Dissertation 170217
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

APPENDIX of DICTATION TEMPLATES Undergraduate Medical Education Approved By: Clerkship & Electives Commi
APPENDIX OF DICTATION TEMPLATES Undergraduate Medical Education Approved by: Clerkship & Electives Committee Date of original approval: August, 2013 Date of last review: N/A Date of next scheduled review: August, 2014 I. PURPOSE The following dictation samples are included to provide clinical clerks with guidance. II. DEFINITIONS CTU Clinical Teaching Unit MRP Most Responsible Physician PCCU Paediatric Critical Care Unit III. APPENDIX CTU - Discharge Summary Dictation Template All patients who 1) were admitted for seven or more days, and/or 2) had been admitted to the PCCU (Paediatric Critical Care Unit), and/or 3) had a complex condition or complicated course in hospital require a dictated (or typed) discharge summary. 1. Required initial information: Your name and position, most responsible physician (MRP) on the day of discharge, patient’s first and last name, PIN, who should receive this discharge summary (the MRP, the referring physician if one is known, the paediatrician or family physician of the patient (if not the referring physician), and other consultants who are going to see the patient in follow-up. Example: “This is John Smith, clinical clerk for Dr. X, dictating on patient Getme Outofhere, PIN 00000000. Please forward copies to Dr. X, Victoria Hospital, Dr. Y, family physician in London, Dr. Z, Paediatrician in London.” 2. Most responsible diagnosis: Diagnosis primarily responsible for the patient’s current admission. 3. History of present illness: Essential history of chief complaint as given by patient and/or care providers. It should include a concise summary of the relevant information from the time the symptoms started and up to the arrival at the Emergency Department. -

Theescapist 103.Pdf
originally a mass of badly dressed Call and its wide open world. Michael Escapist Forum: I very much respect characters became a group of Zenke speaks to a few radiomen at the the hard work Richard has done over the individuals, individuals selling stuff and forefront of the MMOG podcast movement. years, but I have a very hard time For me, it started way back in 1999. It talking about killing things bigger than And Dana Massey explains what Blizzard reconciling what he’s saying here with was February; I was 15. A friend of mine rats. A guy dressed like a wizard did right with World of Warcraft, but his new chosen medium. had me over to take a look at a new summoned a demon right next to me, worries none of the other players in the game he just got: Ultima Online. He then named it “a” and told it to follow field learned the correct lesson. MMOs are a poor vehicle for telling a showed me an ugly little isometric view him. Then a woman wearing nothing but story. While all MMOs HAVE a story, the of a town called Britain, though I a robe stole the sword I had in my Enjoy! players are usually so busy squabbling couldn’t figure out why - no fog or guys backpack. The whole place teemed with over mechanics or questing for loot that in furry hats. The area he referred to as possibility, and I was hooked. Yours, they couldn’t care less about WHY the bank was overrun with people, real they’re doing it. -
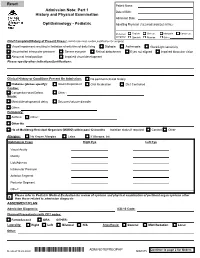
Adm Notepreophp
Patient Name: Admission Note: Part 1 Date of Birth: History and Physical Examination Admission Date: Ophthalmology - Pediatric Admitting Physician (FULL NAME W/MIDDLE INITIAL): Preferred English Chinese Mandarin Cantonese Language Spanish Russian Other: Chief Complaint/History of Present Illness: (admit note must contain justification for surgery) Visual impairment resulting in limitation of activities of daily living Diplopia Asthenopia Glare/Light sensitivity Uncontrolled intraocular pressure Severe eye pain Retinal detachment Eyes not aligned Impaired binocular vision Abnormal head position Impaired visual development Please specify other indications/justifications: Clinical History or Conditions Present On Admission: No pertinent clinical history Diabetes (please specify): Insulin Dependent Oral Medication Diet Controlled Cardiac: Congenital Heart Defect Other : Neuro: Mental/developmental delay Seizures/seizure disorder Other: Pulmonary: Asthma Other : Other Hx: Hx of Multidrug-Resistant Organism (MDRO) within past 12 months Isolation status if required: Contact Other Allergies: No Known Allergies Latex If Allergies, list: Ophthalmic Exam Right Eye Left Eye Visual Acuity Motility Lids/Adnexa Intraocular Pressure Anterior Segment Posterior Segment Other: Please refer to Pediatric Medical Evaluation for review of systems and physical examination of pertinent organ systems other X than those related to admission diagnosis ASSESMENT/PLAN Admission Diagnosis: ICD-10 Code: Planned Procedure(s) with CPT codes: FemtoSecond ORA OTHER: Laterality: Right Left Bilateral N/A Anesthesia: General MAC/Sedation Local Other: Continue to page 2 for Orders Revised 10.22.2020 *ADM NOTEPREOPHP* ADM NOTEPREOPHP ADM.075 Patient Name: Admission Note: Part 2 History and Physical Examination Date of Birth: Admission Date: Ophthalmology - Pediatric Admitting Physician (FULL NAME W/MIDDLE INITIAL): Preferred English Chinese Mandarin Cantonese Language Spanish Russian Other: 1. -

General Rules of the Marquette General Health System Medical Staff
General Rules of the Marquette General Health System Medical Staff I. PATIENT ADMISSION, ALTERNATE COVERAGE, TRANSFER, DISCHARGE AND DEATH 1.1 ADMISSION CRITERIA 1.1-1 Who may admit patients. Only a Member with admitting privileges may admit or co-admit a patient to the Hospital. Except as provided for Qualified Oral Surgeons, Podiatrists and Independent Allied Health Professionals in the Medical Staff Bylaws, a physician Member will be responsible for the general medical care and treatment of every patient admitted to the Hospital. Medical care may be provided by a Resident, other specified professional personnel or Allied Health Staff members provided they are working under the supervision of a Practitioner with clinical privileges. Medical care will be provided only by Members and Hospital support staff authorized to perform such services. 1.1-2 Admission Information. An admitting Practitioner will provide the following information in the patient’s medical record, if such information is available to the admitting Practitioner: (a) Provisional diagnosis. (b) A valid reason for admitting the patient, including information to support the medical necessity and the appropriateness of the admission. (c) Information needed to properly care for the patient being admitted. (d) Information needed to protect the patient from himself/herself. (e) Information needed to protect Hospital personnel and others from potential problems or dangers presented by the patient. (f) Information deemed necessary by the Hospital. 1.1-3 Admission of potentially suicidal or dangerous patients. If an admitting Practitioner reasonably believes a patient admitted for other purposes is potentially suicidal or dangerous to himself/herself or others, the admitting Practitioner will promptly obtain a consultation from a suitable mental health professional. -

The Complete Guide to Social Media from the Social Media Guys
The Complete Guide to Social Media From The Social Media Guys PDF generated using the open source mwlib toolkit. See http://code.pediapress.com/ for more information. PDF generated at: Mon, 08 Nov 2010 19:01:07 UTC Contents Articles Social media 1 Social web 6 Social media measurement 8 Social media marketing 9 Social media optimization 11 Social network service 12 Digg 24 Facebook 33 LinkedIn 48 MySpace 52 Newsvine 70 Reddit 74 StumbleUpon 80 Twitter 84 YouTube 98 XING 112 References Article Sources and Contributors 115 Image Sources, Licenses and Contributors 123 Article Licenses License 125 Social media 1 Social media Social media are media for social interaction, using highly accessible and scalable publishing techniques. Social media uses web-based technologies to turn communication into interactive dialogues. Andreas Kaplan and Michael Haenlein define social media as "a group of Internet-based applications that build on the ideological and technological foundations of Web 2.0, which allows the creation and exchange of user-generated content."[1] Businesses also refer to social media as consumer-generated media (CGM). Social media utilization is believed to be a driving force in defining the current time period as the Attention Age. A common thread running through all definitions of social media is a blending of technology and social interaction for the co-creation of value. Distinction from industrial media People gain information, education, news, etc., by electronic media and print media. Social media are distinct from industrial or traditional media, such as newspapers, television, and film. They are relatively inexpensive and accessible to enable anyone (even private individuals) to publish or access information, compared to industrial media, which generally require significant resources to publish information. -
Resident Supervision Attending Practitioner Responsibilities for Physician, Dental, Optometry, & Podiatry Residents
U.S. DEPARTMENT OF VETERANS AFFAIRS Resident Supervision Attending Practitioner Responsibilities for Physician, Dental, Optometry, & Podiatry Residents “Supervising Practitioner” (synonymous with “Attending”): Responsible for all care in which interns, residents or fellows are involved. “Resident” is used to apply to physician, dentist, optometrist, and podiatrist residents and fellows, regardless of training level. Documentation of all patient encounters must identify the supervising practitioner (attending) by name and indicate the level of involvement. Depending upon the clinical situation, Four types of documentation of resident supervision are allowed: 1. Attending’s progress note or other entry into the patient health record. 2. Attending’s addendum to the resident admission or progress note. 3. Co-signature by the attending implies that the attending has reviewed the resident note or other health record entry, and absent an addendum to the contrary, concurs with the content of the resident note or entry. Use of CPRS function "Additional Signer" is not acceptable for documenting supervision. 4. Resident documentation of attending supervision. [Includes involvement of the attending and the attending’s level of supervision or oversight responsibility (e.g., "I have seen and discussed the patient with my attending, Dr. 'X', and Dr. 'X' agrees with my assessment and plan"), at a minimum, the responsible attending should be identified (e.g., "The attending of record for this patient encounter is Dr. 'X'")] Outpatient: New Patient Visit (includes Emergency Department visits) Attending must be physically present in the clinic. Every patient who is new to the facility must be seen by or discussed with an attending. Documentation: An independent note, addendum to the resident's note, or resident note description of attending involvement. -

2004 February
February 2004 Games and Entertainment Megan Morrone Today you can use the same machine to organize your finances, create a presentation for your boss, and defend the Earth from flesh-eating aliens. But let’s be honest: Even with the crazy advances in software, organizing your finances and creating a presentation for your boss are still not half as much fun as defending the Earth from flesh-eating aliens.That’s why we’ve devoted the entire month of February to the noble pursuit of games and entertainment for PCs, Macs, game consoles, and PDAs. I know what you’re thinking.You’re thinking that you can skip right over this chapter because you’re not a gamer. Gamers are all sweaty, pimpled, 16-year-old boys who lock themselves in their basements sustained only by complex carbohydrates and Mountain Dew for days on end, right? Wrong.Video games aren’t just for young boys anymore. Saying you don’t like video games is like saying you don’t like ice cream or cheese or television or fun.Are you trying to tell me that you don’t like fun? If you watch The Screen Savers,you know that each member of our little TV family has a uniquely different interest in games. Morgan loves a good frag fest, whereas Martin’s tastes tend toward the bizarre (think frogs in blenders or cow tossing.) Kevin knows how to throw a cutting-edge LAN party,while Joshua and Roger like to kick back with old-school retro game emulators. I like to download free and simple low-res games that you can play on even the dinkiest PC, whereas Patrick prefers to build and rebuild the perfect system for the ultimate gaming experience (see February 13).And leave it to Leo to discover the most unique new gaming experience for the consummate early adopter (see February 1). -

Student Clerkship Guide a Comprehensive Guide to Clerkship at the Ottawa Hospital
STUDENT CLERKSHIP GUIDE A COMPREHENSIVE GUIDE TO CLERKSHIP AT THE OTTAWA HOSPITAL Gemma Cox and Stephanie Lubchansky MD 2015 CANDIDATES SPECIAL THANKS To Dr. Krista Wooller for her guidance, support, and feedback during the writing process. The Faculty of Medicine at the University of Ottawa for supporting this endeavor. EDITORS-IN-CHIEF EDITORS Gemma Cox, MD Candidate 2015 Pierre-Olivier Auclair, Mandatory Selectives Coordinator Stephanie Lubchansky, MD Candidate 2015 Dr. Contreras-Dominguez, Internal Medicine Rotation Director FACULTY SUPERVISOR Kelly Frydrych, MD Candidate 2015 Dr. Krista Wooller Julie Ghatalia, Department of Anesthesiology CONTRIBUTORS Celine Giordano, MD Candidate 2015 Kevin Dong, MD Candidate 2015 Hilary Gore, Department of Obstetrics and Bani Falcon, MD Candidate 2015 Gynecology Kelly Frydrych, MD Candidate 2015 Dr. Laura Hopkins, Obstetrics and Habibat Garuba, PGY-2 Internal Medicine Gynecology Rotation Director Celine Giordano, MD Candidate 2015 Dr. B.K. Lam, Surgery Rotation Director Anne McHale, MD Candidate 2015 Dr. Tim Lau, Department of Psychiatry Department of Pediatrics, Children’s Dr. Safeena Kherani, Mandatory Selectives Hospital of Eastern Ontario (CHEO) Rotation Director Department of Surgery, The Ottawa Anne McHale, MD Candidate 2015 Hospital Dr. Eoghan O’Shea, Family Medicine Rotation Diector Dr. Nikhil Rastogi, Anesthesiology Rotation Director Brigitte Rutherford, Department of Psychiatry Denis Vadeboncoeur, 3rd year Liaison Officer Dr. Krista Wooller, Department of Internal Medicine Amy Whyte, Department of Surgery Donna Williams, Department of Family Medicine Dr. Stella Yiu, Emergency Medicine Rotation Director Dr. Marc Zucker, Pediatrics Rotation Director A FEW WORDS FROM THE EDITORS IN CHIEF… This guide was created to help orient you, the incoming clerkship class, to the many experiences that you will encounter over the course of this year. -

Junior Doctor Skill in the Art of Physical Examination: a Retrospective Study of the Medical Admission Note Over Four Decades
Open Access Research BMJ Open: first published as 10.1136/bmjopen-2012-002257 on 3 April 2013. Downloaded from Junior doctor skill in the art of physical examination: a retrospective study of the medical admission note over four decades Charlotte M Oliver,1 Selena A Hunter,2 Takayoshi Ikeda,3 Duncan C Galletly2 To cite: Oliver CM, ABSTRACT et al ARTICLE SUMMARY Hunter SA, Ikeda T, . Objectives: To investigate the hypothesis that junior Junior doctor skill in the art doctors’ examination skills are deteriorating by assessing of physical examination: a Article focus the medical admission note examination record. retrospective study ▪ There is well-documented international evidence of the medical admission Design: Retrospective study of the admission record. supporting a declining standard in junior note over four decades. BMJ Setting: Tertiary care hospital. doctors’ physical examination skills in recent Open 2013;3:e002257. Methods: The admission records of 266 patients years. doi:10.1136/bmjopen-2012- admitted to Wellington hospital between 1975 and 2011 ▪ This study was conducted to address the 002257 were analysed, according to the total number of physical research question that this deterioration has examination observations (PEOtot), examination of the occurred locally in Wellington, New Zealand. ▸ Prepublication history for relevant system pertaining to the presenting complaint this paper are available (RelSystem) and the number of body systems examined Key messages ▪ There has been a decline in the quantity and online. To view these files (Nsystems). Subgroup analysis proceeded according to quality of the medical admission note examin- please visit the journal online admission year, level of experience of the admitting (http://dx.doi.org/10.1136/ ation records in this tertiary care centre between doctor (registrar, house surgeon (HS) and trainee intern bmjopen-2012-002257). -

Medical Record Rules and Regulations
New Hanover Regional Medical Center Rules and Regulations Medical Records Committee Review Function I. Preamble The medical record for each patient of this medical center should contain sufficient information as to identify the patient, support the diagnosis(es), justify the treatment, document the management and results as well as facilitate the continuity of care. Accordingly, the Medical Records Committee conducts quarterly analyses of medical records, or representative samples thereof, so as to assure the propriety and integrity of the medical records for the patients who seek treatment at this institution. This committee may initiate those action steps or recommendations in order to improve the timely completion, accuracy, and completeness of these records. II. Protection of the Medical Record All medical records are the property of the medical center (i.e. hospital) and are maintained for the benefit of each patient and for the healthcare providers. Records may be removed from the hospital’s jurisdiction only as pursuant to an appropriate court order, subpoena, or statute. In the case of re- admission of the patient, previous records may be available upon request for use of the attending physician. Except for current inpatients, all records which are removed from the Medical Records Department should be returned by 5 p.m. each day. III. General Medical Record Requirements All physician entries into the medical record (e.g. orders, notes, operative notes, history and physicals) shall be timed and dated. A legible identifier for services provided/ordered is requested. The method used shall be hand written or an electronic signature (stamp signatures are not acceptable) to sign an order or other medical record documentation. -

The Value of the Physical Examination in Clinical Practice: an International Survey
ORIGINAL RESEARCH Clinical Medicine 2017 Vol 17, No 6: 490–8 T h e v a l u e o f t h e p h y s i c a l e x a m i n a t i o n i n c l i n i c a l p r a c t i c e : an international survey Authors: A n d r e w T E l d e r , A I C h r i s M c M a n u s ,B A l a n P a t r i c k , C K i c h u N a i r , D L o u e l l a V a u g h a n E a n d J a n e D a c r e F A structured online survey was used to establish the views of the act of physically examining a patient sits at the very heart 2,684 practising clinicians of all ages in multiple countries of the clinical encounter and is vital in establishing a healthy about the value of the physical examination in the contempo- therapeutic relationship with patients.7 Critics of the physical rary practice of internal medicine. 70% felt that physical exam- examination cite its variable reproducibility and the utility of ination was ‘almost always valuable’ in acute general medical more sensitive bedside tools, such as point of care ultrasound, ABSTRACT referrals. 66% of trainees felt that they were never observed by in place of traditional methods.2,8 a consultant when undertaking physical examination and 31% Amid this uncertainty, there is little published information that consultants never demonstrated their use of the physical describing clinicians’ opinions about the value of physical examination to them. -

Welcome to Twit.Tv! If You've Stumbled Upon This Page and Are Wondering What It's All About, Read On
Huh? Welcome to TWiT.tv! If you've stumbled upon this page and are wondering what it's all about, read on. The TWiT.tv Story It all started in 1998 with a small cable network called ZDTV, a channel dedicated to covering computers, the Internet, and personal technology. The people behind this site all worked on that network as hosts, reporters, or producers. In 2004, ZDTV, then called TechTV, was sold and dismantled. Former TechTV hosts, Leo Laporte, Patrick Norton, Kevin Rose, and John C. Dvorak, and producers Robert Heron, David Prager, and Roger Chang went on to other jobs, but we stayed in touch, with each other, and with fans of the late TechTV. Those fans told us again and again how important TechTV had been in their lives, and how much they missed the channel. We missed working with each other, too. On a rainy evening in January, 2005 a few of of us got together for dinner after spending the day covering MacWorld Expo in San Francisco. Leo, who was working as a radio host, happened to have a microphone and recorder. He turned it on and recorded 20 minutes of idle chatter about the Expo and the tech world in general. He posted that recording on his web site. Within a few days tens of thousands of people had downloaded the recording. TechTV fans began clamoring for more. A few months later,TWiT was born. We originally called the show The Revenge of The Screen Savers because that was the name of the defunct TV show many of us had worked on, but the cable channel that had bought TechTV complained, so we changed the name to this WEEK in TECH, or TWiT, for short.