Procoagulatory Changes Induced by Head-Up Tilt Test in Patients with Syncope: Observational Study
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Hemoglobin Interaction with Gp1ba Induces Platelet Activation And
ARTICLE Platelet Biology & its Disorders Hemoglobin interaction with GP1bα induces platelet activation and apoptosis: a novel mechanism associated with intravascular hemolysis Rashi Singhal,1,2,* Gowtham K. Annarapu,1,2,* Ankita Pandey,1 Sheetal Chawla,1 Amrita Ojha,1 Avinash Gupta,1 Miguel A. Cruz,3 Tulika Seth4 and Prasenjit Guchhait1 1Disease Biology Laboratory, Regional Centre for Biotechnology, National Capital Region, Biotech Science Cluster, Faridabad, India; 2Biotechnology Department, Manipal University, Manipal, Karnataka, India; 3Thrombosis Research Division, Baylor College of Medicine, Houston, TX, USA, and 4Hematology, All India Institute of Medical Sciences, New Delhi, India *RS and GKA contributed equally to this work. ABSTRACT Intravascular hemolysis increases the risk of hypercoagulation and thrombosis in hemolytic disorders. Our study shows a novel mechanism by which extracellular hemoglobin directly affects platelet activation. The binding of Hb to glycoprotein1bα activates platelets. Lower concentrations of Hb (0.37-3 mM) significantly increase the phos- phorylation of signaling adapter proteins, such as Lyn, PI3K, AKT, and ERK, and promote platelet aggregation in vitro. Higher concentrations of Hb (3-6 mM) activate the pro-apoptotic proteins Bak, Bax, cytochrome c, caspase-9 and caspase-3, and increase platelet clot formation. Increased plasma Hb activates platelets and promotes their apoptosis, and plays a crucial role in the pathogenesis of aggregation and development of the procoagulant state in hemolytic disorders. Furthermore, we show that in patients with paroxysmal nocturnal hemoglobinuria, a chronic hemolytic disease characterized by recurrent events of intravascular thrombosis and thromboembolism, it is the elevated plasma Hb or platelet surface bound Hb that positively correlates with platelet activation. -

Common Gene Polymorphisms Associated with Thrombophilia
Chapter 5 Common Gene Polymorphisms Associated with Thrombophilia Christos Yapijakis, Zoe Serefoglou and Constantinos Voumvourakis Additional information is available at the end of the chapter http://dx.doi.org/10.5772/61859 Abstract Genetic association studies have revealed a correlation between DNA variations in genes encoding factors of the hemostatic system and thrombosis-related disease. Certain var‐ iant alleles of these genes that affect either gene expression or function of encoded protein are known to be genetic risk factors for thrombophilia. The chapter presents the current genetics and molecular biology knowledge of the most important DNA polymorphisms in thrombosis-related genes encoding coagulation factor V (FV), coagulation factor II (FII), coagulation factor XII (FXII), coagulation factor XIII A1 subunit (FXIIIA1), 5,10- methylene tetrahydrofolate reductase (MTHFR), serpine1 (SERPINE1), angiotensin I-con‐ verting enzyme (ACE), angiotensinogen (AGT), integrin A2 (ITGA2), plasma carboxypeptidase B2 (CPB2), platelet glycoprotein Ib α polypeptide (GP1BA), thrombo‐ modulin (THBD) and protein Z (PROZ). The molecular detection methods of each DNA polymorphism is presented, in addition to the current knowledge regarding its influence on thrombophilia and related thrombotic events, including stroke, myocardial infarction, deep vein thrombosis, spontaneous abortion, etc. In addition, best thrombosis prevention strategies with a combination of genetic counseling and molecular testing are discussed. Keywords: Thrombophilia, coagulation -

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -
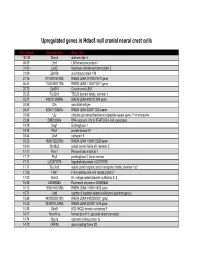
Supp Table 1.Pdf
Upregulated genes in Hdac8 null cranial neural crest cells fold change Gene Symbol Gene Title 134.39 Stmn4 stathmin-like 4 46.05 Lhx1 LIM homeobox protein 1 31.45 Lect2 leukocyte cell-derived chemotaxin 2 31.09 Zfp108 zinc finger protein 108 27.74 0710007G10Rik RIKEN cDNA 0710007G10 gene 26.31 1700019O17Rik RIKEN cDNA 1700019O17 gene 25.72 Cyb561 Cytochrome b-561 25.35 Tsc22d1 TSC22 domain family, member 1 25.27 4921513I08Rik RIKEN cDNA 4921513I08 gene 24.58 Ofa oncofetal antigen 24.47 B230112I24Rik RIKEN cDNA B230112I24 gene 23.86 Uty ubiquitously transcribed tetratricopeptide repeat gene, Y chromosome 22.84 D8Ertd268e DNA segment, Chr 8, ERATO Doi 268, expressed 19.78 Dag1 Dystroglycan 1 19.74 Pkn1 protein kinase N1 18.64 Cts8 cathepsin 8 18.23 1500012D20Rik RIKEN cDNA 1500012D20 gene 18.09 Slc43a2 solute carrier family 43, member 2 17.17 Pcm1 Pericentriolar material 1 17.17 Prg2 proteoglycan 2, bone marrow 17.11 LOC671579 hypothetical protein LOC671579 17.11 Slco1a5 solute carrier organic anion transporter family, member 1a5 17.02 Fbxl7 F-box and leucine-rich repeat protein 7 17.02 Kcns2 K+ voltage-gated channel, subfamily S, 2 16.93 AW493845 Expressed sequence AW493845 16.12 1600014K23Rik RIKEN cDNA 1600014K23 gene 15.71 Cst8 cystatin 8 (cystatin-related epididymal spermatogenic) 15.68 4922502D21Rik RIKEN cDNA 4922502D21 gene 15.32 2810011L19Rik RIKEN cDNA 2810011L19 gene 15.08 Btbd9 BTB (POZ) domain containing 9 14.77 Hoxa11os homeo box A11, opposite strand transcript 14.74 Obp1a odorant binding protein Ia 14.72 ORF28 open reading -

Therapeutic Antibody-Like Immunoconjugates Against Tissue Factor with the Potential to Treat Angiogenesis-Dependent As Well As Macrophage-Associated Human Diseases
antibodies Review Therapeutic Antibody-Like Immunoconjugates against Tissue Factor with the Potential to Treat Angiogenesis-Dependent as Well as Macrophage-Associated Human Diseases Zhiwei Hu ID Department of Surgery Division of Surgical Oncology, The James Comprehensive Cancer Center, The Ohio State University College of Medicine, Columbus, OH 43210, USA; [email protected]; Tel.: +1-614-685-4606 Received: 10 October 2017; Accepted: 18 January 2018; Published: 23 January 2018 Abstract: Accumulating evidence suggests that tissue factor (TF) is selectively expressed in pathological angiogenesis-dependent as well as macrophage-associated human diseases. Pathological angiogenesis, the formation of neovasculature, is involved in many clinically significant human diseases, notably cancer, age-related macular degeneration (AMD), endometriosis and rheumatoid arthritis (RA). Macrophage is involved in the progression of a variety of human diseases, such as atherosclerosis and viral infections (human immunodeficiency virus, HIV and Ebola). It is well documented that TF is selectively expressed on angiogenic vascular endothelial cells (VECs) in these pathological angiogenesis-dependent human diseases and on disease-associated macrophages. Under physiology condition, TF is not expressed by quiescent VECs and monocytes but is solely restricted on some cells (such as pericytes) that are located outside of blood circulation and the inner layer of blood vessel walls. Here, we summarize TF expression on angiogenic VECs, macrophages and other diseased cell types in these human diseases. In cancer, for example, the cancer cells also overexpress TF in solid cancers and leukemia. Moreover, our group recently reported that TF is also expressed by cancer-initiating stem cells (CSCs) and can serve as a novel oncotarget for eradication of CSCs without drug resistance. -

Cellular and Molecular Signatures in the Disease Tissue of Early
Cellular and Molecular Signatures in the Disease Tissue of Early Rheumatoid Arthritis Stratify Clinical Response to csDMARD-Therapy and Predict Radiographic Progression Frances Humby1,* Myles Lewis1,* Nandhini Ramamoorthi2, Jason Hackney3, Michael Barnes1, Michele Bombardieri1, Francesca Setiadi2, Stephen Kelly1, Fabiola Bene1, Maria di Cicco1, Sudeh Riahi1, Vidalba Rocher-Ros1, Nora Ng1, Ilias Lazorou1, Rebecca E. Hands1, Desiree van der Heijde4, Robert Landewé5, Annette van der Helm-van Mil4, Alberto Cauli6, Iain B. McInnes7, Christopher D. Buckley8, Ernest Choy9, Peter Taylor10, Michael J. Townsend2 & Costantino Pitzalis1 1Centre for Experimental Medicine and Rheumatology, William Harvey Research Institute, Barts and The London School of Medicine and Dentistry, Queen Mary University of London, Charterhouse Square, London EC1M 6BQ, UK. Departments of 2Biomarker Discovery OMNI, 3Bioinformatics and Computational Biology, Genentech Research and Early Development, South San Francisco, California 94080 USA 4Department of Rheumatology, Leiden University Medical Center, The Netherlands 5Department of Clinical Immunology & Rheumatology, Amsterdam Rheumatology & Immunology Center, Amsterdam, The Netherlands 6Rheumatology Unit, Department of Medical Sciences, Policlinico of the University of Cagliari, Cagliari, Italy 7Institute of Infection, Immunity and Inflammation, University of Glasgow, Glasgow G12 8TA, UK 8Rheumatology Research Group, Institute of Inflammation and Ageing (IIA), University of Birmingham, Birmingham B15 2WB, UK 9Institute of -

Alternatively Spliced Tissue Factor Induces Angiogenesis Through Integrin Ligation
Alternatively spliced tissue factor induces angiogenesis through integrin ligation Y. W. van den Berga, L. G. van den Hengela, H. R. Myersa, O. Ayachia, E. Jordanovab, W. Rufc, C. A. Spekd, P. H. Reitsmaa, V. Y. Bogdanove, and H. H. Versteega,1 aThe Einthoven Laboratory for Experimental Vascular Medicine and bDepartment of Pathology, Leiden University Medical Center, Albinusdreef 2, 2333 ZA, Leiden, The Netherlands; cDepartment of Immunology and Microbial Science, The Scripps Research Institute, 10550 North Torrey Pines Road, La Jolla, CA 92037; dCenter for Experimental and Molecular Medicine, Academic Medical Center, Meibergdreef 9, 1105 AZ, Amsterdam, The Netherlands; and eDivision of Hematology/Oncology, Department of Internal Medicine, University of Cincinnati College of Medicine, 3125 Eden Avenue, Cincinnati, OH 45267 Edited by Charles T. Esmon, Oklahoma Medical Research Foundation, Oklahoma City, OK, and approved September 25, 2009 (received for review May 15, 2009) The initiator of coagulation, full-length tissue factor (flTF), in complex pancreatic cancer cells transfected to express asTF produce more with factor VIIa, influences angiogenesis through PAR-2. Recently, an blood vessels (20), but it remained mechanistically unclear if and alternatively spliced variant of TF (asTF) was discovered, in which part how angiogenesis is regulated by asTF. One possibility is that asTF of the TF extracellular domain, the transmembrane, and cytoplasmic stimulates cancer cells to produce angiogenic factors, but it is also domains are replaced by a unique C terminus. Subcutaneous tumors plausible that asTF enhances angiogenesis via paracrine stimulation produced by asTF-secreting cells revealed increased angiogenesis, but of endothelial cells. Moreover, the role of VIIa, PAR-2 activation it remained unclear if and how angiogenesis is regulated by asTF. -

Endotoxin Enhances Tissue Factor and Suppresses Thrombomodulin Expression of Human Vascular Endothelium in Vitro Kevin L
Endotoxin Enhances Tissue Factor and Suppresses Thrombomodulin Expression of Human Vascular Endothelium In Vitro Kevin L. Moore,* Sharon P. Andreoli,* Naomi L. Esmon,1 Charles T. Esmon,l and Nils U. Bang1l Department ofMedicine, Section ofHematology/Oncology,* and Department ofPediatrics, Section ofNephrology,t Indiana University School ofMedicine, Indianapolis, Indiana 46223; Oklahoma Medical Research Foundation,§ Oklahoma City, Oklahoma 73104; and Lilly Laboratory for Clinical Research,1' Indianapolis, Indiana 46202 Abstract to support the assembly of clotting factor complexes on their surfaces (13, 14). Endotoxemia is frequently associated clinically with disseminated Under physiologic conditions the thromboresistant properties intravascular coagulation (DIC); however, the mechanism of en- ofthe endothelium are predominant. In some pathological states, dotoxin action in vivo is unclear. Modulation of tissue factor however, this may not be the case. Gram-negative sepsis is fre- (TF) and thrombomodulin (TM) expression on the endothelial quently associated with varying degrees of disseminated intra- surface may be relevant pathophysiologic mechanisms. Stimu- vascular coagulation (DIC),' which is thought to be triggered by lation of human umbilical vein endothelial cells with endotoxin endotoxemia. The pathophysiology of DIC in gram-negative (1 ,ug/ml) increased surface TF activity from 1.52±0.84 to sepsis is complex and the mechanism(s) by which endotoxemia 11.89±8.12 mU/ml-106 cells at 6 h (n = 11) which returned to promotes intravascular coagulation in vivo is unclear. Recently, baseline by 24 h. Repeated stimulation at 24 h resulted in renewed reports by several investigators provide evidence that the throm- TF expression. Endotoxin (1 ,tg/ml) also caused a decrease in boresistance of the endothelial cell is diminished after exposure TM expression to 55.0±6.4% of control levels at 24 h (n = 10) to endotoxin in the absence of other cell types. -

63Rd Annual SSC Meeting, in Conjunction with the 2017 ISTH Congress in Berlin, Germany Meeting Minutes
63rd Annual SSC meeting, in conjunction with the 2017 ISTH Congress in Berlin, Germany Meeting Minutes Standing Committees Coagulation Standards Committee ............................................................... 3 Subcommittees Animal, Cellular and Molecular Models ........................................................ 5 Biorheology .................................................................................................. 7 Control of Anticoagulation ............................................................................ 10 Disseminated Intravascular Coagulation ...................................................... 12 Factor VIII, Factor IX and Rare Coagulation Disorders ................................ 14 Factor XI and the Contact System ................................................................ 19 Factor XIII and Fibrinogen ............................................................................ 21 Fibrinolysis ................................................................................................... 27 Genomics in Thrombosis and Hemostasis ................................................... 33 Hemostasis and Malignancy......................................................................... 46 Lupus Anticoagulant/Phospholipid Dependent Antibodies ........................... 49 Pediatric and Neonatal Hemostasis and Thrombosis ................................... 54 Perioperative Thrombosis and Hemostasis .................................................. 59 Plasma Coagulation Inhibitors ..................................................................... -

Confirmation of Pathogenic Mechanisms by SARS-Cov-2–Host
Messina et al. Cell Death and Disease (2021) 12:788 https://doi.org/10.1038/s41419-021-03881-8 Cell Death & Disease ARTICLE Open Access Looking for pathways related to COVID-19: confirmation of pathogenic mechanisms by SARS-CoV-2–host interactome Francesco Messina 1, Emanuela Giombini1, Chiara Montaldo1, Ashish Arunkumar Sharma2, Antonio Zoccoli3, Rafick-Pierre Sekaly2, Franco Locatelli4, Alimuddin Zumla5, Markus Maeurer6,7, Maria R. Capobianchi1, Francesco Nicola Lauria1 and Giuseppe Ippolito 1 Abstract In the last months, many studies have clearly described several mechanisms of SARS-CoV-2 infection at cell and tissue level, but the mechanisms of interaction between host and SARS-CoV-2, determining the grade of COVID-19 severity, are still unknown. We provide a network analysis on protein–protein interactions (PPI) between viral and host proteins to better identify host biological responses, induced by both whole proteome of SARS-CoV-2 and specific viral proteins. A host-virus interactome was inferred, applying an explorative algorithm (Random Walk with Restart, RWR) triggered by 28 proteins of SARS-CoV-2. The analysis of PPI allowed to estimate the distribution of SARS-CoV-2 proteins in the host cell. Interactome built around one single viral protein allowed to define a different response, underlining as ORF8 and ORF3a modulated cardiovascular diseases and pro-inflammatory pathways, respectively. Finally, the network-based approach highlighted a possible direct action of ORF3a and NS7b to enhancing Bradykinin Storm. This network-based representation of SARS-CoV-2 infection could be a framework for pathogenic evaluation of specific 1234567890():,; 1234567890():,; 1234567890():,; 1234567890():,; clinical outcomes. -

MALE Protein Name Accession Number Molecular Weight CP1 CP2 H1 H2 PDAC1 PDAC2 CP Mean H Mean PDAC Mean T-Test PDAC Vs. H T-Test
MALE t-test t-test Accession Molecular H PDAC PDAC vs. PDAC vs. Protein Name Number Weight CP1 CP2 H1 H2 PDAC1 PDAC2 CP Mean Mean Mean H CP PDAC/H PDAC/CP - 22 kDa protein IPI00219910 22 kDa 7 5 4 8 1 0 6 6 1 0.1126 0.0456 0.1 0.1 - Cold agglutinin FS-1 L-chain (Fragment) IPI00827773 12 kDa 32 39 34 26 53 57 36 30 55 0.0309 0.0388 1.8 1.5 - HRV Fab 027-VL (Fragment) IPI00827643 12 kDa 4 6 0 0 0 0 5 0 0 - 0.0574 - 0.0 - REV25-2 (Fragment) IPI00816794 15 kDa 8 12 5 7 8 9 10 6 8 0.2225 0.3844 1.3 0.8 A1BG Alpha-1B-glycoprotein precursor IPI00022895 54 kDa 115 109 106 112 111 100 112 109 105 0.6497 0.4138 1.0 0.9 A2M Alpha-2-macroglobulin precursor IPI00478003 163 kDa 62 63 86 72 14 18 63 79 16 0.0120 0.0019 0.2 0.3 ABCB1 Multidrug resistance protein 1 IPI00027481 141 kDa 41 46 23 26 52 64 43 25 58 0.0355 0.1660 2.4 1.3 ABHD14B Isoform 1 of Abhydrolase domain-containing proteinIPI00063827 14B 22 kDa 19 15 19 17 15 9 17 18 12 0.2502 0.3306 0.7 0.7 ABP1 Isoform 1 of Amiloride-sensitive amine oxidase [copper-containing]IPI00020982 precursor85 kDa 1 5 8 8 0 0 3 8 0 0.0001 0.2445 0.0 0.0 ACAN aggrecan isoform 2 precursor IPI00027377 250 kDa 38 30 17 28 34 24 34 22 29 0.4877 0.5109 1.3 0.8 ACE Isoform Somatic-1 of Angiotensin-converting enzyme, somaticIPI00437751 isoform precursor150 kDa 48 34 67 56 28 38 41 61 33 0.0600 0.4301 0.5 0.8 ACE2 Isoform 1 of Angiotensin-converting enzyme 2 precursorIPI00465187 92 kDa 11 16 20 30 4 5 13 25 5 0.0557 0.0847 0.2 0.4 ACO1 Cytoplasmic aconitate hydratase IPI00008485 98 kDa 2 2 0 0 0 0 2 0 0 - 0.0081 - 0.0 -
Tissue Factor Regulation, Signaling and Functions Beyond Coagulation with a Focus on Diabetes
Digital Comprehensive Summaries of Uppsala Dissertations from the Faculty of Medicine 1626 Tissue Factor regulation, signaling and functions beyond coagulation with a focus on diabetes DESIRÉE EDÉN ACTA UNIVERSITATIS UPSALIENSIS ISSN 1651-6206 ISBN 978-91-513-0842-5 UPPSALA urn:nbn:se:uu:diva-399599 2020 Dissertation presented at Uppsala University to be publicly examined in Enghoffsalen, Akademiska sjukhuset, ing. 50, Uppsala, Friday, 21 February 2020 at 13:15 for the degree of Doctor of Philosophy (Faculty of Medicine). The examination will be conducted in Swedish. Faculty examiner: Docent, Universitetslektor Sofia Ramström (Örebro Universitet, Institutionen för medicinska vetenskaper). Abstract Edén, D. 2020. Tissue Factor regulation, signaling and functions beyond coagulation with a focus on diabetes. Digital Comprehensive Summaries of Uppsala Dissertations from the Faculty of Medicine 1626. 65 pp. Uppsala: Acta Universitatis Upsaliensis. ISBN 978-91-513-0842-5. Background: Tissue factor (TF) is a 47 kDa transmembrane glycoprotein best known for initiating the coagulation cascade upon binding of its ligand FVIIa. Apart from its physiological role in coagulation, TF and TF/FVIIa signaling has proved to be involved in diseases such as diabetes, cancer and cardiovascular diseases. Biological functions coupled to TF/FVIIa signaling include diet-induced obesity, apoptosis, angiogenesis and migration. Aim: The aim of this thesis was to investigate the role of TF/FVIIa in cells of importance in diabetes, to further investigate the mechanism behind TF/FVIIa anti-apoptotic signaling in cancer cells and lastly to examine the regulation of TF expression in monocytes by micro RNAs (miRNA). Results: In paper I we found that TF/FVIIa signaling augments cytokine-induced beta cell death and impairs glucose stimulated insulin secretion from human pancreatic islets.