolic acidosis caused by a Renal Tubular Acidosis, Diarrhea, Ureteroenterostomies, urinary tract infection and ureteroenterostomy. Why and Pancreaticoenterostomies’’ (Table 1) (1). Should an Emergency Physician Be Aware of This?: Part Ureteroenterostomies are when the ureter has an of the ileal neobladder surgery includes ureteroenteros- abnormal connection with a segment of intestine. -

Paroxysmal Nocturnal Hemoglobinuria
Paroxysmal nocturnal hemoglobinuria Description Paroxysmal nocturnal hemoglobinuria is an acquired disorder that leads to the premature death and impaired production of blood cells. The disorder affects red blood cells (erythrocytes), which carry oxygen; white blood cells (leukocytes), which protect the body from infection; and platelets (thrombocytes), which are involved in blood clotting. Paroxysmal nocturnal hemoglobinuria affects both sexes equally, and can occur at any age, although it is most often diagnosed in young adulthood. People with paroxysmal nocturnal hemoglobinuria have sudden, recurring episodes of symptoms (paroxysmal symptoms), which may be triggered by stresses on the body, such as infections or physical exertion. During these episodes, red blood cells are prematurely destroyed (hemolysis). Affected individuals may pass dark-colored urine due to the presence of hemoglobin, the oxygen-carrying protein in blood. The abnormal presence of hemoglobin in the urine is called hemoglobinuria. In many, but not all cases, hemoglobinuria is most noticeable in the morning, upon passing urine that has accumulated in the bladder during the night (nocturnal). The premature destruction of red blood cells results in a deficiency of these cells in the blood (hemolytic anemia), which can cause signs and symptoms such as fatigue, weakness, abnormally pale skin (pallor), shortness of breath, and an increased heart rate. People with paroxysmal nocturnal hemoglobinuria may also be prone to infections due to a deficiency of white blood cells. Abnormal platelets associated with paroxysmal nocturnal hemoglobinuria can cause problems in the blood clotting process. As a result, people with this disorder may experience abnormal blood clotting (thrombosis), especially in large abdominal veins; or, less often, episodes of severe bleeding (hemorrhage). -

Rules of the Alabama Department of Forensic Sciences Chapter 370-1-1 Chemical Test for Intoxication Table of Contents 370-1-1
RULES OF THE ALABAMA DEPARTMENT OF FORENSIC SCIENCES CHAPTER 370-1-1 CHEMICAL TEST FOR INTOXICATION TABLE OF CONTENTS 370-1-1-.01 Admissibility Rule for the Evidential Breath Alcohol Test Method 370-1-1-.03 Blood, Urine, and Other Bodily Substances 370-1-1-.04 Field Sobriety Screening Tests 370-1-1-.05 Field Sobriety Alcohol Screening Devices 370-1-1-.06 Field Sobriety Drug Screening Devices 370-1-1-.01 Admissibility Rule for the Evidential Breath Alcohol Test Method. (1) Purpose. This rule addresses the statutory elements required for the admissibility of evidence obtained from Breath Alcohol Testing Instruments. This rule contains the METHOD, as referred to by §32-5A-194 Code of Alabama, 1975 as amended, which insures and verifies that each individual Breath Alcohol Test is performed accurately and reliably. IN EVENT THAT ONE OF THESE REQUIREMENTS IS NOT FULFILLED, BREATH ALCOHOL TESTING EVIDENCE MAY STILL BE OFFERED THROUGH TRADITIONAL EVIDENTIARY PREDICATE as approved of in Ex parte Mayo, 652 So. 2d 201 (Ala. 1994). (2) Definitions and Abbreviations. (a) Draeger 7110 MKIII (i) Acceptable Breath Sample. For the purpose of this rule the subject must provide the Draeger Alcotest 7110 MKIII with a breath sample of sufficient volume and duration, as required by the software to be accepted for analysis. Software versions prior to and including version 3.24 require the subject to provide a minimum of 1.5 liters of breath, for a minimum of 4.5 seconds. Software versions 3.25 or later require the subject to provide a minimum of 1.3 liters of breath, for a minimum of 4.0 seconds. -

The Effect of Flood Diuresis on Hemo-Globinuria
THE EFFECT OF FLOOD DIURESIS ON HEMO- GLOBINURIA. BY HERBERT HAESSLERj M.D. (From the Laboratories of The Rockefeller Inatitute for Medical Research.) (Received for publication, November 9, 1921.) The fact is well recognized that a considerable quantity of hemo- globin must be free in the plasma if any is to pass the renal barrier and appear in the urine. The pigment is, like dextrose, a "threshold substance." It readily penetrates into the renal tubules but is absorbed again more or less completely during its course through them. t This being true, diuresis should diminish the chances of absorption by hastening the flow of fluid, and tend to lead to the appearance of the pigment in the urine. Evidence will here be presented that such is the case. Hemoglobinuria, like glycosuria, is much favored by flood diuresis. Method. A concentrated solution of hemoglobin was abruptly thrown into the circulation of rabbits and dogs, followed in some instances by a slower injection of salt solution. The amount of pigment introduced was slightly less than that required to produce hemoglobinuria in the absence of diuresis. The urine was collected at intervals by catheter. All of the animals were males. Individuals were selected with normal kidneys, as indicated by ~e general character of the urine and proven by the autopsy findings. Great care was necessary to prevent hemorrhage during the catheterization of the rabbits, and despite it a few red cells were frequently encountered after- wards in the urine. For this reason the experiments were repeated on dogs, in which the complication can be avoided.