Update on Future Headache Treatments
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Medication Guide
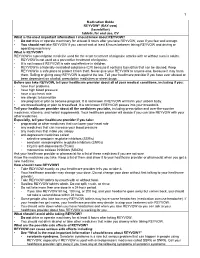
1 Medication Guide REYVOW® (RAY-vow) (lasmiditan) tablets, for oral use, CV What is the most important information I should know about REYVOW? • Do not drive or operate machinery for at least 8 hours after you take REYVOW, even if you feel well enough. • You should not take REYVOW if you cannot wait at least 8 hours between taking REYVOW and driving or operating machinery. What is REYVOW? REYVOW is a prescription medicine used for the acute treatment of migraine attacks with or without aura in adults. • REYVOW is not used as a preventive treatment of migraine. • It is not known if REYVOW is safe and effective in children. • REYVOW is a federally controlled substance (CV) because it contains lasmiditan that can be abused. Keep REYVOW in a safe place to protect it from theft. Never give your REYVOW to anyone else, because it may harm them. Selling or giving away REYVOW is against the law. Tell your healthcare provider if you have ever abused or been dependent on alcohol, prescription medicines or street drugs. Before you take REYVOW, tell your healthcare provider about all of your medical conditions, including if you: • have liver problems • have high blood pressure • have a low heart rate • are allergic to lasmiditan • are pregnant or plan to become pregnant. It is not known if REYVOW will harm your unborn baby. • are breastfeeding or plan to breastfeed. It is not known if REYVOW passes into your breastmilk. Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. -

What Are the Acute Treatments for Migraine and How Are They Used?
2. Acute Treatment CQ II-2-1 What are the acute treatments for migraine and how are they used? Recommendation The mainstay of acute treatment for migraine is pharmacotherapy. The drugs used include (1) acetaminophen, (2) non-steroidal anti-inflammatory drugs (NSAIDs), (3) ergotamines, (4) triptans and (5) antiemetics. Stratified treatment according to the severity of migraine is recommended: use NSAIDs such as aspirin and naproxen for mild to moderate headache, and use triptans for moderate to severe headache, or even mild to moderate headache when NSAIDs were ineffective in the past. It is necessary to give guidance and cautions to patients having acute attacks, and explain the methods of using medications (timing, dose, frequency of use) and medication use during pregnancy and breast-feeding. Grade A Background and Objective The objective of acute treatment is to resolve the migraine attack completely and rapidly and restore the patient’s normal functions. An ideal treatment should have the following characteristics: (1) resolves pain and associated symptoms rapidly; (2) is consistently effective; (3) no recurrence; (4) no need for additional use of medication; (5) no adverse effects; (6) can be administered by the patients themselves; and (7) low cost. Literature was searched to identify acute treatments that satisfy the above conditions. Comments and Evidence The acute treatment drugs for migraine generally include (1) acetaminophens, (2) non-steroidal anti-inflammatory drugs (NSAIDs), (3) ergotamines, (4) triptans, and (5) antiemetics. For severe migraines including status migrainosus and migraine attacks refractory to treatment, (6) anesthetics, and (7) corticosteroids (dexamethasone) are used (Tables 1 and 2).1)-9) There are two approaches to the selection and sequencing of these medications: “step care” and “stratified care”. -

Pharmacokinetics, Pharmacodynamics and Drug
pharmaceutics Review Pharmacokinetics, Pharmacodynamics and Drug–Drug Interactions of New Anti-Migraine Drugs—Lasmiditan, Gepants, and Calcitonin-Gene-Related Peptide (CGRP) Receptor Monoclonal Antibodies Danuta Szkutnik-Fiedler Department of Clinical Pharmacy and Biopharmacy, Pozna´nUniversity of Medical Sciences, Sw.´ Marii Magdaleny 14 St., 61-861 Pozna´n,Poland; [email protected] Received: 28 October 2020; Accepted: 30 November 2020; Published: 3 December 2020 Abstract: In the last few years, there have been significant advances in migraine management and prevention. Lasmiditan, ubrogepant, rimegepant and monoclonal antibodies (erenumab, fremanezumab, galcanezumab, and eptinezumab) are new drugs that were launched on the US pharmaceutical market; some of them also in Europe. This publication reviews the available worldwide references on the safety of these anti-migraine drugs with a focus on the possible drug–drug (DDI) or drug–food interactions. As is known, bioavailability of a drug and, hence, its pharmacological efficacy depend on its pharmacokinetics and pharmacodynamics, which may be altered by drug interactions. This paper discusses the interactions of gepants and lasmiditan with, i.a., serotonergic drugs, CYP3A4 inhibitors, and inducers or breast cancer resistant protein (BCRP) and P-glycoprotein (P-gp) inhibitors. In the case of monoclonal antibodies, the issue of pharmacodynamic interactions related to the modulation of the immune system functions was addressed. It also focuses on the effect of monoclonal antibodies on expression of class Fc gamma receptors (FcγR). Keywords: migraine; lasmiditan; gepants; monoclonal antibodies; drug–drug interactions 1. Introduction Migraine is a chronic neurological disorder characterized by a repetitive, usually unilateral, pulsating headache with attacks typically lasting from 4 to 72 h. -

Potential Mechanisms of Prospective Antimigraine Drugs: a Focus on Vascular (Side) Effects
CORE Metadata, citation and similar papers at core.ac.uk Provided by Elsevier - Publisher Connector Pharmacology & Therapeutics 129 (2011) 332–351 Contents lists available at ScienceDirect Pharmacology & Therapeutics journal homepage: www.elsevier.com/locate/pharmthera Associate Editor: John Fozard Potential mechanisms of prospective antimigraine drugs: A focus on vascular (side) effects Kayi Y. Chan a, Steve Vermeersch b, Jan de Hoon b, Carlos M. Villalón c, Antoinette MaassenVanDenBrink a,⁎ a Division of Vascular Medicine and Pharmacology, Department of Internal Medicine, Erasmus Medical Center, P.O. Box 2040, 3000 CA Rotterdam, The Netherlands b Center for Clinical Pharmacology, University Hospitals Leuven, Campus Gasthuisberg, (K.U. Leuven), Leuven, Belgium c Departamento de Farmacobiología, Cinvestav-Coapa, Czda. de los Tenorios 235, Col. Granjas-Coapa, Deleg. Tlalpan, C.P. 14330, México D.F., Mexico article info abstract Available online 2 December 2010 Currently available drugs for the acute treatment of migraine, i.e. ergot alkaloids and triptans, are cranial vasoconstrictors. Although cranial vasoconstriction is likely to mediate—at least a part of—their therapeutic Keywords: effects, this property also causes vascular side-effects. Indeed, the ergot alkaloids and the triptans have been Antimigraine drugs reported to induce myocardial ischemia and stroke, albeit in extremely rare cases, and are contraindicated in Neuropeptides patients with known cardiovascular risk factors. In view of these limitations, novel antimigraine drugs -

Novel Formulations for Treatment of Migraine
(19) TZZ _T (11) EP 2 756 756 A1 (12) EUROPEAN PATENT APPLICATION (43) Date of publication: (51) Int Cl.: 23.07.2014 Bulletin 2014/30 A01N 43/42 (2006.01) A61K 31/44 (2006.01) (21) Application number: 14165112.5 (22) Date of filing: 24.04.2009 (84) Designated Contracting States: • Turanin, John AT BE BG CH CY CZ DE DK EE ES FI FR GB GR Emeryville, CA California 94608 (US) HR HU IE IS IT LI LT LU LV MC MK MT NL NO PL • Hawley, Roger PT RO SE SI SK TR Emeryville, CA California 94608 (US) • Schuster, Jeffrey, A. (30) Priority: 28.04.2008 US 48463 Bolinas, CA California 94924 (US) (62) Document number(s) of the earlier application(s) in (74) Representative: Duxbury, Stephen et al accordance with Art. 76 EPC: Arnold & Siedsma 09739139.5 / 2 273 880 Pettenkoferstrasse 37 80336 München (DE) (71) Applicant: Zogenix, Inc. Emeryville CA 94608 (US) Remarks: This application was filed on 17-04-2014 as a (72) Inventors: divisional application to the application mentioned • Farr, Stephen J. under INID code 62. Orinda, CA California 94563 (US) (54) Novel formulations for treatment of migraine (57) Systems and methods are described for treating Systems that are self contained, portable, prefilled, and un-met medical needs in migraine and related conditions simple to self administer at the onset of a migraine attack such as cluster headache. Included are treatments that are disclosed, and preferably include a needle-free in- are both rapid onset and long acting, which include sus- jector and a high viscosity formulation, to eliminate such tained release formulations, and combination products, issues as fear of self administration with needles, and Also included are treatments for multiple symptoms of needle stick and cross contamination. -

Lasmiditan Is an Effective Acute Treatment for Migraine: a Phase 3 Randomized Study Bernice Kuca, Stephen D
ARTICLE OPEN ACCESS CLASS OF EVIDENCE Lasmiditan is an effective acute treatment for migraine A phase 3 randomized study Bernice Kuca, BA, MS, Stephen D. Silberstein, MD, Linda Wietecha, BSN, MS, Paul H. Berg, MS, Correspondence Gregory Dozier, MPH, and Richard B. Lipton, MD, on behalf of the COL MIG-301 Study Group Ms. Wietecha [email protected] Neurology® 2018;91:e2222-e2232. doi:10.1212/WNL.0000000000006641 Abstract RELATED ARTICLE Objective Article To assess the efficacy and safety of lasmiditan in the acute treatment of migraine. Galcanezumab in chronic migraine: The randomized, Methods double-blind, placebo- Adult patients with migraine were randomized (1:1:1) to a double-blind dose of oral lasmiditan controlled REGAIN study 200 mg, lasmiditan 100 mg, or placebo and were asked to treat their next migraine attack within Page 1082 4 hours of onset. Over 48 hours after dosing, patients used an electronic diary to record headache pain and the presence of nausea, phonophobia, and photophobia, one of which was MORE ONLINE designated their most bothersome symptom (MBS). Class of Evidence Criteria for rating Results ≥ therapeutic and diagnostic Of the 1,856 patients who treated an attack, 77.9% had 1 cardiovascular risk factors in addition studies to migraine. Compared with placebo, more patients dosed with lasmiditan 200 mg were free of NPub.org/coe headache pain at 2 hours after dosing (32.2% vs 15.3%; odds ratio [OR] 2.6, 95% confidence interval [CI] 2.0–3.6, p< 0.001), similar to those dosed with lasmiditan 100 mg (28.2%; OR 2.2, 95% CI 1.6–3.0, p< 0.001). -

Antimigraine Agents, Triptans Review 07/21/2008
Antimigraine Agents, Triptans Review 07/21/2008 Copyright © 2004 - 2008 by Provider Synergies, L.L.C. All rights reserved. Printed in the United States of America. All rights reserved. No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, digital scanning, or via any information storage and retrieval system without the express written consent of Provider Synergies, L.L.C. All requests for permission should be mailed to: Attention: Copyright Administrator Intellectual Property Department Provider Synergies, L.L.C. 5181 Natorp Blvd., Suite 205 Mason, Ohio 45040 The materials contained herein represent the opinions of the collective authors and editors and should not be construed to be the official representation of any professional organization or group, any state Pharmacy and Therapeutics committee, any state Medicaid Agency, or any other clinical committee. This material is not intended to be relied upon as medical advice for specific medical cases and nothing contained herein should be relied upon by any patient, medical professional or layperson seeking information about a specific course of treatment for a specific medical condition. All readers of this material are responsible for independently obtaining medical advice and guidance from their own physician and/or other medical professional in regard to the best course of treatment for their specific medical condition. This publication, inclusive of all forms contained herein, is intended -

Frovatriptan Versus Zolmitriptan for the Acute Treatment of Migraine: a Double-Blind, Randomized, Multicenter, Italian Study
Neurol Sci (2010) 31 (Suppl 1):S51–S54 DOI 10.1007/s10072-010-0273-x SYMPOSIUM: NEWS IN TREATMENT OF MIGRAINE ATTACK Frovatriptan versus zolmitriptan for the acute treatment of migraine: a double-blind, randomized, multicenter, Italian study Vincenzo Tullo • Gianni Allais • Michel D. Ferrari • Marcella Curone • Eliana Mea • Stefano Omboni • Chiara Benedetto • Dario Zava • Gennaro Bussone Ó The Author(s) 2010. This article is published with open access at Springerlink.com Abstract The objective of this study is to assess patients’ of PF episodes at 2 h was 26% with F and 31% with Z satisfaction with migraine treatment with frovatriptan (F) (p = NS). PR episodes at 2 h were 57% for F and 58% for or zolmitriptan (Z), by preference questionnaire. 133 sub- Z(p = NS). Rate of recurrence was 21 (F) and 24% jects with a history of migraine with or without aura (IHS (Z; p = NS). Time to recurrence within 48 h was better for criteria) were randomized to F 2.5 mg or Z 2.5 mg. The F especially between 4 and 16 h (p \ 0.05). SPF episodes study had a multicenter, randomized, double-blind, cross- were 18 (F) versus 22% (Z; p = NS). Drug-related adverse over design, with each of the two treatment periods lasting events were significantly (p \ 0.05) less under F (3 vs. 10). no more than 3 months. At the end of the study, patients In conclusion, our study suggests that F has a similar were asked to assign preference to one of the treatments efficacy of Z, with some advantage as regards tolerability (primary endpoint). -

Triptans Step Therapy/Quantity Limit Criteria
Triptans Step Therapy/Quantity Limit Criteria Program may be implemented with the following options 1) step therapy 2) quantity limits or 3) step therapy with quantity limits For Blue Cross and Blue Shield of Illinois Option 1 (step therapy only) will apply. Brand Generic Dosage Form Amerge® naratriptan tablets Axert® almotriptan tablets Frova® frovatriptan tablets Imitrex® sumatriptan injection*, nasal spray, tablets* Maxalt® rizatriptan tablets Maxalt-MLT® rizatriptan tablets Relpax® eletriptan tablets Treximet™ sumatriptan and naproxen tablets Zomig® zolmitriptan tablets, nasal spray Zomig-ZMT® zolmitriptan tablets * generic available and included as target agent in quantity limit edit FDA APPROVED INDICATIONS1-7 The following information is taken from individual drug prescribing information and is provided here as background information only. Not all FDA-approved indications may be considered medically necessary. All criteria are found in the section “Prior Authorization Criteria for Approval.” Amerge® Tablets1, Axert® Tablets2, Frova® Tablets3,Imitrex® injection4, Imitrex Nasal Spray5, Imitrex Tablets6, Maxalt® Tablets7, Maxalt-MLT® Tablets7, Relpax® Tablets8, Treximet™ Tablets9, Zomig® Tablets10, Zomig-ZMT® Tablets10, and Zomig® Nasal Spray11 Amerge (naratriptan), Axert (almotriptan), Frova (frovatriptan), Imitrex (sumatriptan), Maxalt (rizatriptan), Maxalt-MLT (rizatriptan orally disintegrating), Relpax (eletriptan), Treximet (sumatriptan/naproxen), Zomig (zolmitriptan), and Zomig-ZMT (zolmitriptan orally disintegrating) tablets, and Imitrex (sumatriptan) and Zomig (zolmitriptan) nasal spray are all indicated for the acute treatment of migraine attacks with or without aura in adults. They are not intended for the prophylactic therapy of migraine or for use in the management of hemiplegic or basilar migraine. Safety and effectiveness of all of these products have not been established for cluster headache, which is present in an older, predominantly male population. -

(12) United States Patent (10) Patent No.: US 6,264,917 B1 Klaveness Et Al
USOO6264,917B1 (12) United States Patent (10) Patent No.: US 6,264,917 B1 Klaveness et al. (45) Date of Patent: Jul. 24, 2001 (54) TARGETED ULTRASOUND CONTRAST 5,733,572 3/1998 Unger et al.. AGENTS 5,780,010 7/1998 Lanza et al. 5,846,517 12/1998 Unger .................................. 424/9.52 (75) Inventors: Jo Klaveness; Pál Rongved; Dagfinn 5,849,727 12/1998 Porter et al. ......................... 514/156 Lovhaug, all of Oslo (NO) 5,910,300 6/1999 Tournier et al. .................... 424/9.34 FOREIGN PATENT DOCUMENTS (73) Assignee: Nycomed Imaging AS, Oslo (NO) 2 145 SOS 4/1994 (CA). (*) Notice: Subject to any disclaimer, the term of this 19 626 530 1/1998 (DE). patent is extended or adjusted under 35 O 727 225 8/1996 (EP). U.S.C. 154(b) by 0 days. WO91/15244 10/1991 (WO). WO 93/20802 10/1993 (WO). WO 94/07539 4/1994 (WO). (21) Appl. No.: 08/958,993 WO 94/28873 12/1994 (WO). WO 94/28874 12/1994 (WO). (22) Filed: Oct. 28, 1997 WO95/03356 2/1995 (WO). WO95/03357 2/1995 (WO). Related U.S. Application Data WO95/07072 3/1995 (WO). (60) Provisional application No. 60/049.264, filed on Jun. 7, WO95/15118 6/1995 (WO). 1997, provisional application No. 60/049,265, filed on Jun. WO 96/39149 12/1996 (WO). 7, 1997, and provisional application No. 60/049.268, filed WO 96/40277 12/1996 (WO). on Jun. 7, 1997. WO 96/40285 12/1996 (WO). (30) Foreign Application Priority Data WO 96/41647 12/1996 (WO). -

Stems for Nonproprietary Drug Names
USAN STEM LIST STEM DEFINITION EXAMPLES -abine (see -arabine, -citabine) -ac anti-inflammatory agents (acetic acid derivatives) bromfenac dexpemedolac -acetam (see -racetam) -adol or analgesics (mixed opiate receptor agonists/ tazadolene -adol- antagonists) spiradolene levonantradol -adox antibacterials (quinoline dioxide derivatives) carbadox -afenone antiarrhythmics (propafenone derivatives) alprafenone diprafenonex -afil PDE5 inhibitors tadalafil -aj- antiarrhythmics (ajmaline derivatives) lorajmine -aldrate antacid aluminum salts magaldrate -algron alpha1 - and alpha2 - adrenoreceptor agonists dabuzalgron -alol combined alpha and beta blockers labetalol medroxalol -amidis antimyloidotics tafamidis -amivir (see -vir) -ampa ionotropic non-NMDA glutamate receptors (AMPA and/or KA receptors) subgroup: -ampanel antagonists becampanel -ampator modulators forampator -anib angiogenesis inhibitors pegaptanib cediranib 1 subgroup: -siranib siRNA bevasiranib -andr- androgens nandrolone -anserin serotonin 5-HT2 receptor antagonists altanserin tropanserin adatanserin -antel anthelmintics (undefined group) carbantel subgroup: -quantel 2-deoxoparaherquamide A derivatives derquantel -antrone antineoplastics; anthraquinone derivatives pixantrone -apsel P-selectin antagonists torapsel -arabine antineoplastics (arabinofuranosyl derivatives) fazarabine fludarabine aril-, -aril, -aril- antiviral (arildone derivatives) pleconaril arildone fosarilate -arit antirheumatics (lobenzarit type) lobenzarit clobuzarit -arol anticoagulants (dicumarol type) dicumarol -

Zomig and Zomig Rapimelt Are Trade Marks of the Astrazeneca Group of Companies
AUSTRALIAN PRODUCT INFORMATION Zomig® and Zomig Rapimelt® (zolmitriptan) 1 NAME OF THE MEDICINE Zolmitriptan 2 QUALITATIVE AND QUANTITATIVE COMPOSITION Zomig is presented as round, yellow (2.5 mg) or pink (5 mg), biconvex film-coated intagliated (with a ‘Z’ on one side) tablets containing 2.5 mg or 5 mg zolmitriptan. The 2.5 mg tablets are 7.4 mm in diameter and are compressed to a weight of 122 mg. The 5 mg tablets are 8.6 mm in diameter and are compressed to a weight of 244 mg. Zomig Rapimelt is presented as orally dispersible white round uncoated orange flavoured tablets containing 2.5 mg zolmitriptan. The tablets are 6.4 mm in diameter, flat-faced with a bevelled edge and intagliated with ‘Z’ on one side. The tablets are compressed to a weight of 100 mg. Excipient(s) with known effect: lactose monohydrate (Zomig), aspartame (Zomig Rapimelt). For the full list of excipients, see Section 6.1 List of excipients. 3 PHARMACEUTICAL FORM • Tablet, film-coated • Tablet, dispersible (oral) 4 CLINICAL PARTICULARS 4.1 THERAPEUTIC INDICATIONS Zomig is indicated for the acute treatment of migraine with or without aura. 4.2 DOSE AND METHOD OF ADMINISTRATION The recommended initial dose of Zomig to treat a migraine attack is 2.5 mg. The Zomig conventional tablet should be swallowed whole with water. The Zomig Rapimelt orally dispersible tablet rapidly dissolves when placed on the tongue and is swallowed with the patient’s saliva. A drink of water is not required when taking the Zomig Rapimelt orally dispersible tablet.