Nematode Appendix (Supplemental Material That Will NOT Be on Exams)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Animal Parasites and Human Diseases
380 ANIMALS AND DISEASE ANIMAL PARASITES AND HUMAN DISEASES By Paul C. Beaver, Ph.D. Department of Tropical Medicine and Public Health, Tulane University School of Medicine P A1IASITES fall only roughly into the two directed to parasitic infections caused by categories implied in the title of this worms which, regardless of length of resi- discussion. While a few of them arc totally dence in the human body, do not reach full dependent upon htmman hosts, and some are reproductive maturity and are therefore not able to develop only in other animals, a diagnosable by the usual laboratory majority of the parasites commonly re- methods. It is of course the larval stages ferred to as “parasites of man” are in or immature adults that arc involve(! amid!, reality parasites of other animals.1 In the owing to their tendency to be mostly in the latter grouip are such familiar examples as tissues and in many instances difficult to Trichinella, found in rats and many other find and identify, the infections caused by animals, including pigs; Balantidium and them are often unrecognized. Largely for some lesser protozoa of pigs; Toxoplasma, this reason the frequency and severity of which occurs in many wild and domesti- infections of this nature have not been cated animals. Trypanosoma cnuzi, which is fully determined. There are, however, some carried by a variety of animals, is the cause familiar examples. of Chagas’ disease commonly seen in parts Certain well known larval tapeworm in- of South America and found recently in a fections are acquired from other animals. -
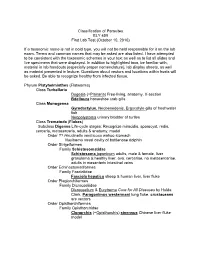
Classification of Parasites BLY 459 First Lab Test (October 10, 2010)
Classification of Parasites BLY 459 First Lab Test (October 10, 2010) If a taxonomic name is not in bold type, you will not be held responsible for it on the lab exam. Terms and common names that may be asked are also listed. I have attempted to be consistent with the taxonomic schemes in your text as well as to list all slides and live specimens that were displayed. In addition to highlighted taxa, be familiar with, material in lab handouts (especially proper nomenclature), lab display sheets, as well as material presented in lecture. Questions about vectors and locations within hosts will be asked. Be able to recognize healthy from infected tissue. Phylum Platyhelminthes (Flatworms) Class Turbellaria Dugesia (=Planaria ) Free-living, anatomy, X-section Bdelloura horseshoe crab gills Class Monogenea Gyrodactylus , Neobenedenis, Ergocotyle gills of freshwater fish Neopolystoma urinary bladder of turtles Class Trematoda ( Flukes ) Subclass Digenea Life-cycle stages: Recognize miracidia, sporocyst, redia, cercaria , metacercaria, adults & anatomy, model Order ?? Hirudinella ventricosa wahoo stomach Nasitrema nasal cavity of bottlenose dolphin Order Strigeiformes Family Schistosomatidae Schistosoma japonicum adults, male & female, liver granuloma & healthy liver, ova, cercariae, no metacercariae, adults in mesenteric intestinal veins Order Echinostomatiformes Family Fasciolidae Fasciola hepatica sheep & human liver, liver fluke Order Plagiorchiformes Family Dicrocoeliidae Dicrocoelium & Eurytrema Cure for All Diseases by Hulda Clark, Paragonimus -

Prevalence of Intestinal Helminth Infections in Dogs and Two Species of Wild Animals from Samarkand Region of Uzbekistan
ISSN (Print) 0023-4001 ISSN (Online) 1738-0006 Korean J Parasitol Vol. 57, No. 5: 549-552, October 2019 ▣ BRIEF COMMUNICATION https://doi.org/10.3347/kjp.2019.57.5.549 Prevalence of Intestinal Helminth Infections in Dogs and Two Species of Wild Animals from Samarkand Region of Uzbekistan Tai-Soon Yong1, Kyu-Jae Lee2, Myeong Heon Shin1, Hak Sun Yu3, Uktamjon Suvonkulov4, 4 5 6, Turycin Bladimir Sergeevich , Azamat Shamsiev , Gab-Man Park * 1Department of Environmental Medical Biology and Institute of Tropical Medicine, Yonsei University College of Medicine, Seoul 03722, Korea; 2Department of Environmental Medical Biology, Yonsei University Wonju College of Medicine, Wonju 26426, Korea; 3Department of Parasitology and Tropical Medicine, School of Medicine, Pusan National University, Yangsan 50612, Korea; 4Isaev Research Institute of Medical Parasitology, Ministry of Health, Samarkand, Republic of Uzbekistan; 5Department of Pediatric Surgery, Samarkand Medical Institute, Samarkand, Republic of Uzbekistan; 6Department of Environmental Medical Biology, Catholic Kwandong University College of Medicine, Gangneung 25601, Korea Abstract: This study aimed to determine the prevalence of intestinal helminth parasitic infections and associated risk fac- tors for the human infection among the people of Samarkand, Uzbekistan. Infection status of helminths including Echino- coccus granulosus was surveyed in domestic and wild animals from 4 sites in the Samarkand region, Uzbekistan during 2015-2018. Fecal samples of each animal were examined with the formalin-ether sedimentation technique and the recov- ery of intestinal helminths was performed with naked eyes and a stereomicroscope in total 1,761 animals (1,755 dogs, 1 golden jackal, and 5 Corsac foxes). Total 658 adult worms of E. -

Agent for Expelling Parasites in Humans, Animals Or Birds
(19) TZZ Z_T (11) EP 2 496 089 B1 (12) EUROPEAN PATENT SPECIFICATION (45) Date of publication and mention (51) Int Cl.: of the grant of the patent: A01N 65/00 (2009.01) A01N 65/10 (2009.01) 22.02.2017 Bulletin 2017/08 A61K 36/23 (2006.01) A01P 5/00 (2006.01) (21) Application number: 10803029.7 (86) International application number: PCT/BE2010/000077 (22) Date of filing: 05.11.2010 (87) International publication number: WO 2011/054066 (12.05.2011 Gazette 2011/19) (54) AGENT FOR EXPELLING PARASITES IN HUMANS, ANIMALS OR BIRDS MITTEL ZUR ABWEISUNG VON PARASITEN BEI MENSCHEN, TIEREN ODER VÖGELN AGENT POUR EXPULSER DES PARASITES CHEZ DES HUMAINS, DES ANIMAUX OU DES OISEAUX (84) Designated Contracting States: (56) References cited: AL AT BE BG CH CY CZ DE DK EE ES FI FR GB • RAMADAN NASHWA I ET AL: "The in vitro effect GR HR HU IE IS IT LI LT LU LV MC MK MT NL NO of assafoetida on Trichomonas vaginalis", PL PT RO RS SE SI SK SM TR JOURNAL OF THE EGYPTIAN SOCIETY OF PARASITOLOGY, EGYPTIAN SOCIETY OF (30) Priority: 06.11.2009 BE 200900689 PARAS1TOLOGY, CAIRO, EG, vol. 33, no. 2, 1 August 2003 (2003-08-01) , pages 615-630, (43) Date of publication of application: XP009136264, ISSN: 1110-0583 12.09.2012 Bulletin 2012/37 • DATABASE MEDLINE [Online] US NATIONAL LIBRARY OF MEDICINE (NLM), BETHESDA, MD, (73) Proprietors: US; December 2004 (2004-12), RAMADAN • MEIJS, Maria Wilhelmina NASHWA I ET AL: "Effect of Ferula assafoetida 4852 Hombourg (BE) on experimental murine Schistosoma mansoni • VAESSEN, Jan Jozef infection.", XP002592455, Database accession 4852 Hombourg (BE) no. -

Efficacy of Simparica Trio™, a Novel Chewable Tablet Containing
Becskei et al. Parasites Vectors (2020) 13:99 https://doi.org/10.1186/s13071-020-3951-4 Parasites & Vectors RESEARCH Open Access Efcacy of Simparica Trio™, a novel chewable tablet containing sarolaner, moxidectin and pyrantel, against induced hookworm infections in dogs Csilla Becskei1*, Mirjan Thys1, Kristina Kryda2, Leon Meyer3,4, Susanna Martorell5, Thomas Geurden1, Leentje Dreesen1, Tiago Fernandes1 and Sean P. Mahabir2 Abstract Background: Ancylostomatids (‘hookworms’) are among the most important zoonotic nematode parasites infecting dogs worldwide. Ancylostoma caninum and Uncinaria stenocephala are two of the most common hookworm species that infect dogs. Both immature and adult stages of hookworms are voracious blood feeders and can cause death in young dogs before infection can be detected by routine fecal examination. Hence, treatment of both immature and adult stages of hookworms will decrease the risk of important clinical disease in the dog as well as the environmental contamination caused by egg-laying adults, which should reduce the risk of infection for both dogs and humans. The studies presented here were conducted to evaluate the efcacy of a novel, oral chewable tablet containing sarolaner, ™ moxidectin and pyrantel (Simparica Trio ), against induced larval (L4), immature adult (L5) and adult A. caninum, and adult U. stenocephala infections in dogs. Methods: Eight negative-controlled, masked, randomized laboratory studies were conducted. Two separate studies were conducted against each of the target parasites and stages. Sixteen or 18 purpose bred dogs, 8 or 9 in each of the two treatment groups, were included in each study. Dogs experimentally infected with the target parasite were dosed once on Day 0 with either placebo tablets or Simparica Trio™ tablets to provide minimum dosages of 1.2 mg/kg sarolaner, 24 µg/kg moxidectin and 5.0 mg/kg pyrantel (as pamoate salt). -

Worms, Nematoda
University of Nebraska - Lincoln DigitalCommons@University of Nebraska - Lincoln Faculty Publications from the Harold W. Manter Laboratory of Parasitology Parasitology, Harold W. Manter Laboratory of 2001 Worms, Nematoda Scott Lyell Gardner University of Nebraska - Lincoln, [email protected] Follow this and additional works at: https://digitalcommons.unl.edu/parasitologyfacpubs Part of the Parasitology Commons Gardner, Scott Lyell, "Worms, Nematoda" (2001). Faculty Publications from the Harold W. Manter Laboratory of Parasitology. 78. https://digitalcommons.unl.edu/parasitologyfacpubs/78 This Article is brought to you for free and open access by the Parasitology, Harold W. Manter Laboratory of at DigitalCommons@University of Nebraska - Lincoln. It has been accepted for inclusion in Faculty Publications from the Harold W. Manter Laboratory of Parasitology by an authorized administrator of DigitalCommons@University of Nebraska - Lincoln. Published in Encyclopedia of Biodiversity, Volume 5 (2001): 843-862. Copyright 2001, Academic Press. Used by permission. Worms, Nematoda Scott L. Gardner University of Nebraska, Lincoln I. What Is a Nematode? Diversity in Morphology pods (see epidermis), and various other inverte- II. The Ubiquitous Nature of Nematodes brates. III. Diversity of Habitats and Distribution stichosome A longitudinal series of cells (sticho- IV. How Do Nematodes Affect the Biosphere? cytes) that form the anterior esophageal glands Tri- V. How Many Species of Nemata? churis. VI. Molecular Diversity in the Nemata VII. Relationships to Other Animal Groups stoma The buccal cavity, just posterior to the oval VIII. Future Knowledge of Nematodes opening or mouth; usually includes the anterior end of the esophagus (pharynx). GLOSSARY pseudocoelom A body cavity not lined with a me- anhydrobiosis A state of dormancy in various in- sodermal epithelium. -

ISSN: 2320-5407 Int. J. Adv. Res. 5(3), 972-999 REVIEW ARTICLE ……………………………………………………
ISSN: 2320-5407 Int. J. Adv. Res. 5(3), 972-999 Journal Homepage: - www.journalijar.com Article DOI: 10.21474/IJAR01/3597 DOI URL: http://dx.doi.org/10.21474/IJAR01/3597 REVIEW ARTICLE HAEMONCHUS CONTORTUS AND OVINE HOST: A RETROSPECTIVE REVIEW. *Saeed El-Ashram1,2, Ibrahim Al Nasr3,4, Rashid mehmood5,6, Min Hu7, Li He7, *Xun Suo1 1. National Animal Protozoa Laboratory, College of Veterinary Medicine, China Agricultural University, Beijing 100193, China. 2. Faculty of Science, Kafr El-Sheikh University, Kafr El-Sheikh, Egypt. 3. College of Science and Arts in Unaizah, Qassim University, Unaizah, Saudi Arabia. 4. College of Applied Health Sciences in Ar Rass, Qassim University, Ar Rass 51921, Saudi Arabia. 5. College of information science and technology, Beijing normal university, Beijing, china. 6. Department of Computer Science and Information Technology, University of Management Sciences and Information Technology, Kotli Azad Kashmir, 11100, Pakistan 7. State Key Laboratory of Agricultural Microbiology, Key Laboratory of Development of Veterinary Products, Ministry of Agriculture, College of Veterinary Medicine, Huazhong Agricultural University, Wuhan 430070, Hubei,China. …………………………………………………………………………………………………….... Manuscript Info Abstract ……………………. ……………………………………………………………… Manuscript History Gastrointestinal (GI) parasitic infections are a world-wide problem for Received: 05 January 2017 both small- and large-scale farmers. Infection by GI parasites in Final Accepted: 09 February 2017 ruminants, including sheep and goat can result in harsh economic losses Published: March 2017 in a variety of ways: reproductive inefficiency, decreased work capacity, involuntary culling, diminished food intake, poor animal growth rates and lower weight gains, treatment and management costs, Key words:- Gastrointestinal (GI) parasitic infections; and mortality in heavily parasitized animals. -

Monophyly of Clade III Nematodes Is Not Supported by Phylogenetic Analysis of Complete Mitochondrial Genome Sequences
UC Davis UC Davis Previously Published Works Title Monophyly of clade III nematodes is not supported by phylogenetic analysis of complete mitochondrial genome sequences Permalink https://escholarship.org/uc/item/7509r5vp Journal BMC Genomics, 12(1) ISSN 1471-2164 Authors Park, Joong-Ki Sultana, Tahera Lee, Sang-Hwa et al. Publication Date 2011-08-03 DOI http://dx.doi.org/10.1186/1471-2164-12-392 Peer reviewed eScholarship.org Powered by the California Digital Library University of California Park et al. BMC Genomics 2011, 12:392 http://www.biomedcentral.com/1471-2164/12/392 RESEARCHARTICLE Open Access Monophyly of clade III nematodes is not supported by phylogenetic analysis of complete mitochondrial genome sequences Joong-Ki Park1*, Tahera Sultana2, Sang-Hwa Lee3, Seokha Kang4, Hyong Kyu Kim5, Gi-Sik Min2, Keeseon S Eom6 and Steven A Nadler7 Abstract Background: The orders Ascaridida, Oxyurida, and Spirurida represent major components of zooparasitic nematode diversity, including many species of veterinary and medical importance. Phylum-wide nematode phylogenetic hypotheses have mainly been based on nuclear rDNA sequences, but more recently complete mitochondrial (mtDNA) gene sequences have provided another source of molecular information to evaluate relationships. Although there is much agreement between nuclear rDNA and mtDNA phylogenies, relationships among certain major clades are different. In this study we report that mtDNA sequences do not support the monophyly of Ascaridida, Oxyurida and Spirurida (clade III) in contrast to results for nuclear rDNA. Results from mtDNA genomes show promise as an additional independently evolving genome for developing phylogenetic hypotheses for nematodes, although substantially increased taxon sampling is needed for enhanced comparative value with nuclear rDNA. -

A Parasite of Red Grouse (Lagopus Lagopus Scoticus)
THE ECOLOGY AND PATHOLOGY OF TRICHOSTRONGYLUS TENUIS (NEMATODA), A PARASITE OF RED GROUSE (LAGOPUS LAGOPUS SCOTICUS) A thesis submitted to the University of Leeds in fulfilment for the requirements for the degree of Doctor of Philosophy By HAROLD WATSON (B.Sc. University of Newcastle-upon-Tyne) Department of Pure and Applied Biology, The University of Leeds FEBRUARY 198* The red grouse, Lagopus lagopus scoticus I ABSTRACT Trichostrongylus tenuis is a nematode that lives in the caeca of wild red grouse. It causes disease in red grouse and can cause fluctuations in grouse pop ulations. The aim of the work described in this thesis was to study aspects of the ecology of the infective-stage larvae of T.tenuis, and also certain aspects of the pathology and immunology of red grouse and chickens infected with this nematode. The survival of the infective-stage larvae of T.tenuis was found to decrease as temperature increased, at temperatures between 0-30 C? and larvae were susceptible to freezing and desiccation. The lipid reserves of the infective-stage larvae declined as temperature increased and this decline was correlated to a decline in infectivity in the domestic chicken. The occurrence of infective-stage larvae on heather tips at caecal dropping sites was monitored on a moor; most larvae were found during the summer months but very few larvae were recovered in the winter. The number of larvae recovered from the heather showed a good correlation with the actual worm burdens recorded in young grouse when related to food intake. Examination of the heather leaflets by scanning electron microscopy showed that each leaflet consists of a leaf roll and the infective-stage larvae of T.tenuis migrate into the humid microenvironment' provided by these leaf rolls. -

Helminthology Nematodes Strongyloides.Pdf
HelminthologyHelminthology –– NematodesNematodes StrongyloidesStrongyloides TerryTerry LL DwelleDwelle MDMD MPHTMMPHTM ClassificationClassification ofof NematodesNematodes Subclass Order Superfamily Genus and Species Probable (suborder) prevalence in man Secernentea Rhabditida Rhabditoidea Strongyloides stercoralis 56 million Stronglyloides myoptami Occasional Strongyloides fuelloborni Millions Strongyloides pyocyanis Occasional GeneralGeneral InformationInformation ► PrimarilyPrimarily aa diseasedisease ofof tropicaltropical andand subtropicalsubtropical areas,areas, highlyhighly prevalentprevalent inin Brazil,Brazil, Columbia,Columbia, andand SESE AsiaAsia ► ItIt isis notnot uncommonuncommon inin institutionalinstitutional settingssettings inin temperatetemperate climatesclimates ((egeg mentalmental hospitals,hospitals, prisons,prisons, childrenchildren’’ss homes)homes) ► SeriousSerious problemproblem inin thosethose onon immunosuppressiveimmunosuppressive therapytherapy ► HigherHigher prevalenceprevalence inin areasareas withwith aa highhigh waterwater tabletable GeneralGeneral RecognitionRecognition FeaturesFeatures ► Size;Size; parasiticparasitic femalefemale 2.72.7 mm,mm, freefree livingliving femalefemale 1.21.2 mm,mm, freefree livingliving malemale 0.90.9 mmmm ► EggsEggs –– 5050--5858 XX 3030--3434 umum ► TheThe RhabdiformRhabdiform larvaelarvae havehave aa shortershorter buccalbuccal canalcanal vsvs hookwormhookworm ► LarvaeLarvae havehave aa doubledouble laterallateral alaealae,, smallersmaller thanthan hookwormhookworm ► S.S. -

Ostertagia Ostertagi Excretory-Secretory Products
Academic Year 2007-2008 Laboratory for Parasitology Department of Virology, Parasitology and Immunology Ghent University – Faculty of Veterinary Medicine Study of Ostertagia ostertagi excretory-secretory products Heidi Saverwyns Proefschrift voorgelegd aan de faculteit Diergeneeskunde tot het behalen van de graad van Doctor in de Diergeneeskundige Wetenschappen Promotoren: Prof. Dr. E. Claerebout en Dr. P. Geldhof Het heeft wel eventjes geduurd, maar nu is het zover. Veel mensen hebben de afgelopen jaren direct of indirect hun medewerking verleend aan het tot stand komen van dit proefschrift. Een aantal van hen wil ik hier persoonlijk bedanken. In eerste instantie wens ik Prof dr. Jozef Vercuysse en mijn promotor Prof. Dr. Edwin Claerebout te bedanken omdat jullie mij de kans boden om op het labo Parasitologie te doctoreren. Jullie deur stond altijd open zowel in goede tijden als in slechte tijden. Bedankt voor alles!! Peter, nog maar pas terug uit Moredun en vervolgens gebombardeerd tot mijn promotor. Jouw hulp was onmisbaar bij het vervolledigen van dit proefschrift. Hopelijk heb je niet te veel fietsuren moeten missen door de ontelbare corrigeersessies. Denk vooral aan die ‘oh zo leuke bureau momenten’ wanneer we samen neurieden op mijn nieuwste ringtone. Dr. Marc Fransen, bedankt voor alle hulp en goede tips wanneer mijn fagen niet deden wat van hen verwacht werd. Natuurlijk wil ik u ook bedanken voor het gedetailleerd en supersnel nalezen van dit proefschrift! Isabel, jouw hersenspinsels (neergepend in een FWO aanvraag) betekenden het startsignaal van een wilde rit op het faagdisplay rad. Je hebt ons reeds enkele jaren geleden verlaten, desalniettemin was je direct bereid om in mijn leescommissie te zetelen. -

(<I>Alces Alces</I>) of North America
University of Tennessee, Knoxville TRACE: Tennessee Research and Creative Exchange Doctoral Dissertations Graduate School 12-2015 Epidemiology of select species of filarial nematodes in free- ranging moose (Alces alces) of North America Caroline Mae Grunenwald University of Tennessee - Knoxville, [email protected] Follow this and additional works at: https://trace.tennessee.edu/utk_graddiss Part of the Animal Diseases Commons, Other Microbiology Commons, and the Veterinary Microbiology and Immunobiology Commons Recommended Citation Grunenwald, Caroline Mae, "Epidemiology of select species of filarial nematodes in free-ranging moose (Alces alces) of North America. " PhD diss., University of Tennessee, 2015. https://trace.tennessee.edu/utk_graddiss/3582 This Dissertation is brought to you for free and open access by the Graduate School at TRACE: Tennessee Research and Creative Exchange. It has been accepted for inclusion in Doctoral Dissertations by an authorized administrator of TRACE: Tennessee Research and Creative Exchange. For more information, please contact [email protected]. To the Graduate Council: I am submitting herewith a dissertation written by Caroline Mae Grunenwald entitled "Epidemiology of select species of filarial nematodes in free-ranging moose (Alces alces) of North America." I have examined the final electronic copy of this dissertation for form and content and recommend that it be accepted in partial fulfillment of the equirr ements for the degree of Doctor of Philosophy, with a major in Microbiology. Chunlei Su,