Ratio of Phosphate to Amino Acids
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Hydroxylation of the Eukaryotic Ribosomal Decoding Center Affects Translational Accuracy
Hydroxylation of the eukaryotic ribosomal decoding center affects translational accuracy Christoph Loenarza,1, Rok Sekirnika,2, Armin Thalhammera,2, Wei Gea, Ekaterina Spivakovskya, Mukram M. Mackeena,b,3, Michael A. McDonougha, Matthew E. Cockmanc, Benedikt M. Kesslerb, Peter J. Ratcliffec, Alexander Wolfa,4, and Christopher J. Schofielda,1 aChemistry Research Laboratory and Oxford Centre for Integrative Systems Biology, University of Oxford, Oxford OX1 3TA, United Kingdom; bTarget Discovery Institute, University of Oxford, Oxford OX3 7FZ, United Kingdom; and cCentre for Cellular and Molecular Physiology, University of Oxford, Oxford OX3 7BN, United Kingdom Edited by William G. Kaelin, Jr., Harvard Medical School, Boston, MA, and approved January 24, 2014 (received for review July 31, 2013) The mechanisms by which gene expression is regulated by oxygen Enzyme-catalyzed hydroxylation of intracellularly localized are of considerable interest from basic science and therapeutic proteins was once thought to be rare, but accumulating recent perspectives. Using mass spectrometric analyses of Saccharomyces evidence suggests it is widespread (11). Motivated by these cerevisiae ribosomes, we found that the amino acid residue in findings, we investigated whether the translation of mRNA to closest proximity to the decoding center, Pro-64 of the 40S subunit protein is affected by oxygen-dependent modifications. A rapidly ribosomal protein Rps23p (RPS23 Pro-62 in humans) undergoes growing eukaryotic cell devotes most of its resources to the tran- posttranslational hydroxylation. We identify RPS23 hydroxylases scription, splicing, and transport of ribosomal proteins and rRNA as a highly conserved eukaryotic subfamily of Fe(II) and 2-oxoglu- (12). We therefore reasoned that ribosomal modification is a tarate dependent oxygenases; their catalytic domain is closely re- candidate mechanism for the regulation of protein expression. -

Significance of Urinary Hydroxyproline in Man
SIGNIFICANCE OF URINARY HYDROXYPROLINE IN MAN Darwin J. Prockop, Albert Sjoerdsma J Clin Invest. 1961;40(5):843-849. https://doi.org/10.1172/JCI104318. Find the latest version: https://jci.me/104318/pdf SIGNIFICANCE OF URINARY HYDROXYPROLINE IN MAN By DARWIN J. PROCKOP AND ALBERT SJOERDSMA (From the Section of Experimental Therapeutics, National Heart Institute, Bethesda, Md.) (Submitted for publication September 27, 1960; accepted January 12, 1961) Since nearly all of the hydroxyproline of the of Marfan's syndrome (2) reflect a rapid rate of body is found in collagen, it has been suggested collagen degradation. (1, 2) that the urinary excretion of this imino An incidental discovery in the study was that acid may be an important index of collagen me- the increase in urinary hydroxyproline after in- tabolism. The origin of urinary hydroxyproline, gestion of gelatin represents an increased excre- however, is not definitely established. The iso- tion of hydroxyproline peptides. This appears to topic studies of Stetten (3) in rats indirectly sug- be the first demonstration that significant amounts gested that most of the free and peptide hydroxy- of peptides can be excreted following ingestion of proline in the body arises from the breakdown of a protein. collagen, since she found that hydroxyproline-N'5 was not significantly incorporated into collagen. MATERIALS AND METHODS Ziff, Kibrick, Dresner and Gribetz (1), on the The 8 subjects utilized in the study were hospitalized other hand, observed an increased excretion of for periods of 3 to 12 weeks; 3 were patients with Mar- hydroxyproline when it was added to the diet of fan's syndrome, 2 of whom were previously shown to have elevated excretions of hydroxyproline (2). -

Subject Index
Cambridge University Press 0521462924 - Amino Acids and Peptides G. C. Barrett and D. T. Elmore Index More information Subject index acetamidomalonate synthesis 123–4 in fossil dating 15 S-adenosyl--methionine 11, 12, 174, 181 in geological samples 15 alanine, N-acetyl 9 in Nature 1 structure 4 IR spectrometry 36 alkaloids, biosynthesis from amino acids 16–17 isolation from proteins 121 alloisoleucine 6 mass spectra 61 allosteric change 178 metabolism, products of 187 allothreonine 6 metal-binding properties 34 Alzheimer’s disease 14 NMR 41 amidation at peptide C-terminus 57, 94, 181 physicochemical properties 32 amides, cis–trans isomerism 20 protein 3 N-acylation 72 PTC derivatives 87 N-alkylation 72 quaternary ammonium salts 50 hydrolysis 57 reactions of amino group 49, 51 O-trimethylsilylation 72 reactions of carboxy group 49, 53 reduction to -aminoalkanols 72 racemisation 56 amidocarbonylation in amino acid synthesis 125 routine spectrometry 35 amino acids, abbreviated names 7 Schöllkopf synthesis 127–8 acid–base properties 32 Schiff base formation 49 antimetabolites 200 sequence determination 97 et seq. as food additives 14 following selective chemical degradation 107 as neurotransmitters 17 following selective enzymic degradation 109 asymmetric synthesis 127 general strategy for 92 - 17–18 identification of C-terminus 106–7 biosynthesis 121 identification of N-terminus 94, 97 biosynthesis from, of creatinine 183 by solid-phase methodology 100 of nitric oxide 186 by stepwise chemical degradation 97 of porphyrins 185 by use of dipeptidyl -

A Few Experimental Suggestions Using Minerals to Obtain Peptides with a High Concentration of L-Amino Acids and Protein Amino Acids
S S symmetry Hypothesis A Few Experimental Suggestions Using Minerals to Obtain Peptides with a High Concentration of L-Amino Acids and Protein Amino Acids Dimas A. M. Zaia 1,* and Cássia Thaïs B. V. Zaia 2 1 Laboratório de Química Prebiótica-LQP, Departamento de Química, Universidade Estadual de Londrina, CEP 86 057-970 Londrina, Brazil 2 Laboratório de Fisiologia Neuroendocrina e Metabolismo–LaFiNeM, Departamento de Ciências Fisiológicas, Universidade Estadual de Londrina, CEP 86 057-970 Londrina, Brazil; [email protected] * Correspondence: [email protected] Received: 9 October 2020; Accepted: 25 November 2020; Published: 10 December 2020 Abstract: The peptides/proteins of all living beings on our planet are mostly made up of 19 L-amino acids and glycine, an achiral amino acid. Arising from endogenous and exogenous sources, the seas of the prebiotic Earth could have contained a huge diversity of biomolecules (including amino acids), and precursors of biomolecules. Thus, how were these amino acids selected from the huge number of available amino acids and other molecules? What were the peptides of prebiotic Earth made up of? How were these peptides synthesized? Minerals have been considered for this task, since they can preconcentrate amino acids from dilute solutions, catalyze their polymerization, and even make the chiral selection of them. However, until now, this problem has only been studied in compartmentalized experiments. There are separate experiments showing that minerals preconcentrate amino acids by adsorption or catalyze their polymerization, or separate L-amino acids from D-amino acids. Based on the [GADV]-protein world hypothesis, as well as the relative abundance of amino acids on prebiotic Earth obtained by Zaia, several experiments are suggested. -

Neurotransmitters-Drugs Andbrain Function.Pdf
Neurotransmitters, Drugs and Brain Function. Edited by Roy Webster Copyright & 2001 John Wiley & Sons Ltd ISBN: Hardback 0-471-97819-1 Paperback 0-471-98586-4 Electronic 0-470-84657-7 Neurotransmitters, Drugs and Brain Function Neurotransmitters, Drugs and Brain Function. Edited by Roy Webster Copyright & 2001 John Wiley & Sons Ltd ISBN: Hardback 0-471-97819-1 Paperback 0-471-98586-4 Electronic 0-470-84657-7 Neurotransmitters, Drugs and Brain Function Edited by R. A. Webster Department of Pharmacology, University College London, UK JOHN WILEY & SONS, LTD Chichester Á New York Á Weinheim Á Brisbane Á Singapore Á Toronto Neurotransmitters, Drugs and Brain Function. Edited by Roy Webster Copyright & 2001 John Wiley & Sons Ltd ISBN: Hardback 0-471-97819-1 Paperback 0-471-98586-4 Electronic 0-470-84657-7 Copyright # 2001 by John Wiley & Sons Ltd. Bans Lane, Chichester, West Sussex PO19 1UD, UK National 01243 779777 International ++44) 1243 779777 e-mail +for orders and customer service enquiries): [email protected] Visit our Home Page on: http://www.wiley.co.uk or http://www.wiley.com All Rights Reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic, mechanical, photocopying, recording, scanning or otherwise, except under the terms of the Copyright, Designs and Patents Act 1988 or under the terms of a licence issued by the Copyright Licensing Agency Ltd, 90 Tottenham Court Road, London W1P0LP,UK, without the permission in writing of the publisher. Other Wiley Editorial Oces John Wiley & Sons, Inc., 605 Third Avenue, New York, NY 10158-0012, USA WILEY-VCH Verlag GmbH, Pappelallee 3, D-69469 Weinheim, Germany John Wiley & Sons Australia, Ltd. -

(12) Patent Application Publication (10) Pub. No.: US 2007/0254315 A1 Cox Et Al
US 20070254315A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2007/0254315 A1 Cox et al. (43) Pub. Date: Nov. 1, 2007 (54) SCREENING FOR NEUROTOXIC AMINO (60) Provisional application No. 60/494.686, filed on Aug. ACID ASSOCATED WITH NEUROLOGICAL 12, 2003. DSORDERS Publication Classification (75) Inventors: Paul A. Cox, Provo, UT (US); Sandra A. Banack, Fullerton, CA (US); Susan (51) Int. Cl. J. Murch, Cambridge (CA) GOIN 33/566 (2006.01) GOIN 33/567 (2006.01) Correspondence Address: (52) U.S. Cl. ............................................................ 435/721 PILLSBURY WINTHROP SHAW PITTMAN LLP (57) ABSTRACT ATTENTION: DOCKETING DEPARTMENT Methods for screening for neurological disorders are dis P.O BOX 105OO closed. Specifically, methods are disclosed for screening for McLean, VA 22102 (US) neurological disorders in a Subject by analyzing a tissue sample obtained from the subject for the presence of (73) Assignee: THE INSTITUTE FOR ETHNO elevated levels of neurotoxic amino acids or neurotoxic MEDICINE, Provo, UT derivatives thereof associated with neurological disorders. In particular, methods are disclosed for diagnosing a neu (21) Appl. No.: 11/760,668 rological disorder in a subject, or predicting the likelihood of developing a neurological disorder in a Subject, by deter (22) Filed: Jun. 8, 2007 mining the levels of B-N-methylamino-L-alanine (BMAA) Related U.S. Application Data in a tissue sample obtained from the subject. Methods for screening for environmental factors associated with neuro (63) Continuation of application No. 10/731,411, filed on logical disorders are disclosed. Methods for inhibiting, treat Dec. 8, 2003, now Pat. No. 7,256,002. -

Chemical Methods for the Characterization of Proteolysis in Cheese During Ripening Plh Mcsweeney, Pf Fox
Chemical methods for the characterization of proteolysis in cheese during ripening Plh Mcsweeney, Pf Fox To cite this version: Plh Mcsweeney, Pf Fox. Chemical methods for the characterization of proteolysis in cheese during ripening. Le Lait, INRA Editions, 1997, 77 (1), pp.41-76. hal-00929515 HAL Id: hal-00929515 https://hal.archives-ouvertes.fr/hal-00929515 Submitted on 1 Jan 1997 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Lait (1997) 77, 41-76 41 © ElseviernNRA Review Chemical methods for the characterization of proteolysis in cheese during ripening PLH McSweeney, PF Fox Department of Food Chemistry, University College, Cork, Ireland Summary - Proteolysis is the principal and most complex biochemical event which occurs during the maturation of most cheese varieties. Proteolysis has been the subject of much study and a range of analytieal techniques has been developed to assess its extent and nature. Methods for assessing pro- teolysis can he c1assified under two broad headings: non-specifie and specifie techniques, both of which are reviewed. Non-specifie techniques include the quantitation of nitrogen soluble in various extrac- tants or precipitants and the Iiberation of reactive groups. -
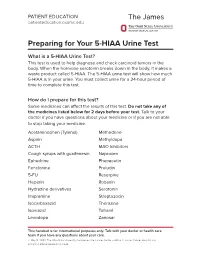
Preparing for Your 5-HIAA Urine Test
PATIENT EDUCATION patienteducation.osumc.edu Preparing for Your 5-HIAA Urine Test What is a 5-HIAA Urine Test? This test is used to help diagnose and check carcinoid tumors in the body. When the hormone serotonin breaks down in the body, it makes a waste product called 5-HIAA. The 5-HIAA urine test will show how much 5-HIAA is in your urine. You must collect urine for a 24-hour period of time to complete this test. How do I prepare for this test? Some medicines can affect the results of this test.Do not take any of the medicines listed below for 2 days before your test. Talk to your doctor if you have questions about your medicine or if you are not able to stop taking your medicine. Acetaminophen (Tylenol) Methedrine Aspirin Methyldopa ACTH MAO Inhibitors Cough syrups with guaifenesin Naproxen Ephedrine Phenacetin Fenclonine Preludin 5-FU Reserpine Heparin Robaxin Hydrazine derivatives Serotonin Imipramine Streptozocin Isocarboxazid Thorazine Isoniazid Tofranil Levodopa Zanosar This handout is for informational purposes only. Talk with your doctor or health care team if you have any questions about your care. © May 14, 2020. The Ohio State University Comprehensive Cancer Center – Arthur G. James Cancer Hospital and Richard J. Solove Research Institute. There are certain foods and drinks that you should not eat or drink before this test. Do not eat or drink any of the items below for 4 days before the test or during the test. Avocados Grapefruit Bananas Honeydew Coffee/Tea Kiwi Cantaloupe Pineapple Dates Plantains Eggplant Plums Tomatoes / tomato products Nuts (walnuts, pecans, hickory nuts, butternuts) • Do not drink alcoholic beverages for 2 days before or during the test. -

付表 ⅠA 指定を受けた医薬の有効成分 Annex ⅠA Designated
付表ⅠA 指定を受けた医薬の有効成分 Annex ⅠA Designated Pharmaceutical Active Ingredients 号(Sub-heading) 品名 Description 2818.30 アルゲルドラート algeldrate 2833.22 アルスルフ alusulf 2842.10 アルマシラート almasilate 2842.10 シマルドラート simaldrate 2842.90 硫酸アルマドラ ート almadrate sulfate 2842.90 アルマガート almagate 2842.90 カルバルドラード carbaldrate 2842.90 ヒドロタルシト hydrotalcite 2842.90 マガルドラート magaldrate 2843.30 オーラノフィン auranofin 2843.30 金チオグリカニド aurothioglycanide 2843.30 金チオりんご酸ナトリウム sodium aurothiomalate 2843.30 金チオ硫酸ナトリウム sodium aurotiosulfate 2843.90 カルボプラチン carboplatin 2843.90 シスプラチン cisplatin 2843.90 デキソルマプラチン dexormaplatin 2843.90 エンロプラチン enloplatin 2843.90 イプロプラチン iproplatin 2843.90 ロバプラチン lobaplatin 2843.90 ミボプラチン miboplatin 2843.90 ネダプラチン nedaplatin 2843.90 オルマプラチン ormaplatin 2843.90 オキサリプラチン oxaliplatin 2843.90 セブリプラチン sebriplatin 2843.90 スピロプラチン spiroplatin 2843.90 ゼニプラチン zeniplatin 2844.40 アルツモマブ altumomab 2844.40 塩化セシウム(131Cs) cesium (131 Cs) chloride 2844.40 クロルメロドリン(197Hg) chlormerodrin (197 Hg) 2844.40 シアノコバラミン(57Co) cyanocobalamin (57 Co) 2844.40 シアノコバラミン(58Co) cyanocobalamin (58 Co) 2844.40 シアノコバラミン(60Co) cyanocobalamin (60 Co) 2844.40 エチオダイズド油(131I) ethiodized oil (131 I) 2844.40 くえん酸第二鉄(59Fe)注射液 ferric (59 Fe) citrate in 2844.40 フィブリノゲン(125I) fibrinogen (125 I) 2844.40 フルデオキシグルコー ス(18F) fludeoxyglucose ( 18 F) 2844.40 フルオロドパ(18F) fluorodopa (18 F) 2844.40 くえん酸ガリウム(67Ga) gallium (67 Ga) citrate 2844.40 金コロイド(198Au) gold (198 Au), colloidal 2844.40 イオベングアン(131I) iobenguane (131 I) 2844.40 よう化人血清アルブミン(125I) iodinated (125 I) human serum albumin 2844.40 よう化人血清アルブミン(131I) iodinated -

Designing Peptidomimetics
CORE Metadata, citation and similar papers at core.ac.uk Provided by UPCommons. Portal del coneixement obert de la UPC DESIGNING PEPTIDOMIMETICS Juan J. Perez Dept. of Chemical Engineering ETS d’Enginyeria Industrial Av. Diagonal, 647 08028 Barcelona, Spain 1 Abstract The concept of a peptidomimetic was coined about forty years ago. Since then, an enormous effort and interest has been devoted to mimic the properties of peptides with small molecules or pseudopeptides. The present report aims to review different approaches described in the past to succeed in this goal. Basically, there are two different approaches to design peptidomimetics: a medicinal chemistry approach, where parts of the peptide are successively replaced by non-peptide moieties until getting a non-peptide molecule and a biophysical approach, where a hypothesis of the bioactive form of the peptide is sketched and peptidomimetics are designed based on hanging the appropriate chemical moieties on diverse scaffolds. Although both approaches have been used in the past, the former has been more widely used to design peptidomimetics of secretory peptides, whereas the latter is nowadays getting momentum with the recent interest in designing protein-protein interaction inhibitors. The present report summarizes the relevance of the information gathered from structure-activity studies, together with a short review on the strategies used to design new peptide analogs and surrogates. In a following section there is a short discussion on the characterization of the bioactive conformation of a peptide, to continue describing the process of designing conformationally constrained analogs producing first and second generation peptidomimetics. Finally, there is a section devoted to review the use of organic scaffolds to design peptidomimetics based on the information available on the bioactive conformation of the peptide. -

Preparation of N-‐(Boc)-‐Allylglycine Methyl Ester
Preparation of N-(Boc)-Allylglycine Methyl Ester Using a Zinc-mediated, Palladium-catalyzed Cross-coupling Reaction N. D. Prasad Atmuri and William D. Lubell* Département de Chimie, Université de Montréal, P.O. Box 6128, Station Centre-ville, Montréal, QC H3C 3J7, Canada Checked by Jean-Nicolas Desrosiers, Nizar Haddad, and Chris H. Senanayake Iodine (1.3 equiv), Ph3P (1.3 equiv), OH Imidazole (1.3 equiv) I A. DCM, 0 °C - rt BocHN CO2Me 82% BocHN CO2Me 1 2 1. Zn (6 equiv), DMF Br Br (0.6 equiv), 60 °C I TMSCl (0.2 equiv), rt - 35 °C B. BocHN CO Me BocHN CO2Me 2 2. Br (1 M in THF) 2 3 Pd2(dba)3 (0.02 equiv) P(o-tol)3 (0.1 equiv) –78 °C - rt, 12 h 65% Procedure A. tert-Butyl (R)-1-(methoxycarbonyl)-2-iodoethylcarbamate (2). An oven- dried 1000-mL, three-necked, round-bottomed flask containing an egg- shaped Teflon®-coated magnetic stir bar (7 cm long) is equipped with a rubber septum with a thermometer, a 125 mL addition funnel and an argon inlet adaptor. The apparatus is purged with argon (Note 1). Keeping a Org. Synth. 2015, 92, 103-116 103 Published on the Web 4/6/2015 DOI: 10.15227/orgsyn.092.0103 © 2015 Organic Syntheses, Inc. positive flow of argon, the septum is removed temporarily and the flask is charged with triphenylphosphine (Note 2) (32.66 g, 124.5 mmol, 1.3 equiv) and 400 mL of dichloromethane (Note 3). The solution is stirred at room temperature and imidazole (8.47 g, 124.5 mmol, 1.3 equiv) (Note 2) is added in one portion. -

Interpretive Guide for Amino Acids
Interpretive Guide for Amino Acids Intervention Options LOW HIGH Essential Amino Acids Arginine (Arg) Arg Mn Histidine (His) Folate, His Isoleucine (Ile) * B6, Check for insulin insensitivity Leucine (Leu) * B6, Check for insulin insensitivity Lysine (Lys) Carnitine Vitamin C, Niacin, B6, Iron, a-KG Methionine(Met) * B6, á-KG, Mg, SAM Phenylalanine (Phe) * Iron,VitaminC,Niacin,LowPhediet Threonine(Thr) * B6, Zn Tryptophan(Trp) Trpor5-HTP Niacin, B6 Valine (Val) * B6, Check for insulin insensitivity Essential Amino Acid Derivatives Neuroendocrine Metabolism y-Aminobutyric Acid (GABA) a-KG, B6 Glycine (Gly) Gly Folate, B6,B2,B5 Serine (Ser) B6, Mn, Folate * Taurine (Tau) Tau, B6 Vit. E, Vit. C, B-Carotene, CoQ10, Lipoate Tyrosine(Tyr) Iron,Tyr,VitaminC,Niacin Cu, Iron, Vitamin C, B6 Ammonia/Energy Metabolism a-Aminoadipic Acid B6, a-KG Asparagine (Asn) Mg Aspartic Acid (Asp) a-KG, B6 Mg, Zn Citrulline (Cit) Mg, Aspartic acid Glutamic Acid (Glu) B6, a-KG Niacin, B6 Glutamine (Gln) a-KG, B6 Ornithine (Orn) Arg Mg, a-KG, B6 Sulfur Metabolism Cystine (Cys) NAC B2 Cystathionine B6 Homocystine (HCys) B6, Folate, B12, Betaine Additional Metabolites a-Amino-N-Butyric Acid a-KG, B6 B6, a-KG Alanine (Ala) * B6 Anserine Zn n-Alanine Lactobacillus and Bifidobacteria, B6 n-Aminoisobutyric Acid B6 Carnosine Zn Ethanolamine Mg Hydroxylysine (HLys) Vitamin C, Iron, a-KG Hydroxyproline (HPro) Vitamin C, Iron, a-KG 1-Methylhistidine Vitamin E, B12, Folate 3-Methylhistidine BCAAs, Vit. E, Vit. C, n-Carotene, CoQ10, Lipoate Phosphoethanolamine (PE) SAM, B12, Folate, Betaine Phosphoserine Mg Proline (Pro) a-KG Vitamin C, Niacin Sarcosine B2 * Use balanced or custom mixtures of essential amino acids Nordic Laboratiroes∙ Nygade 6, 3.sal ∙ 1164 Copenhagen K ∙ DenmarkTel: +45 33 75 1000 ∙ e-mail: [email protected] In association with ©Metametrix, Inc.