Colon-Targeted Delivery Systems for Therapeutic Applications: Drug Release from Multiparticulate, Monolithic Matrix, and Capsule-Filled Delivery Systems
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Softgels' Clear Advantages
DEEPDIVE REPORT March 2019 naturalproductsinsider.com Softgels’ Clear Advantages Report brought to you by DEEPDIVE REPORT Softgels’ Clear Advantages Contents Market snapshot ..................................................................................... 3 Consumer appeal .................................................................................... 4 Softgel history .......................................................................................... 6 Advantages of softgels ........................................................................... 7 How softgels are made .......................................................................... 9 Softgel challenges and solutions .......................................................11 Oxidation ...........................................................................................11 Consumer experience .......................................................................12 Dietary considerations ......................................................................12 Shelf stability ....................................................................................14 Bioavailability ....................................................................................14 Innovative developments .....................................................................16 Copyright © 2019 Informa Exhibitions LLC. All rights reserved. The publisher reserves the right to accept or reject any advertising or editorial material. Advertisers, and/or their agents, assume the -

Prescription Advantage Drug Exclusions
February 23, 2006 Dear Prescription Advantage Member: This letter is to inform you about changes to your Prescription Advantage coverage because of the new Medicare prescription drug coverage that began on January 1, 2006. Since this drug coverage will be available, Prescription Advantage will provide supplemental coverage for prescription drug purchases of members who are eligible for Medicare. For all members, with or without Medicare, Prescription Advantage will only cover classes of drugs that Medicare has not excluded from coverage. We have determined that you have taken one or more of the prescription drugs listed on the second page of this letter, which Medicare has excluded from coverage. As of March 31, 2006, Prescription Advantage will no longer cover these drugs. We recommend that you speak to your doctor regarding this change in drug coverage as he or she can most appropriately advise you of any viable alternatives or substitutions that are available to you. Your doctor is the most qualified person to determine which prescription drugs are suitable for you. If you have any questions, please call Customer Service (toll free) at 1-800-AGE-INFO (1-800- 243-4636) or TTY for the deaf and hard of hearing at 1-877-610-0241. Sincerely, Prescription Advantage Commonwealth of Massachusetts Executive Office of Health and Human Services Executive Office of Elder Affairs Prescription Advantage 1-800-AGE-INFO (1-800-243-4636) TTY: 1-877-610-0241 www.800ageinfo.com 3/9/2006 Page 2 of 3 Alkabel-sr tablet Fioricet tablet Phenazopyridine plus -

Journal of Controlled Release 161 (2012) 446–460
Journal of Controlled Release 161 (2012) 446–460 Contents lists available at SciVerse ScienceDirect Journal of Controlled Release journal homepage: www.elsevier.com/locate/jconrel Review Administration, distribution, metabolism and elimination of polymer therapeutics Ela Markovsky, Hemda Baabur-Cohen, Anat Eldar-Boock, Liora Omer, Galia Tiram, Shiran Ferber, Paula Ofek, Dina Polyak, Anna Scomparin, Ronit Satchi-Fainaro ⁎ Department of Physiology and Pharmacology, Sackler School of Medicine, Tel Aviv University, Tel Aviv 69978, Israel article info abstract Article history: Polymer conjugation is an efficient approach to improve the delivery of drugs and biological agents, both by Received 6 September 2011 protecting the body from the drug (by improving biodistribution and reducing toxicity) and by protecting the Accepted 16 December 2011 drug from the body (by preventing degradation and enhancing cellular uptake). This review discusses the Available online 29 December 2011 journey that polymer therapeutics make through the body, following the ADME (absorption, distribution, metabolism, excretion) concept. The biological factors and delivery system parameters that influence each Keywords: stage of the process will be described, with examples illustrating the different solutions to the challenges Polymer therapeutics Angiogenesis of drug delivery systems in vivo. ADME © 2011 Elsevier B.V. All rights reserved. Biodistribution Angiogenesis-dependent diseases Cancer Contents 1. Introduction ............................................................. -
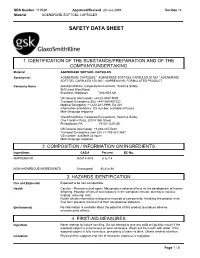
Safety Data Sheet
SDS Number 110529 Approved/Revised 23-Jun-2008 Version 14 Material AGENERASE SOFTGEL CAPSULES SAFETY DATA SHEET 1. IDENTIFICATION OF THE SUBSTANCE/PREPARATION AND OF THE COMPANY/UNDERTAKING space Material AGENERASE SOFTGEL CAPSULES space Synonym(s) AGENERASE CAPSULES * AGENERASE SOFTGEL CAPSULES 50 MG * AGENERASE SOFTGEL CAPSULES 150 MG * AMPRENAVIR, FORMULATED PRODUCT space Company Name GlaxoSmithKline, Corporate Environment, Health & Safety 980 Great West Road Brentford, Middlesex TW8 9GS UK space UK General Information: +44-20-8047-5000 Transport Emergency (EU) +44-1865-407333 Medical Emergency +1-612-221-3999, Ext 221 Information and Advice: US number, available 24 hours Multi-language response space GlaxoSmithKline, Corporate Environment, Health & Safety One Franklin Plaza, 200 N 16th Street Philadelphia, PA 19102-1225 US space US General Information: +1-888-825-5249 Transport Emergency (non EU) +1-703-527-3887 US number, available 24 hours Multi-language response . 2. COMPOSITION / INFORMATION ON INGREDIENTS space Ingredients CAS # Percent EC-No. AMPRENAVIR 161814-49-9 6 to 7.4 NON-HAZARDOUS INGREDIENTS Unassigned 92.6 to 94 3. HAZARDS IDENTIFICATION space Fire and Explosion Expected to be non-combustible. space Health Caution - Pharmaceutical agent. May produce adverse effects on the development of human offspring. Possible effects of overexposure in the workplace include: diarrhoea; nausea; tingling; vomiting; rash. Health effects information is based on hazards of components. Handling this product in its final form presents minimal risk from occupational exposure. space Environment No information is available about the potential of this product to produce adverse environmental effects. 4. FIRST-AID MEASURES space Ingestion Never attempt to induce vomiting. -

From Molecule to Dose Form Bioavailability Toolkit to Fast Track Development Introduction
contents introduction 2 part one: Connecting the 4 Dots in Drug Delivery part two: The Bioavailability 8 Toolbox part three: The Toolbox of 2025 16 part four: Delivering Change 21 from molecule to dose form bioavailability toolkit to fast track development introduction When it comes to drug formulation challenges, there trend and the key to succeed in this competitive is no one-size-fits-all solution. landscape. The leading evidence of this trend includes more direct-to-consumer advertising and a The 3rd annual drug delivery landscape survey* recent patient focused drug development initiative confirms that bioavailability, safety, efficacy by the FDA to gather the patient’s perspective and solubility are the top challenges faced by on their condition and available treatments. formulation scientists. The pharmaceutical and Interestingly, survey data shows that although biopharmaceutical industries have to overcome not the industry has identified the value of patient- only formulation challenges but also the business centric drug design, it has not been very successful challenges of bringing a product successfully to in applying it. For instance, to successfully apply market. The survey participants, a vast majority of patient-centric design, the drug product should be whom are Formulation Scientists and R&D Managers, adapted as per the patient’s preference at earlier indicated that development time, selecting the stages of drug development to avoid high costs at appropriate drug delivery platform, budget and late stages, a practice which is not very common in choosing the right external partner are the top the industry. Also, when asked to rate the significant business challenges. -

Brain-Targeted Drug Delivery by Manipulating Protein Corona Functions
ARTICLE https://doi.org/10.1038/s41467-019-11593-z OPEN Brain-targeted drug delivery by manipulating protein corona functions Zui Zhang1,2, Juan Guan1, Zhuxuan Jiang1, Yang Yang1, Jican Liu3, Wei Hua4, Ying Mao4, Cheng Li2, Weiyue Lu2, Jun Qian2 & Changyou Zhan 1,2 Protein corona presents a major obstacle to bench-to-bedside translation of targeted drug delivery systems, severely affecting targeting yields and directing unfavorable biodistribution. 1234567890():,; Corona-mediated targeting provides a new impetus for specific drug delivery by precisely manipulating interaction modes of functional plasma proteins on nano-surface. Here bio- inspired liposomes (SP-sLip) were developed by modifying liposomal surface with a short nontoxic peptide derived from Aβ1-42 that specifically interacts with the lipid-binding domain of exchangeable apolipoproteins. SP-sLip absorb plasma apolipoproteins A1, E and J, con- sequently exposing receptor-binding domain of apolipoproteins to achieve brain-targeted delivery. Doxorubicin loaded SP-sLip (SP-sLip/DOX) show significant enhancement of brain distribution and anti-brain cancer effect in comparison to doxorubicin loaded plain liposomes. SP-sLip preserve functions of the absorbed human plasma ApoE, and the corona-mediated targeting strategy works in SP modified PLGA nanoparticles. The present study may pave a new avenue to facilitate clinical translation of targeted drug delivery systems. 1 Department of Pharmacology, School of Basic Medical Sciences & State Key Laboratory of Molecular Engineering of Polymers, Fudan University, 200032 Shanghai, PR China. 2 School of Pharmacy & Key Laboratory of Smart Drug Delivery (Fudan University), Ministry of Education, 201203 Shanghai, PR China. 3 Department of Pathology, Affiliated Zhongshan Hospital Qingpu Branch, Fudan University, 201700 Shanghai, PR China. -

Novel Thyroxine Formulations: a Further Step Toward Precision Medicine
Endocrine (2019) 66:87–94 https://doi.org/10.1007/s12020-019-02049-x REVIEW Novel thyroxine formulations: a further step toward precision medicine 1 2 1,3 Camilla Virili ● Pierpaolo Trimboli ● Marco Centanni Received: 3 June 2019 / Accepted: 5 August 2019 © Springer Science+Business Media, LLC, part of Springer Nature 2019 Abstract Levothyroxine (T4) is a critical-dose drug, because little variations in the blood concentration may cause treatment failure as well as iatrogenic thyrotoxicosis. Despite the dose response of this drug being more carefully titrated nowadays, several papers still report that a significant fraction of patients treated with levothyroxine demonstrate a TSH which is not on target. Moreover, some widespread gastrointestinal disorders as well as interfering drugs and foods may cause the “refractoriness” of a significant number of patients to an expected dose of thyroxine. The increasing awareness of the mechanisms interfering with the oral thyroid hormone bioavailability and the body of evidence regarding the complexity of treatment in certain classes of patients prompted pharmaceutical research to identify new hormonal formulations to optimize the performance of fi 1234567890();,: 1234567890();,: this drug. In this brief review, the progression of the scienti c knowledge of novel T4 formulations use has been analyzed. Keywords Liquid levothyroxine ● Softgel thyroxine ● Thyroxine absorption ● Thyroxine malabsorption ● Drugs dissolution ● Gastrointestinal disorders Introduction levothyroxine doses are used to treat patients of different ages and with specific clinical conditions [8]. Synthesized in 1927 by Harrington [1] and obtained as The daily requirement of levothyroxine depends on sodium salt in 1950 [2], levothyroxine (T4) has subse- patients’ lean body mass [9], the leading cause of hypo- quently obtained the role of gold standard in the treatment thyroidism and the therapeutic goal [e.g. -

Pharmacokinetics and Pharmacodynamics Modeling and Simulation Systems to Support the Development and Regulation of Liposomal Drugs
pharmaceutics Review Pharmacokinetics and Pharmacodynamics Modeling and Simulation Systems to Support the Development and Regulation of Liposomal Drugs Hua He 1,2, Dongfen Yuan 2 , Yun Wu 3 and Yanguang Cao 2,4,* 1 Center of Drug Metabolism and Pharmacokinetics, China Pharmaceutical University, Nanjing 210009, China; [email protected] 2 Division of Pharmacotherapy and Experimental Therapeutics, School of Pharmacy, University of North Carolina at Chapel Hill, Chapel Hill, NC 27599, USA; [email protected] 3 Department of Biomedical Engineering, University at Buffalo, The State University of New York, 332 Bonner Hall, Buffalo, NY 14260, USA; [email protected] 4 Lineberger Comprehensive Cancer Center, University of North Carolina at Chapel Hill, Chapel Hill, NC 27599, USA * Correspondence: [email protected]; Tel.: +1-(919)-966-4040 Received: 30 January 2019; Accepted: 28 February 2019; Published: 7 March 2019 Abstract: Liposomal formulations have been developed to improve the therapeutic index of encapsulated drugs by altering the balance of on- and off-targeted distribution. The improved therapeutic efficacy of liposomal drugs is primarily attributed to enhanced distribution at the sites of action. The targeted distribution of liposomal drugs depends not only on the physicochemical properties of the liposomes, but also on multiple components of the biological system. Pharmacokinetic–pharmacodynamic (PK–PD) modeling has recently emerged as a useful tool with which to assess the impact of formulation- and system-specific factors on the targeted disposition and therapeutic efficacy of liposomal drugs. The use of PK–PD modeling to facilitate the development and regulatory reviews of generic versions of liposomal drugs recently drew the attention of the U.S. -

Important Pharmacy Information There Is No Copay When Your Primary Care Provider (PCP) Or Unitedhealthcare Community Plan Specialist Writes You a Covered Prescription
Important Pharmacy Information There is no copay when your Primary Care Provider (PCP) or UnitedHealthcare Community Plan Specialist writes you a covered prescription. But you can get many over-the-counter (OTC) medicines free when you have a prescription. You can get the medications listed on the following pages when they are medically necessary and you get a written prescription from your UnitedHealthcare Community Plan doctor and take it to a UnitedHealthcare Community Plan pharmacy. To get your medicine: • Take your prescription to a UnitedHealthcare Community Plan pharmacy. To find a pharmacy, call 1-800-903-5253 or go to UHCCommunityPlan.com. • For your safety, we urge you to select a single pharmacy from which to get your drugs. • Get to know the pharmacist and build a relationship. If the UnitedHealthcare Community Plan pharmacy says they cannot fill your covered prescription or you have to pay more than your copay: Do not leave the pharmacy. Do not pay for it yourself. Ask the pharmacy why they cannot fill your prescription. Response Your Solution Not Covered • Ask them to call OptumRx right away to find out which medicine is covered. • Ask them to call your doctor to see if you can get the covered medicine instead. Prior • Ask them to call your doctor for a prior authorization. Authorization • You can call your doctor and ask that a prior authorization be sent to: Needed UnitedHealthcare Pharmacy Prior Notification Service Fax 1-866-940-7328 Phone 1-800-310-6826 Refill Too Soon • Ask what day it can be filled. • Pick your prescription up the day it can be filled. -

SOFT GELATIN CAPSULES Capsules Are Solid Oral Dosage Forms in Which the Drug Is Enclosed Within a Hard Or Soft Shell
CAPSULES PRODUCTION. MICROCAPSULES. HARD AND SOFT GELATIN CAPSULES Capsules are solid oral dosage forms in which the drug is enclosed within a hard or soft shell. The shell is normally made from gelatin and results in a simple, easy - to - swallow formulation with no requirement for a further coating step. They can be either hard or soft depending on the nature of the capsule shell, with soft capsules possessing a fl exible, plasticized gelatin fi lm. Hard gelatin capsules are usually rigid two - piece capsules that are manufactured in one procedure and packed in another totally separate operation, whereas the formulation of soft gelatin capsules is more complex but all steps are integrated. There is a growing interest in using non - animal - derived products for formulation of the capsule shells to address cultural, religious, and dietary requirements. HPMC (e.g., V - caps, Quali - VC, Vegicaps) and pullulan shells (NPCaps) and starch are alternatives. Hard - Shell Gelatin Capsules Although the challenges of powder blending, homogeneity, and lubcricity exist for capsules as for tablets, they are generally perceived to be a more fl exible formulation as there is no requirement for the powders to form a robust compact. This means that they may also be more suitable for delivery of granular and beadlike formulations, fragile formulations that could be crushed by the normal compaction step. They are commonly employed in clinical trials due to the relative ease of blinding and are useful for taste masking. Capsules are usually more expensive dosage forms than an equivalent tablet formulation due to the increased cost of the shells and the slower production rates. -

Challenges of Dissolution Methods Development for Soft Gelatin Capsules
pharmaceutics Review Challenges of Dissolution Methods Development for Soft Gelatin Capsules Festo Damian 1, Mohammad Harati 2, Jeff Schwartzenhauer 3, Owen Van Cauwenberghe 1,4 and Shawn D. Wettig 1,5,* 1 School of Pharmacy, University of Waterloo, 200 University Ave W, Waterloo, ON N2L 3G1, Canada; [email protected] (F.D.); [email protected] (O.V.C.) 2 Department of Natural Sciences, University of Michigan, 2209 Natural Sciences Building, 4901 Evergreen Rd, Dearborn, MI 48128, USA; [email protected] 3 Catalent Pharma Solutions, 2125 Ambassador Dr, Windsor, ON N9C 3R5, Canada; [email protected] 4 Bio Therapeutic Molecules Inc., 70 Southgate Drive, Unit 4, Guelph, ON N1G 4P5, Canada 5 Waterloo Institute for Nanotechnology, University of Waterloo, 200 University Ave W, Waterloo, ON N2L 3G1, Canada * Correspondence: [email protected]; Tel.: +1-519-888-4567 (ext. 42221) Abstract: Recently, the development of soft gelatin capsules (SGCs) dosage forms has attracted a great deal of interest in the oral delivery of poorly water-soluble drugs. This is attributed to the increased number of poorly soluble drugs in the pipeline, and hence the challenges of finding innovative ways of developing bioavailable and stable dosage forms. Encapsulation of these drugs into SGCs is one of the approaches that is utilized to deliver the active ingredients to the systemic circulation to overcome certain formulation hurdles. Once formulated, encapsulated drugs in the form of SGCs require suitable in vitro dissolution test methods to ensure drug product quality and Citation: Damian, F.; Harati, M.; Schwartzenhauer, J.; Van performance. This review focuses on challenges facing dissolution test method development for Cauwenberghe, O.; Wettig, S.D. -

1097.Full.Pdf
1521-009X/47/10/1097–1099$35.00 https://doi.org/10.1124/dmd.119.088708 DRUG METABOLISM AND DISPOSITION Drug Metab Dispos 47:1097–1099, October 2019 Copyright ª 2019 by The American Society for Pharmacology and Experimental Therapeutics Special Section on Pharmacokinetic and Drug Metabolism Properties of Novel Therapeutic Modalities—Commentary Pharmacokinetic and Drug Metabolism Properties of Novel Therapeutic Modalities Brooke M. Rock and Robert S. Foti Pharmacokinetics and Drug Metabolism, Amgen Research, South San Francisco, California (B.M.R.) and Pharmacokinetics and Drug Metabolism, Amgen Research, Cambridge, Massachusetts (R.S.F.) Received July 10, 2019; accepted July 26, 2019 Downloaded from ABSTRACT The discovery and development of novel pharmaceutical therapies in experimental and analytical tools will become increasingly is rapidly transitioning from a small molecule–dominated focus to evident, both to increase the speed and efficiency of identifying safe a more balanced portfolio consisting of small molecules, mono- and efficacious molecules and simultaneously decreasing our de- clonal antibodies, engineered proteins (modified endogenous pro- pendence on in vivo studies in preclinical species. The research and dmd.aspetjournals.org teins, bispecific antibodies, and fusion proteins), oligonucleotides, commentary included in this special issue will provide researchers, and gene-based therapies. This commentary, and the special issue clinicians, and the patients we serve more options in the ongoing as a whole, aims to highlight