House of Representatives Study Committee on Maternal Mortality
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Supplemental Statement OMB NO
Received by NSD/FARA Registration Unit 06/05/2012 11:27:24 AM U.S. Department of Justice Supplemental Statement OMB NO. 1124-0002 Washington, DC 20530 Pursuant to Section 2 ofthe Foreign Agents Registration Act of 1938, as amended For Six Month Period Ending April 30, 2012 ; (Insert date) I - REGISTRANT 1. (a) Name of Registrant (b) Registration No. Nelson Mullins Riley & Scarborough LLP 5928 (c) Business Address(es) of Registrant 1320 Main Street, 17th Floor, Columbia, SC 29201 2. Has there been a change in the information previously furnished in connection with the following (a) If an individual: (1) Residence address(es) Yes • No Ex] (2) Citizenship Yes • No [3 (3) Occupation Yes • No [x] (b) If an organization: (1) Name Yes • No H (2) Ownership or control Yes • No 0 (3) Branch offices Yes • No [3 (c) Explain fully all changes, if any, indicated in items (a) and (b) above. IF THE REGISTRANT IS AN INDIVIDUAL, OMIT RESPONSE TO ITEMS 3, 4 AND 5(a). 3. If you have previously filed Exhibit C', state whether any changes therein have occurred during this 6 month reporting period. Yes D No S If yes, have you filed an amendment to the Exhibit C? Yes • No • If no, please attach the required amendment. i The Exhibit C, for which no printed form is provided, consists of a true copy ofthe charter, articles of incorporation, association, and by laws of a registrant that is an organization. (A waiver of the requirement to file an Exhibit C may be obtained for good cause upon written application to the Assistant Attorney General, National Security Division, U.S. -

GCEP EPIC - October 2020 10/6/20, 4�07 PM
GCEP EPIC - October 2020 10/6/20, 407 PM HOME \ CONTACT October 2020 GCEP EPIC The Magazine of the Georgia College of Emergency Physicians IN THIS ISSUE... President's Message Diversity & Inclusion Committee Government Affairs Financial Market News BOD Spotlight Important Dates/GEMLAC President's Message GCEP Members, Life as we know it is beginning to return to some semblance of normalcy. Many emergency departments are beginning to return to pre-pandemic volumes. There has been minimal activity on Governor Kemp's Covid-19 Task Force, but many entities around the state are beginning to return to full capacity. Schools around our John L. Sy, DO, MS, FACEP state have opened or are about to open. It is more President, GCEP important now than ever before to be vigilant. No one is immune, not even the President of the United States (POTUS). We need to focus on physician wellness for our colleagues and ourselves. Please come support GCEP at our annual Lake Oconee meeting - Georgia Emergency Medicine Leadership and Advocacy Conference on December 3-4, 2020. The GCEP Education planning committee and staff have worked very hard to make it possible to attend in the traditional format at the Ritz on Lake Oconee AND new this year we will be offering a virtual option for those who prefer not to travel. Programming will highlight https://ui.constantcontact.com/rnavmap/email/action/print?agentId=1134836320186 Page 1 of 12 GCEP EPIC - October 2020 10/6/20, 407 PM legislators who have been supportive of our advocacy agenda and lectures to improve leadership skills even for those seasoned physicians. -

James.Qxp March Apri
COBB COUNTY A BUSTLING MARCH/APRIL 2017 PAGE 26 AN INSIDE VIEW INTO GEORGIA’S NEWS, POLITICS & CULTURE THE 2017 MOST INFLUENTIAL GEORGIA LOTTERY CORP. CEO ISSUE DEBBIE ALFORD COLUMNS BY KADE CULLEFER KAREN BREMER MAC McGREW CINDY MORLEY GARY REESE DANA RICKMAN LARRY WALKER The hallmark of the GWCCA Campus is CONNEE CTIVITY DEPARTMENTS Publisher’s Message 4 Floating Boats 6 FEATURES James’ 2017 Most Influential 8 JAMES 18 Saluting the James 2016 “Influentials” P.O. BOX 724787 ATLANTA, GEORGIA 31139 24 678 • 460 • 5410 Georgian of the Year, Debbie Alford Building A Proposed Contiguous Exhibition Facilityc Development on the Rise in Cobb County 26 PUBLISHED BY by Cindy Morley INTERNET NEWS AGENCY LLC 2017 Legislators of the Year 29 Building B CHAIRMAN MATTHEW TOWERY COLUMNS CEO & PUBLISHER PHIL KENT Future Conventtion Hotel [email protected] Language Matters: Building C How We Talk About Georgia Schools 21 CHIEF OPERATING OFFICER LOUIE HUNTER by Dr. Dana Rickman ASSOCIATE EDITOR GARY REESE ADVERTISING OPPORTUNITIES Georgia’s Legal Environment on a PATTI PEACH [email protected] Consistent Downward Trend 23 by Kade Cullefer The connections between Georggia World Congress Center venues, the hotel MARKETING DIRECTOR MELANIE DOBBINS district, and the world’world s busiest aairporirport are key differentiaferentiatorsators in Atlanta’Atlanta’s ability to [email protected] Georgia Restaurants Deliver compete for in-demand conventions and tradeshows. CIRCULATION PATRICK HICKEY [email protected] Significant Economic Impact 31 by Karen Bremer CONTRIBUTING WRITERS A fixed gateway between the exhibit halls in Buildings B & C would solidify KADE CULLEFER 33 Atlanta’s place as the world’s premier convention destination. -

1947-1948 Course Catalog
EMORY -at A Division of Emory University Catalog REGISTER 1946-47 Announcements 1947-48 Oxford, Georgia Junior College I hereby apply for admission to the Academy at the opening of the. Quarter, 19 Full Name Permanent Address Address during summer if different Parent or Guardian (Name and Address) Father's occupation (even if not living) Is he living?. Date of applicant's birth Place of birth Church membership If not a member give preference Favorite sport or hobby What will be your probable life work? Outline of Previous Education High School and Other Institution (Name of School) Years Attended 19 19 19 19-- What has been your comparative standing?. (Check one): Low. Average. High Are you enclosing dormitory reservation fee?. Probable length of attendance at Oxford Date: 19 Signature of Applicant EMORY-at- Oxford COLLEGE AND ACADEMY A Division of Emory University 111th YEAR Announcements for Session of 1947-1948 April 1, 1947 POST OFFICE OXFORD, GEQRGIA TABLE OF CONTENTS Page Acadmic Calendar 3 Academy 16-22 Buildings and Equipment 9 College Courses 33-37 Dining Hall 11 Emory's Creed 8 Expenses 29-30 Faculty 5, 10 Health and Medical Care 11 History of Oxford 6 Junior College 7, 23 Location 9 Loan Funds 31 Officers of Administration 4 Officers of Instruction 5 Religious Life 10 Roster 38-44 Scholarship 10-11 Student Activities 12 Student Employment 31 Veterans Education 31 ACADEMIC CALENDAR SUMMER QUARTER 1947 June 10, Tuesday—Summer quarter opens. Saturday classes will be general in the summer quarter. August 22, Friday—Summer quarter closes. FALL QUARTER 1947 September, 23, Tuesday—Fall quarter opens. -

Oxford College
EMORY BOLD LIBERAL ARTS IS PLUS FEARLESS RESEARCH A DIVERSE, INVOLVED COMMUNITY IN ATLANTA, A CITY RICH WITH OPPORTUNITY PREPARING STUDENTS TO CHANGE THE WORLD PAGE 1 l EMORY UNIVERSITY ACADEMICS AT EMORY, undergraduates benefit from an unusual combi- OUR FACULTY—leading scholars, teachers, and experts— nation—the strong teaching and personal connections of a set the tone in our intellectual community, where learning liberal arts college, paired with the resources and expertise extends into after-class conversations and mentoring, and of a top research university. students gain inspiration from their enthusiasm. This combination makes a difference. Students gain access Emory offers an unusual number of academic choices, from to groundbreaking ideas and minds, explore with a vast undergraduate colleges to majors to preprofessional paths, array of tools, and make creative and interdisciplinary giving students many ways to find their right fit. And learning collaborations. across majors is enriched by the city of Atlanta, where students can gain experience and begin to set their sights on the future. INTERNSHIPS 2,000 available in Atlanta and APPLYING KNOWLEDGE 10,000+ Emory students are using what they learn in the class- beyond room to make a difference in the world. Through research, internships, and off-campus study, our students contribute of students do research with to discoveries, tackle difficult issues, and gain a global under- a faculty member across the standing. After graduation, they have experience to build on 55% sciences, -

Erin Phillips Phone: (864) 313-2016 Email: [email protected]
Erin Phillips Phone: (864) 313-2016 Email: [email protected] Education Bachelor of Science in Environmental Sciences Emory University; Atlanta, GA GPA: 3.921 Expected Graduation: June 2022 Relevant Coursework: AP Biology (4), AP Calculus AB/BC (5), AP Chemistry (4) BIO 141L- Foundations of Modern Biology Lab CHEM 202Z- Principles of Reactivity CS 170- Introduction to Computer Science ENVS 120- Living in the Anthropocene ENVS 190- Freshman Seminar in Environmental Sciences ENVS 131- Introduction to ENVS Field Studies ENVS 229- Atmospheric Science with Lab ENVS 240- Ecosystem Ecology ENVS 240L- Ecosystem Ecology Lab ENVS 260- Quantitative Technology in Environmental Study QTM 100- Introduction to Statistical Inference On Campus Involvement 2018-2019: Hamilton Holmes Residence Hall Association 2hrs/wk Secretary Organized meetings and planned events for members of the residence hall 2019-2022: Emory Climate Analysis and Solutions Team 3hrs/wk EmPower Program Developed and taught a program about energy efficiency to a middle school classroom Emory Climate Organization 1hr/wk Events Coordinator Helping plan Universities for Greener Georgia Conference Develops events to communicate climate issues to the general student body Georgia Beta Chapter of Pi Beta Phi 3hrs/wk Member Volunteering and Employment 2016-2019 Roper Mountain Science Center 40hrs/wk Employee Educated the public about the natural sciences, most specifically insects. Handled live animals while educating the public Assisted in “Summer Science” camps that taught elementary and middle -

Gold Dome Report 2017 Session Georgia General Assembly
GOLD DOME REPORT 2017 SESSION GEORGIA GENERAL ASSEMBLY By Nelson Mullins Riley & Scarborough, LLP 404-322-6000 GOLD DOME REPORT 2017 SESSION GEORGIA GENERAL ASSEMBLY TABLE OF CONTENTS Description Page No. Agriculture 3 Alcoholic Beverages 4 Animals 6 Appeal and Error 6 Aviation 7 Banking and Finance 7 Cardiac Care Centers 10 Child Welfare 10 Civil Practice 15 Commerce and Trade 17 Constitution 22 Corporations, Partnerships and Associations 22 Courts 23 Crimes and Offenses 35 Criminal Justice Reform 47 Criminal Procedure 51 Debtor and Creditor 55 Domestic Relations 55 Drugs 60 Education 70 Elections/Ethics 91 Eminent Domain 92 Estates 93 Evidence 94 Fire Protection and Safety 94 Gambling 95 Game and Fish 96 General Assembly 97 Guardian and Ward 98 Handicapped Persons 98 Health 99 Highways, Bridges, and Ferries 115 Hospital Provider Fee 116 Insurance 117 Labor and Industrial Relations 125 Law Enforcement Officers and Agencies 127 Local Government 131 i Description Page No. MARTA 136 Medical Marijuana 137 Mental Health 138 Minors 140 Motor Vehicles and Traffic 141 Narcotic Treatment 144 Natural Resources 146 Penal Institutions 148 Professions/Businesses 153 Property/Liens 163 Public Officers and Employees 168 Public Utilities and Public Transportation 172 Retirement and Pensions 174 Revenue and Taxation 175 Social Services 191 State Government 196 Torts 200 Veterans Affairs 203 Waters of the State, Ports, and Watercraft 207 Budget 208 Study Committees for the Interim 221 ii Gold Dome Report 2017 Legislative Session June, 2017 The 2017 Session of the Georgia General Assembly concluded at 12:50 a.m. on March 31, 2017. Leaders of both chambers decided to work past the historical midnight "deadline" and continued to pass legislation well into the night. -

2015 Georgia Newspaper Directory
2015 Georgia Newspaper Directory An official listing of the members of the Georgia Press Association Published by: Georgia Newspaper Service Inc. January 2015 Affiliate of the Georgia Press Association Table of Contents About Georgia Press Association . 2 GPA Leadership Guide . 3 Newspaper Groups with GPA Members . .4 GPA Member Locator Map . 6 Newspapers by County/Legal Organ . 7 Advertisers: The Brunswick News GPA Daily Newspaper Listings . 9 Cherokee Ledger-News, Woodstock GPA Weekly Newspaper Listings . 22 Georgia EMC GPA Associate Member Listings . .76 Georgia Municipal Association BEHIND EVERY TRAIN ARE GPA Media Associate Member Listings . .78 Georgia Newspaper Service STRONG LOCAL PARTNERSHIPS. Total Market Coverage Publications (TMCs) . 79 Georgia Peanut Commission Georgia College Press Association Member Listings. .80 At Norfolk Southern, we value our community GeorgiaPublicNotice.com connections. Our partnerships are built on a 2014 Statewide Political Officers . 82 Jackson Spalding foundation of safety and service to strengthen 2014 Georgia U.S. Congressmen and General Assembly . 83 MultiAd Georgia’s economy. At Norfolk Southern, we handle everything from combines to cars. But it’s State and Regional Newspaper Associations . 86 Norfolk Southern how we handle them that makes the difference. Smith Communications Inc. * Although every effort is made to ensure the accuracy and thoroughness of Georgia Press Association directory listings, errors and omissions sometimes occur. For corrections or additions, To learn more, contact -
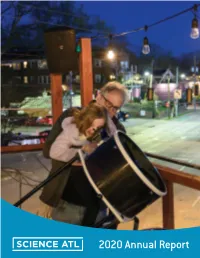
2020 Annual Report Wow - This Has Been Quite a Year
2020 Annual Report Wow - this has been quite a year. Our flagship event, the Atlanta Science Festival, was cancelled days after beginning. In the months that have followed, we’ve been living in a strange new reality - considering what the future holds for an organization like ours that relies so much on interaction with the public. One thing we know for sure, however, is that this time period is only heightening the importance of science for our livelihoods, crystallizing the need for the work we do. We are excited to continue thinking creatively about how to share amazing science with the Atlanta metro region, how to inspire people - young and old - to fall in love with science, and how to make sure that everyone has equitable access to science learning opportunities. While coronavirus and social justice are most present on our minds these days, building this annual report was a much needed opportunity to reflect back on the good work Science ATL has done in the community over the past year before our world turned upside down. We worked with an incredible new cohort of Georgia Chief Science Officers, we nerded out on best practices in science communication with our latest Science ATL Communication Fellows, we held some really spectacular public science events, and strengthened collaborations and CONTENTS friendships with many new and old partners also Letter from Directors.....................p 2 trying to do good in the city. Regardless of what the future holds, we are Overview of Science ATL..............p 3 inspired to continue working with you to cultivate an Atlanta community that is full of Public Engagement......................p 5 love and science. -

Full-Time MBA Catalog 2020-2021
Full-time MBA Catalog 2020-2021 I CERTIFY THIS COPY TO BE TRUE AND CORRECT TO CONTENT AND POLICY _______________________________________ Goizueta Business School Full-time MBA Program One-Year and Two-Year formats Catalog About Goizueta Business School https://goizueta.emory.edu/about OUTLINING SUCCESS,WRITING NEW CHAPTERS Business education has been an integral part of Emory University's identity for more than 100 years. That kind of longevity and significance does not come without a culture built around success and service. Goizueta Advisory Board • Sarah Brown 89MBA, Global Account Director at The Coca-Cola Company (Marietta, GA) • Andrew J. Conway 92MBA, Managing Director at Credit Suisse (Scarsdale, NY) • H. James Dallas 94WEMBA (Atlanta, GA) • Jeffrey C. Denneen 97MBA, Leader, Americas Higher Education Practice at Bain & Company, Inc. (Atlanta, GA) • Robert K. Ehudin 86BBA, Managing Director at Goldman Sachs Group, Inc. (Rye Brook, NY) • Matthew H. Friedman 94BBA, Fidelity Investments (Boston, MA) • Gardiner W. Garrard III 99MBA, Co-Founder, Managing Partner, CEO of TTV Capital (Atlanta, GA) • Rebecca Morris Ginzburg 94BBA, Junto Capital Management, LP (New York, NY) • Michael M. Grindell 99WEMBA, EVP, Chief Administrative Officer, 22squared (Atlanta, GA) • Brian K. Howard, M.D. 15WEMBA, President, North Fulton Plastic Surgery (Atlanta, GA) • Omar A. Johnson 04MBA, Vice President-Marketing, Apple Computer • Mary Humann Judson, President, The Goizueta Foundation (Atlanta, GA) • Michael Marino 94MBA, Managing Director at JP Morgan Chase & Co. (Atlanta, GA) • Jonathan I. Mayblum 84BBA, Co-Founder & CEO of ARCTURUS (Armonk, NY) • Leslie D.J. Patterson 99MBA, EY, Growth Markets Leader (Atlanta, GA) • Olga Goizueta Rawls 77C, Chair & Director of The Goizueta Foundation (Atlanta, GA) • Matthew P. -

GEORGIA BIO 2021 LEGISLATIVE TRACKING SHEET Georgia Bio Will Provide Updates on Specific Legislation of Interest to the Georgia Bio Membership
GEORGIA BIO 2021 LEGISLATIVE TRACKING SHEET Georgia Bio will provide updates on specific legislation of interest to the Georgia Bio membership. If you have bills that you would like included in the weekly bill update, please email [email protected]. BILLS HB 3 - Conservation and natural resources; certain conditions for permits for facilities that emit ethylene oxide; provide Bill Author: Rep. Erick E. Allen (D - Smyrna) Bill Status: No committee assignment yet Summary: HB 3 relates to certain conditions required for permitting of facilities that emit ethylene oxide HB 49; Mental Health Parity Act Bill Author: Rep. Shelly Hutchinson (D - Snellville) Bill Status: House Insurance Committee Summary: HB 49 would require that insurer treatment of mental health and substance use disorder claims be treated in parity with other health insurance claims. HB 72; New Mothers Medicaid Expansion Act Bill Author: Rep. Carolyn Hugley (D - Columbus) Bill Status: House Health & Human Services Committee Summary: HB 49 would require the Department of Community Health to allow mothers giving birth to newborns to retain Medicaid eligibility for one year following birth. HB 73 – Insurance; reduce out-of-pocket costs for consumers requiring insulin Bill Author: Rep. Carolyn Hugley (D - Columbus) Bill Status: House Insurance Committee Summary: HB 73 would implement a $50 out-of-pocket cap on insulin prescriptions for Medicaid and PeachCare recipients. It also outlines annual reporting requirements to the Department of Insurance. HB 80; Supplemental Appropriations Act Bill Author: Rep. David Ralston (R – Blue Ridge) Bill Status: Senate Appropriations Committee Summary: HB 80 is the supplemental appropriations bill to adjust spending for the amended FY2021 budget. -

Georgia Legislative and Regulatory Update
Georgia Legislative and Regulatory Update Peter K. Floyd, Esq. Electric Cities General Counsel Alston & Bird, LLP Electric Cities Annual Meeting Reynolds Plantation, Greensboro, GA March 30, 2011 Georgia Legislative and Regulatory Update . Who I am and Who I’m Not . 2011 Ga. Legislation That Made Crossover Day . 2011 Ga. Legislation That Didn’t Make Crossover Day . Misc. Recent Ga. Legislation . Ga. Territorial Act Update Who I Am and Who I’m Not (www.alston.com) Or, why is this guy up here talking… . Atlanta Headquarters with 850+ attorneys . Attorneys ranked among the best in the U.S. and the world . Strong practices in energy and infrastructure development . Public and private finance . International construction & government contracts practice . Tax Expertise (Intl., Fed., State & Local) . Represent: Ga. state and local governments, public and private owners, engineering and design firms, contractors and subcontractors. Extensive Experience with: public finance, commercial construction, tax, grants and incentives, energy regulation, hospital-medical office building projects, college and university projects, retail and hospitality projects, sporting venues, industrial plants and facilities. Who I Am and Who I’m Not (www.alston.com) Or, why is this guy up here talking… . Help track and interpret legislation and regulation for Electric Cities, MEAG Power and the Gas Authority, among other general counsel/asst. GC duties. Note: I’m not trying to cover everything. There are way too may things relevant cities generally with all of the different hats you where. I’m currently following over 75 different bills in the Ga. General Assembly. I’ll just address electric utility related highlights. I am not a “lobbyist”, so I won’t be much help regarding the latest Gold Dome or PSC dirt.