2021 Committee Roster & Committee Descriptions
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

2020 SWPONL Conference First Name Middle Last Name Degrees
2020 SWPONL Conference First name Middle Last name Degrees/Credentials Job Title Hospital / Company City, State Tammy Allison MSN, DNP Clinical Director, Education The Uniontown Hospital Uniontown, PA Heather Ambrose DNP, RN, NEA-BC, CPN Director of Nursing UPMC Presbyterian Shadyside Pittsburgh, PA Daniela Angeloni Infermiera CNO UPMC Salvator Mundi Roma, Italy Joe Archer MS, BS, RRT Territory Manager BD/BARD Pittsburgh, PA Amanda Barker Monitoring Sales Specialist Medtronic Pittsburgh, PA Lee Baron MSN, RN Assistant Vice President, Nursing Monongahela Valley Hospital Monongahela, PA Kim Bartolowits RN, MSN, NE-BC Magnet Program Director Allegheny General Hospital/AHN Pittsburgh, PA Deborah Beer DNP, RN-BC,CNE Director, Clinical & Operational UPMC Western Psychiatric Hospital Pittsburgh, PA Informatics Kimberly Belton MSN, RN Nurse Manager Allegheny General Hospital/AHN Pittsburgh, PA Janet Bischof PhD RN NE-BC CNE Director/Associate Professor Wheeling University Wheeling, WV Jodie M Blaha RN, MSN Unit Director UPMC Pittsburgh PA Jeffrey R Bomba MBA, MSN, RN, NE-BC Patient Care Manager AHN Jefferson Hospital Jefferson Hills, PA Karen Bray RN, MSN Vice-President, Patient Care Washington Health System Washington, PA Services Amy Bridgman MSN, RN-BC, CPN Advanced Clinical Education UPMC Children's Hospital of Pittsburgh Aliquippa, PA Specialist Kimberly Brooks DNP, RN Director, Education/Magnet UPMC Magee-Womens Hospital Pittsburgh, PA 2020 SWPONL Conference Angela Brown RN, MSN, CCRN Nurse Manager Allegheny General Hospital/AHN Pittsburgh, PA Kristie Bruner MSN, RN, NE-BC Nurse Manager Allegheny General Hospital/AHN Pittsburgh, PA Lisa M Bryan-Morris MSN, RN, NEA-BC Chief Nursing Officer UPMC Passavant Hospital Pittsburgh, PA Helen Burns PhD, RN, NEA-BC, FAAN Senior Vice President and Chief Excela Health Greensburg, PA Nursing Officer Diane M. -

Most UPMC Hospitals and Other Facilities in Western Pennsylvania Will Be Out-Of-Network for Patients with Highmark Commercial Insurance After June 30, 2019
Most UPMC hospitals and other facilities in western Pennsylvania will be out-of-network for patients with Highmark commercial insurance after June 30, 2019. Below are answers to frequently asked questions about how your health care will be impacted. Q: Will UPMC Hamot be out-of-network after June 30, 2019? A: Yes, UPMC Hamot will be out-of-network for Highmark commercial members after June 30, 2019. Q: Will UPMC doctors be out-of-network after June 30, 2019? A: Yes, most UPMC doctors in Erie will be out-of-network for Highmark commercial members after June 30, 2019. Additionally, if you would like to see a UPMC doctor at, or near, another UPMC hospital or facility that will be out-of-network after June 30, 2019, you can expect that doctor to be out-of-network for you as well. Q: Will any UPMC specialty services be in-network for Highmark commercial members in western Pa. after June 30, 2019? A: Yes, in addition to Children’s Hospital of Pittsburgh of UPMC and Western Psychiatric Institute and Clinic of UPMC, a very limited number of UPMC specialty services will be in-network for Highmark commercial members in western Pennsylvania after June 30, 2019. Q: Will I have access to UPMC Hillman Cancer Center after June 30, 2019? A: No, Highmark commercial members will not have in-network access to UPMC Hillman Cancer Center services at UPMC Hamot, including clinical trials, after June 30, 2019. Q: How do I know if I have commercial insurance? A: Commercial health insurance policies often are provided as part of a group plan, such as through an employer or union. -

PPC-Infographic.Pdf
Celebrating our 15th anniversary, Partnership for Patient Care (PPC) is the region’s premier patient safety and quality program driving health equity and high quality outcomes. 115th5th Anniversary 2006 – 2021 WHAT IS PARTNERSHIP FOR PATIENT CARE? Partnership for Patient Care (PPC) is a collaboration between Independence Blue Cross, Health Care Improvement Foundation and the region’s leading healthcare organizations and stakeholders to accelerate the adoption of evidence-based clinical best practices. PPC’s improvement efforts have enabled the region to foster partnerships among organizations that share a common desire for providing the safest and highest quality care to patients. PPC serves as an umbrella, under which several programs have been established during the past 15 years to support ongoing regional improvement. PPC PROGRAMS Health Equity Data Strategy (HEDS) NEW New in 2021, HEDS is a regional collaborative aimed at decreasing disparities in health outcomes with a focus on establishing recommendations for the implementation of a health equity data strategy. This program will support organizations in the accurate and reliable collection of REaL (ethnicity, and language) data, utilization of the data to evaluate health outcomes, identification of disparities across populations and health conditions; and implementation of targeted quality improvement strategies that promote health equity. Safety Forum 100% A forum of front-line patient safety leaders from hospitals across Southeastern PA that of participants rated promotes interactive discussions about safety hazards and vulnerabilities and a peer- the program as very good or excellent to-peer exchange of patient safety approaches, processes, and best practices. Pennsylvania Urologic Regional Collaborative (PURC) 142 PURC is a quality improvement initiative that brings urology practices together in a physician- participating physicians led, data-sharing and improvement collaborative aimed at advancing the quality of diagnosis 17,000+ and care for men with prostate cancer. -
UPMC Year End Financial and Operating Report & Audited
UPMC Year End Financial and Operating Report & Audited Consolidated Financial Statements FOR THE PERIOD ENDED DECEMBER 31, 2020 UPMC YEAR END FINANCIAL AND OPERATING REPORT • DECEMBER 2020 | UPMC Year End Financial and Operating Report & Audited Consolidated Financial Statements FOR THE PERIOD ENDED DECEMBER 31, 2020 TABLE OF CONTENTS Introduction to Management’s Discussion and Analysis ............................... 1 Management’s Discussion and Analysis ........................................ 2 Consolidated Financial Highlights .......................................... 3 Business Highlights .................................................. 4 Condensed Consolidating Statements of Operations ............................... 6 Divisional Information ................................................... 7 Revenue and Operating Metrics ............................................. 9 Key Financial Indicators ................................................. 12 Market Share ....................................................... 13 Asset and Liability Management ............................................ 14 Utilization Statistics ................................................... 16 Outstanding Debt .................................................... 17 Debt Covenant Calculations .............................................. 18 Audited Consolidated Financial Statements ..................................... 19 Report of Independent Registered Public Accounting Firm ........................... 20 Consolidated Balance Sheets .......................................... -

Tobacco Settlement Report: FY 2017-18
THE TOBACCO SETTLEMENT ANNUAL REPORT TO THE GENERAL ASSEMBLY JULY 1, 2017 – JUNE 30, 2018 Tom Wolf Teresa D. Miller Governor Secretary of Human Services THE TOBACCO SETTLEMENT ANNUAL REPORT TO THE GENERAL ASSEMBLY JULY 1, 2017 – June 30, 2018 Page Executive Summary 3 Uncompensated Care for Hospitals (2017-2018) 4 Attachment 1 – Hospitals eligible for tobacco payment 7 Attachment 2 – Hospitals qualified to receive UC payments 12 Attachment 3 – Hospitals qualified to receive EE payments 16 Attachment 4 – Hospitals affiliations for tobacco payments 19 Attachment 5 – Hospitals with potential DSH-UPL issues 24 Attachment 6 – Total expenditures for each fiscal year 25 Attachment 7 – Uncompensated care (UC) payment method 28 Home and Community-Based Services to Older Pennsylvanians 30 Chart 1 - Aging Waiver Allocation Direct Service Costs 31 Table 1 - Summary of the Aging Waiver 32 Table 2 - Number of Applicants 33 Table 3 - Funded Individuals (Aging Waiver Program) 35 Table 4 - Total Expenditure by PSA 37 Table 5 - Aging Waiver Costs, Number of Claims and Consumers by Service Category for Fiscal Year 2017-2018 39 Table 6 - Costs, Number of Claims and Number of Unduplicated Consumers by Service Category for FY 2017-2018 40 Table 7 - Average State and Federal Costs per Individual 40 Medical Assistance for Workers with Disabilities (MAWD) 41 2 EXECUTIVE SUMMARY The Commonwealth of Pennsylvania joined 45 other states in November 1998 in a master settlement agreement (MSA) with the tobacco industry, estimated to total $206 billion over the first 25 years. Pennsylvania’s share was estimated to be about $11 billion between the years 2000 and 2025. -
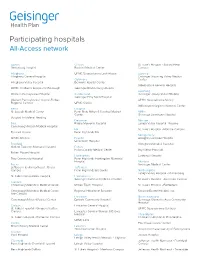
Participating Hospitals All-Access Network
Participating hospitals All-Access network Adams Clinton St. Luke’s Hospital - Sacred Heart Gettysburg Hospital Bucktail Medical Center Campus Allegheny UPMC Susquehanna Lock Haven Luzerne Allegheny General Hospital Geisinger Wyoming Valley Medical Columbia Center Allegheny Valley Hospital Berwick Hospital Center Wilkes-Barre General Hospital UPMC Children’s Hospital of Pittsburgh Geisinger Bloomsburg Hospital Lycoming Western Pennsylvania Hospital Cumberland Geisinger Jersey Shore Hospital Geisinger Holy Spirit Hospital Western Pennsylvania Hospital-Forbes UPMC Susquehanna Muncy Regional Campus UPMC Carlisle Williamsport Regional Medical Center Berks Dauphin St. Joseph Medical Center Penn State Milton S Hershey Medical Mifflin Center Geisinger Lewistown Hospital Surgical Institute of Reading Delaware Monroe Blair Riddle Memorial Hospital Lehigh Valley Hospital - Pocono Conemaugh Nason Medical Hospital Elk St. Luke’s Hospital - Monroe Campus Tyrone Hospital Penn Highlands Elk Montgomery UPMC Altoona Fayette Abington Lansdale Hospital Uniontown Hospital Bradford Abington Memorial Hospital Guthrie Towanda Memorial Hospital Fulton Fulton County Medical Center Bryn Mawr Hospital Robert Packer Hospital Huntingdon Lankenau Hospital Troy Community Hospital Penn Highlands Huntingdon Memorial Hospital Montour Bucks Geisinger Medical Center Jefferson Health Northeast - Bucks Jefferson Campus Penn Highlands Brookville Northampton Lehigh Valley Hospital - Muhlenberg St. Luke's Quakertown Hospital Lackawanna Geisinger Community Medical Center St. Luke’s Hospital - Anderson Campus Cambria Conemaugh Memorial Medical Center Moses Taylor Hospital St. Luke’s Hospital - Bethlehem Conemaugh Memorial Medical Center - Regional Hospital of Scranton Steward Easton Hospital, Inc. Lee Campus Lancaster Northumberland Conemaugh Miners Medical Center Ephrata Community Hospital Geisinger Shamokin Area Community Hospital Carbon Lancaster General Hospital St. Luke’s Hospital - Gnaden Huetten UPMC Susquehanna Sunbury Campus Lancaster General Women & Babies Hospital Philadelphia St. -

Employee Handbook
Employee Handbook You and Jefferson Thomas Jefferson University & Hospitals Stephen K. Klasko, MD, MBA President and CEO Thomas Jefferson University and Jefferson Health System Dear Colleague, Welcome to Thomas Jefferson University and Hospitals! In accepting your new position, you have joined a team committed to redefining healthcare. With a robust history and community roots dating back to 1824, Jefferson is a nationally influential and widely respected academic medical center. We deliver high quality, personalized and compassionate care, and you are now a vital part of our tradition of excellence. By selecting Jefferson, you will enjoy competitive pay, a broad selection of employee benefits from which to choose, opportunity for educational and developmental growth, and a challenging and interactive work environment. Congratulations and my best wishes as you assume your new responsibilities at Jefferson. Sincerely, Stephen K. Klasko, MD, MBA President and CEO Thomas Jefferson University and Jefferson Health System About This Handbook This employee handbook has been designed to provide you with general information about various policies, benefits, services and facilities of Jefferson which may be of interest to you in the course of your employment. Please understand that it only highlights these topics. More specific information may be obtained from your supervisor, the hospital intranet, where any specific policies cited here may be found or the Department of Human Resources at Suite 2150 Gibbon Building or Methodist Administration Suite. You are strongly encouraged to become acquainted with all Jefferson policies and procedures to make your employment as satisfying and productive as possible. The policies, procedures and benefits described in this handbook are not all-inclusive and may be amended or rescinded from time to time at the discretion of Jefferson, with or without notice. -

LVBCH Newsletter
Volume 14 No 4 Winter 2018/2019 President’s Message by Carl Seitz As I write this letter, it is late December – the time when we reflect on the past year’s accomplishments and plan for the new year. For 2018, Coalition activity and accomplishments included: • Coalition membership reaching 220 members. • Capital BlueCross and Geisinger Health Plan named as Medical Plan Partners for 2019-2021. • The 38th Annual Conference held May 3 with a record 259 attendees, 30 sponsors/exhibitors, and feedback regarding the high energy level of the event. • Partnering with the NEPA MAEA to expand our market area and bring our purchasing programs to their members. • Hosting Leah Binder, President/CEO of the Leapfrog Group, as she toured Lehigh Valley Health Network’s Muhlenberg Campus and St. Luke’s University Health Network’s Bethlehem Campus. During her visit, we also screened the documentary, “To Err is Human” with a panel discussion regarding medical errors. • Holding the inaugural Associates Showcase, which spotlighted five of the Coalition’s Associate Members: AblePay Health, Benefitfocus, ConsumerMedical, Health Advocate and Trividia Health. In 2019, I ask you to include the Coalition in your plans by doing at least one of the following: • Attend the Coalition’s 39th Annual Conference at DeSales University on May 2, 2019. • Join one of the Coalition’s Committees: Membership, Quality, Purchasing, or Data. • Attend a member education program. • Bring a colleague from a non-member employer to a Coalition event and encourage them to have their company join the Coalition. • Meet with Donna Corsi, our Director of Member Programs and Services, to learn more about the Coalition, our purchasing programs, and ways to engage in the Coalition. -
Restructuring the MLH/Jefferson Partnership
Main Line Health Physician Restructuring the MLH/Jefferson partnership Surviving Sepsis: The future of Hepatology: SUMMER 2014 ED success moves health care at From Hep C to Inside: to inpatient Exton Square Mall transplant care Main Line Health Physician Medical staff education initiative BY ANGUS GILLIS, MD The Main Line Health medical staff structure is an integrated model that encompasses private practice MESSAGES | 2 physicians who are on staff, hospital-employed physicians, and physicians/physician groups who are under contract for provision of services to the Hospital System. Medical staff functions have traditionally included initial credentialing, reappointment, and approval of privileges for new procedures. Tools used to fulfill these tasks include focused and ongoing professional practice evaluation (FPPE and OPPE). The staff is responsible for peer review, including case study and quality concerns. By-law and policy issues such as investigations, interventions, confidentiality, and physician rights are also areas in which the medical staff is involved. The staff has administrative functions related to patient safety, infection control, pharmacy and therapeutics, medical records, and behavioral issues like disruptive behavior and practitioner health. This is only a partial list of the responsibilities of the medical staff. Ultimate responsibility for approval and implementation of any recommendations by the staff’s Medical Executive Committee lies with the Board of Main Line Health. In addition to the above functions, the medical staff also takes an active role in continuing medical education. Your medical staff dues have always funded clinical educational efforts, such as Grand Rounds, at our various locations. A new additional effort is the Medical Executive Committee’s budgeting of dedicated monies for physician education, which will enable members to carry out these medical staff responsibilities. -

Designated Acute Care Hospital Stroke Centers 180424
Acute Stroke -ready; Comprehensive stroke COUNTY FACILITY NAME CITY ZIP Center or Primary Stroke Center? MONTGOMERY Abington Memorial Hospital Comprehensive stroke Center Abington 19001 ALLEGHENY Allegheny General Hospital Comprehensive Stroke Center Pittsburgh 15212 CUMBERLAND Carlisle Regional Medical Center Primary Stroke Center Carlisle 17015 FRANKLIN Chambersburg Hospital Primary Stroke Center Chambersburg 17201 CHESTER Chester County Hospital – Chester County Primary Stroke Center West Chester 19380 CAMBRIA Conemaugh Memorial Medical Center Primary Stroke Center Johnstown 15905 BLAIR Conemaugh Nason Medical Center Acute Stroke -ready Roaring Spring 16673 BUCKS Doylestown Hospital Primary Stroke Center Doylestown 18901 MONTGOMERY Einstein Medical Center Montgomery Primary Stroke Center East Norriton 19403 LANCASTER Ephrata Community Hospital Primary Stroke Center Ephrata 17522 WESTMORELAND Excela Health Frick Hospital Primary Stroke Center Westmoreland 15666 WESTMORELAND Excela Health Latrobe Hospital Primary Stroke Center Latrobe 15650 WESTMORELAND Excela Health Westmoreland Hospital Primary Stroke Center Greensburg 15601 LACKAWANNA Geisinger Community Medical Center – Scranton - Lackawanna County Primary Stroke Center Scranton 18510 MONTOUR Geisinger Medical Center – Montour County Primary Stroke Center Danville 17822 LUZERNE Geisinger Wyoming Valley Medical Center, Wilkes-Barre – Luzerne County Primary Stroke Center Wilkes Barre 18711 ADAMS Gettysburg Hospital Primary Stroke Center Gettysburg 17325 CARBON Gnadden Huetten Memorial -

HMO Proactive Tiered Network Hospital List
Save with Keystone HMO Proactive, our most popular plans Keystone HMO Proactive health plans are our most popular for good reason: You get access to high-quality care and save money. Not only do you pay less for your monthly premiums, but you can save even more by choosing doctors and hospitals in Tier 1 – Preferred. Save with Tier 1 – Preferred Tier 1 – Preferred includes more than 50 percent of the network. Keystone HMO Proactive offers the same essential health benefits as our other health plans, including doctor visits, Tier 1 – Preferred hospital stays, prescription drug coverage, blood tests, and X-rays. The difference is its tiered provider network, which gives you the option to pay less for care by choosing Tier 1 –Preferred providers. Here are the most important things to know about Keystone HMO Proactive: • You can visit any doctor or hospital in the Independence Blue Cross network once you have a referral. Tier 2 – Enhanced Tier 3 – Standard • You will select a PCP to coordinate your care and refer you to specialists. • Some services cost the same no matter what provider you Save even more choose — like preventive care, emergency room visits, and Keystone HMO Silver Proactive Select and Keystone HMO Silver urgent care. Proactive Value: These lower-premium options are only available • When you use doctors and hospitals in Tier 1 – Preferred, when you purchase directly from Independence Blue Cross. you pay the lowest out-of-pocket costs. Keystone HMO Silver Proactive Value includes a deductible for • The choice is always yours. You can choose Tier 1 providers Tiers 1 – 3 for some services. -

2005 Most Wired Survey and Benchmarking Study
2012 Most Wired Survey Winners by State Alabama Cullman Regional Medical Center: Innovator Award winner Evergreen Medical Center: Most Wired–Small and Rural St. Vincent’s Hospital–Birmingham: Most Wired University of Alabama at Birmingham (UAB) Hospital: Most Wired Washington County Hospital, Chatom: Most Wired–Small and Rural Arizona Banner Health, Phoenix: Most Wired Tucson Medical Center: Most Wired Arkansas Stone County Medical Center, Mountain View: Most Wired–Small and Rural California Eisenhower Medical Center, Rancho Mirage: Most Wired Kaiser Permanente, Oakland: Most Improved Naval Hospital Lemoore: Most Wired–Small and Rural Rady Children's Hospital–San Diego: Most Wired San Francisco VA Medical Center: Most Wired Sharp HealthCare, San Diego: Most Wired Stanford Hospital and Clinics: Most Wired University of California Davis Health System, Sacramento: Most Wired University of California, San Diego Health System: Most Wired VA Palo Alto Health Care System: Most Wired VA Sierra Pacific Network, Mare Island: Most Wired Colorado Denver Health and Hospital Authority: Most Wired Poudre Valley Health System, Fort Collins: Most Wired Connecticut Hartford Hospital: Most Wired Middlesex Health System, Middletown: Most Wired MidState Medical Center, Meriden: Most Wired Saint Francis Care, Hartford: Most Wired William W. Backus Hospital, Norwich: Most Wired Yale New Haven Health System: Most Wired Delaware Alfred I. duPont Hospital for Children, Wilmington: Most Wired District of Columbia Washington, D.C. VA Medical Center: Most Wired Florida