Roe V. Wade</Em>
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

DAVID S. COHEN Drexel University Thomas R
DAVID S. COHEN Drexel University Thomas R. Kline School of Law 3320 Market St. Philadelphia, PA 19104 (215)571-4714 [email protected] TEACHING EXPERIENCE DREXEL UNIVERSITY THOMAS R. KLINE SCHOOL OF LAW, Philadelphia, PA 2006-current Professor of Law Teach Constitutional Law courses and Sex, Gender, and the Law. AWARDS: Dean Jennifer L. Rosato Excellence in the Classroom Award (2009, 2010, 2012, 2015, 2016) Abortion Care Network Person of the Year (2016) Center for Reproductive Rights Innovation in Scholarship Award (2015) UNIVERSITY OF PENNSYLVANIA LAW SCHOOL, Philadelphia, PA 2003-06 Lecturer-in-Law Taught upper-level seminar each spring entitled “Sex Discrimination and the Law.” UNIVERSITY OF PENNSYLVANIA, Philadelphia, PA 2004-05 Adjunct Professor Taught undergraduate seminar each fall entitled “Law and Social Policy of Sex and Reproduction.” LONG ISLAND UNIVERSITY, Brooklyn, NY 2000-01 Adjunct Assistant Professor Developed and taught graduate-level political science classes entitled “The American Constitution and Political System” and “Current Topics in Law and Politics.” EDUCATION COLUMBIA UNIVERSITY SCHOOL OF LAW, J.D. 1997 Honors: Harlan Fiske Stone Scholar, 1994-97 Public Interest Commitment Award Columbia Human Rights Fellowship Activities: Columbia Human Rights Law Review, Managing Editor/Head Articles Editor Columbia Journal of Gender and Law, Articles Editor Professor Kimberlé Crenshaw, Research Assistant DARTMOUTH COLLEGE, B.A. in Philosophy with Women’s Studies minor, 1994 JUDICIAL CLERKSHIPS U.S. COURT OF APPEALS, NINTH CIRCUIT, Santa Ana, CA 1998-99 Judicial Law Clerk for the Honorable Warren J. Ferguson 1 SUPREME COURT OF NEW JERSEY, Trenton, NJ 1997-98 Judicial Law Clerk for the Honorable Alan B. -

The Epidemiology of Abortion and Its Prevention in Chile, 79(5) Rev
Gene Gene Start Gene End Motif Start Motif End Motif Strand Exon Start Exon End HS Start HS End Distance NLGN4X 5808082 6146706 5821352 5821364 gtggccacggcgg ‑ 5821117 5821907 5811910 5813910 7442 AFF2 147582138 148082193 148048477 148048489 ccaccatcacctc + 148048319 148048609 148036319 148040319 8158 NLGN3 70364680 70391051 70386983 70386995 gtggatatggtgg + 70386860 70387650 70371089 70377089 9894 MECP2 153287263 153363188 153296166 153296178 gtggtgatggtgg ‑ 153295685 153296901 153306976 153308976 10798 FRMPD4 12156584 12742642 12739916 12739928 ccaccatggccgc + 12738647 12742642 12721454 12727454 12462 PHF8 53963112 54071569 54012352 54012364 ccaccatgtcctc ‑ 54012339 54012382 54025089 54033089 12725 RAB39B 154487525 154493852 154493567 154493579 cctccatggccgc ‑ 154493358 154493852 154478566 154480566 13001 FRMPD4 12156584 12742642 12736309 12736321 ggggcaagggagg + 12735619 12736909 12721454 12727454 14867 GRPR 16141423 16171641 16170710 16170722 cctccgtggccac + 16170378 16171641 16208454 16211454 37732 AFF2 147582138 148082193 148079262 148079274 cccccgtcaccac + 148072740 148082193 148036319 148040319 38943 SH3KBP1 19552082 19905744 19564111 19564123 cctccttatcctc ‑ 19564039 19564168 19610454 19614454 46331 PDZD4 153067622 153096003 153070331 153070343 cccccttctcctc ‑ 153067622 153070355 153013976 153018976 51355 SLC6A8 152953751 152962048 152960611 152960623 ccaccctgacccc + 152960528 152962048 153013976 153018976 53353 FMR1 146993468 147032647 147026533 147026545 gaggacaaggagg + 147026463 147026571 147083193 147085193 56648 HNRNPH2 -
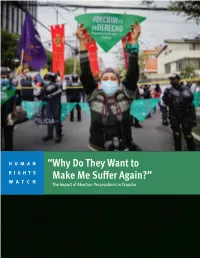
“Why Do They Want to Make Me Suffer Again?” the Impact of Abortion Prosecutions in Ecuador
HUMAN “Why Do They Want to RIGHTS WATCH Make Me Suffer Again?” The Impact of Abortion Prosecutions in Ecuador “Why Do They Want to Make Me Suffer Again?” The Impact of Abortion Prosecutions in Ecuador Copyright © 2021 Human Rights Watch All rights reserved. Printed in the United States of America ISBN: 978-1-62313-919-3 Cover design by Rafael Jimenez Human Rights Watch defends the rights of people worldwide. We scrupulously investigate abuses, expose the facts widely, and pressure those with power to respect rights and secure justice. Human Rights Watch is an independent, international organization that works as part of a vibrant movement to uphold human dignity and advance the cause of human rights for all. Human Rights Watch is an international organization with staff in more than 40 countries, and offices in Amsterdam, Beirut, Berlin, Brussels, Chicago, Geneva, Goma, Johannesburg, London, Los Angeles, Moscow, Nairobi, New York, Paris, San Francisco, Sydney, Tokyo, Toronto, Tunis, Washington DC, and Zurich. For more information, please visit our website: http://www.hrw.org JULY 2021 ISBN: 978-1-62313-919-3 “Why Do They Want to Make Me Suffer Again?” The Impact of Abortion Prosecutions in Ecuador Summary ........................................................................................................................... 1 Key Recommendations ....................................................................................................... 8 To the Presidency ................................................................................................................... -

The Safety and Quality of Abortion Care in the United States (2018)
THE NATIONAL ACADEMIES PRESS This PDF is available at http://nap.edu/24950 SHARE The Safety and Quality of Abortion Care in the United States (2018) DETAILS 222 pages | 6 x 9 | PAPERBACK ISBN 978-0-309-46818-3 | DOI 10.17226/24950 CONTRIBUTORS GET THIS BOOK Committee on Reproductive Health Services: Assessing the Safety and Quality of Abortion Care in the U.S.; Board on Population Health and Public Health Practice; Board on Health Care Services; Health and Medicine Division; National FIND RELATED TITLES Academies of Sciences, Engineering, and Medicine SUGGESTED CITATION National Academies of Sciences, Engineering, and Medicine 2018. The Safety and Quality of Abortion Care in the United States. Washington, DC: The National Academies Press. https://doi.org/10.17226/24950. Visit the National Academies Press at NAP.edu and login or register to get: – Access to free PDF downloads of thousands of scientific reports – 10% off the price of print titles – Email or social media notifications of new titles related to your interests – Special offers and discounts Distribution, posting, or copying of this PDF is strictly prohibited without written permission of the National Academies Press. (Request Permission) Unless otherwise indicated, all materials in this PDF are copyrighted by the National Academy of Sciences. Copyright © National Academy of Sciences. All rights reserved. The Safety and Quality of Abortion Care in the United States THE SAFETY AND QUALITY OF ABORTION CARE IN THE UNITED STATES Committee on Reproductive Health Services: Assessing the Safety and Quality of Abortion Care in the U.S. Board on Population Health and Public Health Practice Board on Health Care Services Health and Medicine Division A Consensus Study Report of Copyright National Academy of Sciences. -

Induced Abortion in Chile
In Brief Induced Abortion in Chile Chile is one of a small handful of countries worldwide that Abortion-related deaths and injuries appear to have declined dramatically prohibit induced abortion under any circumstance, including In the 1960s, many Chilean women if a woman’s life is at risk. The longstanding ban, which undergoing unsafe abortions died as a result, or suffered serious short- or long- runs counter to Chile’s stated commitment to international term health complications for which they women’s rights treaties, faces a robust challenge in the did not receive the medical treatment they needed.9 In 1960, there were 294 form of a recent bill proposed by the government of maternal deaths per 100,000 live births,10 and one-third of these deaths were at- President Bachelet that would allow the procedure under tributable to unsafe abortion.11 One in limited circumstances. Yet informed debate on the topic is five hospital beds in obstetric depart- ments were occupied by women receiving hindered by the lack of data on the incidence and context of postabortion treatment. clandestine induced abortion. Chile’s maternal mortality ratio fell to 55 deaths per 100,000 live births by In every country, regardless of the legal No data exist on the characteristics of 1990, and to 22 by 2013.12 The precise status of induced abortion, some women women obtaining abortions in Chile, nor contribution of unsafe induced abortion experiencing an unintended pregnancy on their reasons for doing so. As one to overall maternal mortality is unclear, turn to abortion to end it.1 Chile is no researcher points out, “we do not know… but experts agree that far fewer deaths exception to this worldwide pattern. -

A Reproductive Right, Or a Moral Profligacy?
A REPRODUCTIVE RIGHT, OR A MORAL PROFLIGACY? A POLICY PAPER DISCUSSING THE LEGISLATIVE FUTURE FOR MALTA An Għaqda Studenti Tal-Liġi Policy Paper © Għaqda Studenti tal-Liġi 2020 OPENING REMARKS INTRODUCTION It is with great pleasure that I present A multidisciplinary modus operandi was to you this year’s GħSL policy paper employed to offer a holistic discussion addressing the subject of Abortion, a and this was achieved through a paper which is the culmination of the thorough examination of pertinent comprehensive work of the GħSL Policy areas beyond the legal sphere such as Office. medical research, ethical considerations involved, as well as the psychological GħSL strives to keep law students as aspects, among others. well as society as a whole abreast regarding current legal issues in Malta. Moreover, a comparative exercise was An ongoing area of contention featuring carried out, whereby the laws regulating, across local media centres around the restricting and prohibiting abortion were topic of abortion. Due to the polarised evaluated. This contributed towards a views on this subject, the GħSL comprehensive outcome of this policy Executive Board decided that it would paper and provided a robust reference be opportune to delve into this topic. point for active and potential students alike. As a body representing the interests of law students, throughout this paper our Finally, I would like to thank the main focus was to maintain and uphold colleagues of GħSL, including all those an impartial appreciation of the law who contributed to this paper, namely while taking into account the sensitive Dr Desiree Attard, Andrew Sciberras, nature of this topic. -

November 2015 Supreme Court Agrees to Hear Lawsuit Challenging Texas’ Pro-Life Law by Dave Andrusko
November 2015 Supreme Court agrees to hear lawsuit challenging Texas’ pro-life law By Dave Andrusko As widely, but not universally issue and lower courts have expected, the United States disagreed over the requirement Supreme Court agreed Friday that abortionists have admitting to take up a lawsuit brought by privileges at a nearby hospital a coalition of abortion providers for situations of medical that challenges two provisions emergencies. HB2 also requires of H.B. 2, an omnibus 2013 that abortion clinics meet the Texas law. same building standards as However reluctant justices ambulatory surgical centers. may (or may not) have been It is noteworthy what to wade into the abortion was never challenged: the controversy, it made sense Pain-Capable Unborn Child for the High Court to hear Protection Act. Also not before Whole Woman’s Health v. Cole. Abortion is an important See “Court,” page 17 Frustrated with Congress? Elect a Pro-life President and more pro-life senators By Karen Cross, National Right to Life Political Director According to a Gallup poll life legislation and it goes to released November 12, only the U.S. Senate. Under most 11% of Americans approve of circumstances sixty votes are Congress – the lowest point this required for passage. We don’t year and one of the lowest ever. have 60 pro-life votes in the But pro-lifers are frustrated Senate. for a very different reason. Both The Pain-Capable Unborn houses of Congress have strong Child Protection Act (H.R. pro-life leadership, but their 36), which would protect from efforts have been stymied by abortion unborn children 20 pro-abortion President Barack weeks or older, easily passed Obama and an entrenched pro- the U.S. -

Bibliography of Sexuality Studies in Latin America
Bibliography of Sexuality Studies in Latin America In 1997 Donna J. Guy and I published a bibliography of sexuality studies on Latin America in our edited book Sex and Sexuality in Latin America (New York University Press, 1997), including studies in a wide variety of fields. This bibliography was updated for the Spanish edition of that book, Sexo y sexualidades en América Latina (Paidos, Buenos Aires, 1998); that version included a number of items that had come to our attention after we turned in the book to NYU. Interestingly, the number of publications in Latin America (and in Spanish and Portuguese) increased in that brief period, and continues to increase. Adán Griego has added his own bibliography and has agreed to maintain it and keep it current. The bibliography that follows is based on the previous ones but has the advantage of not being fixed in time. —— Daniel Balderston, 1999. This bibliographic list is organized alphabetically by author, or by title in a few cases where no specific author appears. Select the initial letter of the author or the title of the work you are looking for or simply scroll down the list. Please send corrections, additions and comments to: [email protected] A A las orillas de Lesbos. Narrativa lésbica. Lima: MHOL, 1997. Abad, Erika Gisela. "¿La Voz de Quién?" Diálogo, No.12, (Summer 2009): 28. Abdalla, Fernanda Tavares de Mello and Nichiata, Lúcia Yasuko Izumi. A Abertura da privacidade e o sigilo das informações sobre o HIV/Aids das mulheres atendidas pelo Programa Saúde da Família no município de São Paulo, Brasil. -

Amnesty International Report 2014/15 the State of the World's Human Rights
AMNESTY INTERNATIONAL OF THE WORLD’S HUMAN RIGHTS THE STATE REPORT 2014/15 AMNESTY INTERNATIONAL REPORT 2014/15 THE STATE OF THE WORLD’S HUMAN RIGHTS The Amnesty International Report 2014/15 documents the state of human rights in 160 countries and territories during 2014. Some key events from 2013 are also reported. While 2014 saw violent conflict and the failure of many governments to safeguard the rights and safety of civilians, significant progress was also witnessed in the safeguarding and securing of certain human rights. Key anniversaries, including the commemoration of the Bhopal gas leak in 1984 and the Rwanda genocide in 1994, as well as reflections on 30 years since the adoption of the UN Convention against Torture, reminded us that while leaps forward have been made, there is still work to be done to ensure justice for victims and survivors of grave abuses. AMNESTY INTERNATIONAL This report also celebrates those who stand up REPORT 2014/15 for human rights across the world, often in difficult and dangerous circumstances. It represents Amnesty International’s key concerns throughout 2014/15 the world, and is essential reading for policy- THE STATE OF THE WORLD’S makers, activists and anyone with an interest in human rights. HUMAN RIGHTS Work with us at amnesty.org AIR_2014/15_cover_final.indd All Pages 23/01/2015 15:04 AMNESTY INTERNATIONAL Amnesty International is a global movement of more than 7 million people who campaign for a world where human rights are enjoyed by all. Our vision is for every person to enjoy all the rights enshrined in the Universal Declaration of Human Rights and other international human rights standards. -

J-A21004-14 2015 PA Super 12 COMMONWEALTH OF
J-A21004-14 2015 PA Super 12 COMMONWEALTH OF PENNSYLVANIA, IN THE SUPERIOR COURT OF PENNSYLVANIA Appellee v. EILEEN O’NEIL, Appellant No. 2506 EDA 2013 Appeal from the Judgment of Sentence July 15, 2013 In the Court of Common Pleas of Philadelphia County Criminal Division at No(s): CP-51-CR-0001668-2011 BEFORE: BOWES, OTT, and STRASSBURGER,* JJ. OPINION BY BOWES, J.: FILED JANUARY 20, 2015 Eileen O’Neil appeals from the judgment of sentence of six to twenty- three months incarceration to be followed by two years of probation after a jury found her guilty of two counts each of conspiracy to commit corrupt organizations and theft by deception. We reverse and remand for a new trial. The charges in this case arose after the Commonwealth uncovered the ghastly acts of Dr. Kermit Gosnell at his abortion clinic. The Federal Bureau of Investigations (“FBI”), the Drug Enforcement Agency (“DEA”), and Philadelphia District Attorney’s Office detectives conducted a raid at Gosnell’s ____________________________________________ * Retired Senior Judge assigned to the Superior Court. J-A21004-14 abortion clinic, the Women’s Medical Society Clinic, on February 18, 2010. The investigation was largely focused on Gosnell’s alleged illegal issuance of prescription medication and performance of illegal abortions. As a result of the investigation, law enforcement uncovered the deaths of born-alive infants and one mother during a botched abortion. The Commonwealth charged Gosnell with seven counts of first-degree murder based on the deaths of seven newborn infants, and third degree murder in the death of Karnamaya Mongar.1 In addition, the Commonwealth charged Gosnell with conspiracy to commit murder, Abortion Act violations, corrupt organizations and other crimes. -

District of Columbia Pain-Capable Unborn Child Protection Act Hearing Committee on the Judiciary House of Representatives
DISTRICT OF COLUMBIA PAIN-CAPABLE UNBORN CHILD PROTECTION ACT HEARING BEFORE THE SUBCOMMITTEE ON THE CONSTITUTION AND CIVIL JUSTICE OF THE COMMITTEE ON THE JUDICIARY HOUSE OF REPRESENTATIVES ONE HUNDRED THIRTEENTH CONGRESS FIRST SESSION ON H.R. 1797 MAY 23, 2013 Serial No. 113–19 Printed for the use of the Committee on the Judiciary ( Available via the World Wide Web: http://judiciary.house.gov U.S. GOVERNMENT PRINTING OFFICE 81–175 PDF WASHINGTON : 2013 For sale by the Superintendent of Documents, U.S. Government Printing Office Internet: bookstore.gpo.gov Phone: toll free (866) 512–1800; DC area (202) 512–1800 Fax: (202) 512–2104 Mail: Stop IDCC, Washington, DC 20402–0001 COMMITTEE ON THE JUDICIARY BOB GOODLATTE, Virginia, Chairman F. JAMES SENSENBRENNER, JR., JOHN CONYERS, JR., Michigan Wisconsin JERROLD NADLER, New York HOWARD COBLE, North Carolina ROBERT C. ‘‘BOBBY’’ SCOTT, Virginia LAMAR SMITH, Texas MELVIN L. WATT, North Carolina STEVE CHABOT, Ohio ZOE LOFGREN, California SPENCER BACHUS, Alabama SHEILA JACKSON LEE, Texas DARRELL E. ISSA, California STEVE COHEN, Tennessee J. RANDY FORBES, Virginia HENRY C. ‘‘HANK’’ JOHNSON, JR., STEVE KING, Iowa Georgia TRENT FRANKS, Arizona PEDRO R. PIERLUISI, Puerto Rico LOUIE GOHMERT, Texas JUDY CHU, California JIM JORDAN, Ohio TED DEUTCH, Florida TED POE, Texas LUIS V. GUTIERREZ, Illinois JASON CHAFFETZ, Utah KAREN BASS, California TOM MARINO, Pennsylvania CEDRIC RICHMOND, Louisiana TREY GOWDY, South Carolina SUZAN DelBENE, Washington MARK AMODEI, Nevada JOE GARCIA, Florida RAU´ L LABRADOR, Idaho HAKEEM JEFFRIES, New York BLAKE FARENTHOLD, Texas GEORGE HOLDING, North Carolina DOUG COLLINS, Georgia RON DeSANTIS, Florida [Vacant] SHELLEY HUSBAND, Chief of Staff & General Counsel PERRY APELBAUM, Minority Staff Director & Chief Counsel SUBCOMMITTEE ON THE CONSTITUTION AND CIVIL JUSTICE TRENT FRANKS, Arizona, Chairman JIM JORDAN, Ohio, Vice-Chairman STEVE CHABOT, Ohio JERROLD NADLER, New York J. -

The Life Battle Celebrating and Building on S353
FNC | spotlight The Life Battle Celebrating and Building on S353 he first thing she said to me was, For years, efforts have been made to stop the ho- ‘I know it’s a girl and I need your locaust of abortion. Yet, these two recent accounts, “ help to get it out of me.…’ With the first regarding a sex-selection abortion and the written by: her arms tightly crossed along second a chemical abortion, show how much work Mary her abdomen, she explained that still remains. her husband and his parents expected a boy, In the waning hours of the 2013 Legislative and that Carpenter’s help could change her Summa, Session, North Carolina lawmakers passed what life. ‘I have a daughter,’ Priya said. ‘I don’t J.D. T 1 constitutes one of the few pieces of meaningful pro- need another one.’” life legislation enacted in this State in the past 100 “I first heard of the mifepristone abortion years.3 Upon signing this bill into law, Governor Pat pill, on September 17, 2003, the worst day of McCrory underscored that, in his mind, the law was my life. A nurse told me my daughter, Holly, about insuring safer conditions for women seeking was in the hospital and in very serious condi- abortion.4 While that is a laudable goal we should tion. I asked, ‘What is wrong?’ She responded, all support, we must also recognize that abortion ‘Mr. Patterson, we’ll explain when you get directly impacts two lives: the life of the mother and here … come as quickly as you can.’ I sped to the life of the unborn child.