Downsizing the Massachusetts Mental Health System: the Olitp Ics of Evasion Richard A
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Emergency Behavioral Health Services
ALERT #24 ___________________ October 5, 2007 EMERGENCY BEHAVIORAL HEALTH SERVICES POLICIES AND PROCEDURES FOR EMERGENCY SERVICES PROGRAMS AND HOSPITAL EMERGENCY DEPARTMENTS FOR MBHP MEMBERS AND UNINSURED CONSUMERS The following information should be communicated immediately to other appropriate staff in your organization. The Massachusetts Behavioral Health Partnership (MBHP) is the company that manages behavioral health (mental health and substance abuse) services for MassHealth’s Primary Care Clinician (PCC) Plan Members*. Additionally, MBHP is contracted with the Department of Mental Health to manage most of the Emergency Services Programs (ESPs) across the Commonwealth. In that role, MBHP is issuing this Alert to hospital Emergency Departments (EDs), MBHP network providers, and other interested stakeholders in order to provide clarification and guidance relative to the management of behavioral health emergencies in the ED setting. More specifically, this Alert delineates the roles and responsibilities of the Emergency Services Programs (ESPs) and describes an individual’s progression through this system, with a goal of expediting his or her movement through the hospital ED and into acute behavioral health services, as medically necessary. ESPs function as a “safety net” for all citizens of the Commonwealth regardless of age, payer, or ability to pay. It is important to note that the policies and procedures in this Alert applies to those populations for whom the ESPs are contracted with MBHP to serve, which includes MBHP members, MassHealth (non-MCO enrolled) Members, uninsured consumers, and DMH consumers. However, it is also important to note that MassHealth also requires the four Managed Care Organizations (MCOs) contracted with MassHealth to utilize the ESP system for emergency behavioral health services for MassHealth MCO enrolled Members. -

2004 Annual Report July 1, 2003 to June 30, 2004 Massachusetts Department of Mental Health
2004 Annual Report July 1, 2003 to June 30, 2004 Massachusetts Department of Mental Health Mitt Romney Governor Ronald Preston Secretary Elizabeth Childs, M.D. Commissioner “Bloom” — a public art installation of 28,000 pots of flowers at the Massachusetts Mental Health Center in November 2003 by artist Anna Schuleit commemorating the hospital’s closing. Mission The mission of the Department of Mental Health is to improve the quality of life for adults with serious and persistent mental illness and children with serious mental illness or severe emotional disturbance. This is accomplished by ensuring access to an integrated network of effective and effi- cient and culturally competent mental health services that promote consumer rights, responsibili- ties, rehabilitation, and recovery. Guiding Principles Provide responsive, high quality, cost effective services Focus support on the most vulnerable citizens of the Commonwealth Design programs using current scientific research, evaluation studies, and program outcome data Promote opportunities for individuals with mental illness to participate in rehabilitation and recov- ery no matter how severe their symptoms or pervasive their illness Offer individuals appropriate choices among services tailored to meet their unique needs Value managers who engage their colleagues and staff in entrepreneurial, innovative leadership that will improve the system Value input from a wide public audience and recognize that community advocacy and advisory groups are an essential component of system planning -

Annual Report of the Massachusetts Commission on Mental Diseases Of
TH** •O0«-»iA Public Document No. 117 SECOND ANNUAL EEPOET Massachusetts Commission on Mental Diseases THE COMMONWEALTH OF MASSACHUSETTS Year ending November 30, 1917. BOSTON: WRIGHT & POTTER PRINTING CO., STATE PRINTERS, 32 DERNE street. 1918. Publication of this Document approved by the Supervisor of Administration. TABLE OF CONTENTS. * PAGE Members of the Commission and List of Officers, 5 Letter of Transmission to Governor and Council, 7 Duties of the Commission, ..... 9,10 Activities of the Commission, ..... 10-15 Review of the Year: — All Classes under Care, ..... 16,17 The Insane, ....... 17-23 The Feeble-minded, . 23,24 The Epileptic, ....... 24,25 Report of the Pathologist, ..... 25-54 Reports of Committees on Nursing Service, . 54-61 Out-patient Departments, ..... 61-71 Commitments for Observation and Temporary Care, 71-73 Stability of Service, ...... 74,75 Capacity for Patients, ..... 76-78 Institutions : — Public 79-127 Private, . 127-130 Unlicensed Homes, . 131 Family Care of the Insane, .... 131-134 The Commission: — Proceedings of, . 135 Plans and Specifications, ..... 135 Estimates of State Expenses for 1918: — The Commission, 135, 136 Maintenance Appropriations, 136-138 Special Appropriations, .... 139-142 Financial Statement of Commission, 143, 144 Support Department, ..... 145-148 Deportations, ....... 148, 149 Transfers, ....... 150 Financial Department, . 150 General Matters : — New Legislation, ...... 151-160 Nineteen-year Statement as to Special Appropriations, 160-162 Financial Statistics, ....... 163-201 General Statistics, ....... 203-265 Directors^ of Institutions, ...... 266-278 Index, ......... 279-286 Digitized by the Internet Archive in 2010 with funding from Boston Library Consortium IVIember Libraries http://www.archive.org/details/annualreportofma1917mass2 Members of the Massachusetts Commission on Mental Diseases. -

Environmental Protection Agency § 52.1126
Environmental Protection Agency § 52.1126 these areas. The inventories consist of lease potential (approximately equiva- emission estimates of volatile organic lent to 1 percent sulfur content.) compounds and nitrogen oxides, and Deerfield Specialty Paper Company, Monroe cover point, area, non-road mobile, on- Bridge; Amherst College, Amherst; Brown road mobile and biogenic sources. The Company, Holyoke; Monsanto Polymer and inventories were submitted as revisions Petrochemical Company, Building 21, to the SIP in partial fulfillment of ob- Springfield; Monsanto Polymer and Petro- ligations for nonattainment areas chemical Company, Building 49, Spring- under EPA’s 1997 8-hour ozone stand- field; Mount Holyoke College, South Had- ard. ley; Uniroyal Tire Inc., Chicopee; Smith College, Northampton; West Springfield [62 FR 37514, July 14, 1997, as amended at 77 Generating Station, Western Massachu- FR 50601, Aug. 22, 2012] setts Electric, West Springfield. § 52.1126 Control strategy: Sulfur ox- Pioneer Valley APCD ides. Belchertown State School, Belchertown (a) The revisions to the control strat- James River Graphics (formerly Scott egy resulting from the modification to Graphics), south Hadley (conditioned upon the emission limitations applicable to operation of the boilers on only one of the the sources listed below or resulting two stacks at any given time, and oper- ation being so restricted in the source’s op- from the change in the compliance erating permit granted by the Massachu- date for such sources with the applica- setts Department of Environmental Qual- ble emission limitation is hereby ap- ity Engineering.) proved. All regulations cited are air Massachusetts Mutual Life Insurance Com- pollution control regulations of the pany, Springfield. -

Annual Report of the Trustees of the Danvers State Hospital
: Public Document No. 20 THIRTY-EIGHTH ANNUAL REPORT THE TRUSTEES Danvers State Hospital, DANVERS, MASS. (POST-OFFICE, HATHORNE), Yeak ending November 30, 1915. BOSTON WEIGHT & POTTER PRINTING CO., STATE PRINTERS, 32 DERNE STREET. 1916. Approved by The State Board of Publication. CONTENTS. Organization of Hospital, . 5 Report op Trustees, 15 Report of Superintendent, 18 Report of Clinical Groups, 66 64 Report of Treasurer, . Statistics, 71 OFFICERS OF THE DANVERS STATE HOSPITAL. Nov. 30, 1915. TRUSTEES. Mr. S. Herbert Wilkins, Chairman, . Salem. Mr. Seward W. Jones, Newton Highlands. Mr. Ernest B. Dane, Boston. Miss Annie M. Kilham, Beverly. Mr. Samuel Cole, Corresponding Secretary, Beverly. Mr. Dan A. Donahue, Salem. Miss Mary Ward Nichols, Recording Secretary. Danvers. RESIDENT OFFICERS. George M. Kline, M.D., . Physician and Superintendent. John B. Macdonald, M.D., Physician and Assistant Superin- tendent. Nelson G. Trueman, M.D., Assistant Physician. William J. Thompson, M.D., Assistant Physician. Alice M. Patterson, M.D., Assistant Physician. David T. Brewster, M.D., Assistant Physician. Alfred P. Chronquest, M.D., Assistant Physician. NONRESIDENT OFFICERS. Lawson G. Lowret, M.D., Pathologist. Mr. Horace M. Brown, Treasurer and Clerk. Mr. Scott Whitcher, Steward. HEADS OF DEPARTMENTS. Mr. Adam D. Smith, . Supervisor Male Department. Miss Eunice A. Fisk, Superintendent of Nurses and Prin- cipal of Training School. Mrs. Harriet A. Read, Supervisor Female Department. Mr. Carl A. Lindgren, Engineer. Mr. Junius C. Wing, Farmer. Mr. George W. Gardner, Carpenter. CONSULTING BOARD OF PHYSICIANS. Dr. Francis W. Anthony, 112 Main Street, Haverhill. Dr. William Howe Merrill, "The Bay State," Lawrence. Dr. Edward M. Greene, 20 Mt. -

2020 Mps Outstanding Psychiatrist Awards
2020 MPS OUTSTANDING PSYCHIATRIST AWARDS PSYCHIATRIC EDUCATION - Lewis Kirshner, MD, DLFAPA Dr. Lewis Kirshner received his BA in anthropology with honors and distinction from Wesleyan University. He earned his medical degree at Jefferson Medical College and did his internship at Mt. Zion Hospital in San Francisco. He then pursued a residency in psychiatry on the Albert Einstein College of Medicine service at the Bronx Municipal Hospital Center. After serving as Captain in the USAF for two years, Dr. Kirshner came to Boston where he did a fellowship at the Harvard University Health Service. He also trained in psychoanalysis at the Boston Psychoanalytic Institute where he later attained the rank of Training and Supervising Analyst. Dr. Kirshner was certified by the American Board of Psychiatry and Neurology and, also by the Board of Professional Standards of the American Psychoanalytic Association; and is a distinguished life fellow of the American Psychiatric Association. Dr. Kirshner was founding director of the inpatient psychiatric service at Mt. Auburn Hospital where he served for five years before becoming director of the Metropolitan Beaverbrook Community Mental Health Center. He later moved to the Harvard Community Health Plan in Wellesley where he served for 11 years as Chief of Mental Health Services. During this time, Dr. Kirshner was also developing his private practice of psychotherapy and psychoanalysis. In 1992, Dr. Kirshner joined the staff of the Brockton VA Medical Center. At that time the Harvard South Shore Psychiatry Residency Training Program was seeking independent accreditation, and Dr. Kirshner was recruited to design and to implement the psychotherapy training module and to serve as part-time faculty on this Harvard Medical School service. -

AN INVESTIGATION of the MENTAL HOSPITAL BUILDING TYPE Irvin J
AN INVESTIGATION OF THE MENTAL HOSPITAL BUILDING TYPE Irvin J. Kohler August 1954 Submitted to the faculty of the Department of Architecture, Massachusetts Institute of Technology, in partial fulfillment of masterts thesis study, 1954. FOREWARD This study is concerned with the application of .the disciplines of architecture to the problems of the care and treatment of the mentally ill. I feel that there is sufficient justification to demand the re-thinking of build- ings housing the patient's treatment and living facilities to make them more in keeping with our standards of contem- porary achievements in both architecture and psychiatry. The limitations of such a study were: the study, itself; the personal limitations of the investigator; and the presentation. The gap between architecture and psy- chiatry is tremendous. Each is a field unto itself, but the two must be joined together if there is to be a satisfactory solution to the problems of the mental hospital building type. A great deal of time and research was necessary be- fore the writer could even begin to bridge this gap, due to professional differences in terminology, outlook, and ap- proach. The next limitation was my personal discomfort when I saw the patients illhoused, with very little in their en- vironment to help them retain their individuality and denied the right to facilities for a complete life because of build- ing deficiencies. The last limitation was that the presen- tation of such a study must necessarily be orderly and cata- logue in an organized way what a mental hospital is and needs. However, no such order is in existence in the actual build- ing, and unfortunately this presentation tends to leave the reader with the concept of order in the mental hospital. -

1973 NGA Annual Meeting
Proceedings OF THE NATIONAL GOVERNORS' CONFERENCE 1973 SIXTY-FIFTH ANNUAL MEETING DEL WEBB'S SAHARA TAHOE. LAKE TAHOE, NEVADA JUNE 3-61973 THE NATIONAL GOVERNORS' CONFERENCE IRON WORKS PIKE LEXINGTON, KENTUCKY 40511 Published by THE NATIONAL GOVERNORS' CONFERENCE IRON WORKS PIKE LEXINGTON, KENTUCKY 40511 CONTENTS Executive Committee Rosters . vi Other Committees of the Conference vii Governors and Guest Speakers in Attendance ix Program of the Annual Meeting . xi Monday Session, June 4 Welcoming Remarks-Governor Mike O'Callaghan 2 Address of the Chairman-Governor Marvin Mandel 2 Adoption of Rules of Procedure 4 "Meet the Governors" . 5 David S. Broder Lawrence E. Spivak Elie Abel James J. Kilpatrick Tuesday Session, June 5 "Developing Energy Policy: State, Regional and National" 46 Remarks of Frank Ikard . 46 Remarks of S. David Freeman 52 Remarks of Governor Tom McCall, Chairman, Western Governors' Conference 58 Remarks of Governor Thomas J. Meskill, Chairman, New England Governors' Conference . 59 Remarks of Governor Robert D. Ray, Chairman, Midwestern Governors' Conference 61 Remarks of Governor Milton J. Shapp, Vice-Chairman, Mid-Atlantic Governors' Conference . 61 Remarks of Governor George C. Wallace, Chairman, Southern Governors' Conference 63 Statement by the Committee on Natural Resources and Environmental Management, presented by Governor Stanley K. Hathaway 65 Discussion by the Governors . 67 "Education Finance: Challenge to the States" 81 Remarks of John E. Coons . 81 Remarks of Governor Wendell R. Anderson 85 Remarks of Governor Tom McCall 87 Remarks of Governor William G. Milliken 88 iii Remarks of Governor Calvin L. Rampton 89 Discussion by the Governors . 91 "New Directions in Welfare and Social Services" 97 Remarks by Frank Carlucci 97 Discussion by the Governors . -

Of 379 Institutons Receiving a Questionnaire on Their Paramedical
DOCUMENT RESUME ED 022 442 JC 680 311 INVENTORY 1967: MASSACHUSETTS HEALTH MANPOWER TRAINING AT LESS THAN A BACCALAUREATE LEVEL. PART I. Training Center for Comprehensive Care, Jamaica Plain, Mass. Pula Date 67 Note-96p. EDRS Price MF-S0.50 HC-$3.92 Descriptors-*HEALTH OCCUPATIONS, *JUNIOR COLLEGES, *MANPOWER DEVELOPMENT, MEDICAL RECORD TECHNICIANS, fvEDICAL SERVICES, NURSES, NURSES AIDES, *PARAMEDICAL OCCUPATIONS, *SUBPROFESSIONALS, THERAPISTS, VOCATIONAL EDUCATION Identifiers *Massachusetts Of 379 institutonsreceiving a questionnaire on their paramedical training programs, 369 replied. They supplied data on 465 courses in 56 job categories. Those conducting the courses include hospitals, nursing homes, highschools, colleges, universities, technical schools, community service agencies, the State Department of Public Health, and an industrial plant. For each job category are given (1) a definition, (2) a detailed description of the curriculum, (3) the teaching staff, (4) a hst of the places offering the course, (5) the cost of the course, (6) in-training payment, if any, for taking the course, (7) length of time required for the course, and (8) ehgibility requirements for the trainee. (HH) U.S.melitillMMIN DEPARIMENTOFFICE OF HEALTH, OF EDUCATION EDUCATION &WELFARE THIS DOCUMENT HAS BEEN REPRODUCEDEXACTLY AS RECEIVED FROM THE PERSONPOSITIONSTATEDMASSACHUSETTS DO OR OR NOT ORGANIZATION POLICY. NECESSARILY ORIGINATING REPRESENT IT.OFFICIALPOINTS OFFICE OF VIEW OF EDUCATION OR OPINIONS ATHEALTH LESS THANMANPOWERAINVENTORY BACCALAUREATETRAITLEVEL ING fteb 1967 Training Center170 Mortonfor Comprehensive Street Care i Jamaica PARTPlain, ONEMass. 02130 1 MASSACHUSETTS IHEALTH N V E N T O RMANPOWER Y 19 6 7 TRAINING 1 AT LESS THAN ACONTENTS BACCALAUREATELEVEL IntroductionSponsorship of the survey Pages1-2 TheMethodDefinition Situation used ofin trainingconducting the survey 3-5 Location.JobNumberrequirements. -
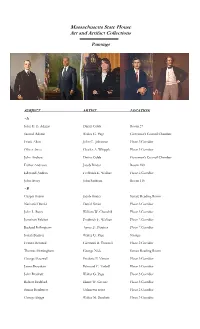
Open PDF File, 134.33 KB, for Paintings
Massachusetts State House Art and Artifact Collections Paintings SUBJECT ARTIST LOCATION ~A John G. B. Adams Darius Cobb Room 27 Samuel Adams Walter G. Page Governor’s Council Chamber Frank Allen John C. Johansen Floor 3 Corridor Oliver Ames Charles A. Whipple Floor 3 Corridor John Andrew Darius Cobb Governor’s Council Chamber Esther Andrews Jacob Binder Room 189 Edmund Andros Frederick E. Wallace Floor 2 Corridor John Avery John Sanborn Room 116 ~B Gaspar Bacon Jacob Binder Senate Reading Room Nathaniel Banks Daniel Strain Floor 3 Corridor John L. Bates William W. Churchill Floor 3 Corridor Jonathan Belcher Frederick E. Wallace Floor 2 Corridor Richard Bellingham Agnes E. Fletcher Floor 2 Corridor Josiah Benton Walter G. Page Storage Francis Bernard Giovanni B. Troccoli Floor 2 Corridor Thomas Birmingham George Nick Senate Reading Room George Boutwell Frederic P. Vinton Floor 3 Corridor James Bowdoin Edmund C. Tarbell Floor 3 Corridor John Brackett Walter G. Page Floor 3 Corridor Robert Bradford Elmer W. Greene Floor 3 Corridor Simon Bradstreet Unknown artist Floor 2 Corridor George Briggs Walter M. Brackett Floor 3 Corridor Massachusetts State House Art Collection: Inventory of Paintings by Subject John Brooks Jacob Wagner Floor 3 Corridor William M. Bulger Warren and Lucia Prosperi Senate Reading Room Alexander Bullock Horace R. Burdick Floor 3 Corridor Anson Burlingame Unknown artist Room 272 William Burnet John Watson Floor 2 Corridor Benjamin F. Butler Walter Gilman Page Floor 3 Corridor ~C Argeo Paul Cellucci Ronald Sherr Lt. Governor’s Office Henry Childs Moses Wight Room 373 William Claflin James Harvey Young Floor 3 Corridor John Clifford Benoni Irwin Floor 3 Corridor David Cobb Edgar Parker Room 222 Charles C. -

EOHHS State-Operated Facility and Congregate Care Site Data
EOHHS State-Operated Facilities Current Positive Current Current Current Total State Positive Patient Facility State Staff Patient Patients Staff Patient Deaths in Cases Census Recovered Cases Last 28 Days Chelsea Soldiers' Home 312 0 226 0 54 0 Corrigan Mental Health Center 64 0 14 0 0 0 Hogan DDS Regional Center 422 0 106 0 61 0 Holyoke Soldiers' Home 324 < 5 103 0 65 0 Lemuel Shattuck Hospital 740 5 184 0 41 0 Pappas Rehabilitation Hospital for Children 221 0 58 0 < 5 0 Pocasset Mental Health Center 80 0 13 0 0 0 Solomon Carter Fuller Mental Health Center 194 0 54 0 6 0 Taunton State Hospital 207 < 5 44 0 < 5 0 Tewksbury Hospital 962 6 325 0 112 0 Western Massachusetts Hospital 295 < 5 68 0 17 0 Women's Recovery from Addictions Program 221 < 5 45 0 0 0 Worcester Recovery Center & Hospital 830 < 5 262 0 20 0 Wrentham DDS Developmental Center 850 < 5 195 0 80 0 Data as of September 7, 2021 Notes: 1. Patient cases and recoveries are for patients included in the current census, they do not include all facility cases and recoveries over time 2. Recovered patients are defined as those who have tested negative or have met symptom and time-based recovery guidelines issued by the MA Department of Public Health and Centers for Disease Control 9/8/2021 Updated: 9/8/2021 Draft for Discussion Purposes Only 1 EOHHS Congregate Care Sites State-Operated Sites Vendor-Operated Sites Current Current Positive Current Current Current Current Total State Positive Current Positive Client Deaths Agency State Staff Client Clients Clients Staff Client Client -

Jaco Three Views of His Secrets
26 bassplayer.com /january2016 Jaco Three Views of his secreTs By e.e. Bradman About hAlf An hour into the new documentary Jaco, there’s a scene that reflects a cru- cial aspect of the Jaco Pastorius legend. It’s the fall of 1975, and Blood, Sweat & Tears drummer Bobby Colomby has flown a virtually unknown Jaco from Ft. Lauderdale to New York to record his debut with jazz luminaries Hubert Laws, Herbie Hancock, Don Alias, Wayne Shorter, and Lenny White. The product of those sessions, the soulful, eclectic stunner simply titled Jaco Pastorius, would shake the bass world to its foundations, of course, but the album cover—with its bold lettering across a no-nonsense black & white portrait by Don Hunstein—might suggest that the unsmiling young maestro was overly serious about making a good first impression. That wasn’t true at all. “It was wild,” says Return To Forever drummer Lenny White of the sessions in October 1975. “Basically, we would play, do a take, and go outside and play basketball.” “We could have done it on bicycles with microphones, and he would have played it perfectly,” remembers producer Colomby, still impressed four decades later. Far from nervous, in fact, 23-year-old Jaco was natural, relaxed, and in his element. “I walked into the studio, and Jaco’s eyes were lit up because he had found home—this was the level he belonged on,” recalls trombonist/musical direc- tor Peter Graves. These quintessential Pastorius hallmarks—soul- ful virtuosity, athletic showmanship, and superhu- man technique, with confidence to burn—are central bassplayer.com / january2016 27 CS JACO JEFF YEAGER Robert Trujillo themes of Jaco.