Measuring Muscle and Fat with Peripheral Quantitative Computed Tomography
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Requirements James Miyor to Hit a 3-Pointer to Broken Their Five-Game and the Carrier Dome
; 9m '^wrw,' 4fi M' Pag» 24 • THE VILLANOVAN • JwHMry 30, 1$07 Sports I S Wildcats terminate losing streak Vol. 62, Na IS VILLANOVA UNIVER8fTY, VILLANOVA, PA**^» w^ f FetmiaryS, 1987 By STEPHEN J. SCHLAGER stripe. Rony Seikaly hit two from back and forth at each other and Seton Hall's Mark Bryant com- Wilson ended the scoring by ^ the line followed by an eight-foot the first half ended with Villanova mitted his fifth persona] foul and hitting both ends of a one-and-one. The Villanova Wildcat basket- jumper by Coleman to tie the ball up by nine, 42-33. sent Massey to the line. Massey The final score read Villanova 86, ball team ventured on a road trip game at 40. West scored first in second half missed the one-and-one, allowing Seton Hall 82. The WUdcaU had last week to Syracuse University The score was tied again at 42, making two charity points and a finally Requirements James Miyor to hit a 3-pointer to broken their five-game and the Carrier Dome. Villanova 48 and then at 50 before Syracuse 16-foot jumper off a feed from bring the score to a diff-hanging losing streak. came out and put the squeeze on took the lead for good off a Sher- Wilson. By the time the first the Orangemen. man Douglas jumper from 18 feet television timeout rolled along the Villanova controlled the tap and with 3:28 left in the game. Wildcats were still up by nine, 50- and Doug West slammed home the Syracuse took complete control 41. -

J. Frank Wilson
J. FRANK WILSON J. Frank was born December 11, 1941 in Lufkin, TX. In 1962 J. Frank Wilson, After Being Discharged From Goodfellow Air Force Base, Auditioned For The San Angelo Based Group "The Cavaliers" (Sid Holmes-Lewis Elliott-Bob Zeller-Ray Smith). J. Frank Would Then Be Discovered By Independent Record Producer Sonley Roush Who Had Booked The Band At The Blue Note Club (3rd and Birdwell St) In Big Spring, Texas In 1962. After Signing A 3 Year Manager's Contract With Sid Holmes, In 1963, Frank Took A Leave Of Absents. In 1964 J. Frank Was Re-Instated As The Lead Singer For The Cavaliers Replacing John Maberry. The Cavaliers, J. Frank Wilson, Buddy Croyle, Lewis Elliott, Roland Atkinson, Jim Wynne And A Girl Who Sang In Church (unknown) Went About The Business Of Copying Wayne Cochran's Record In Ron Newdoll's Studio In San Angelo. With J. Frank In Top Form The Record (First Released On Tamara 761 & Le Cam 722) On Josie Started Moving Up The Billboard Charts. It Wasn't Long After This That Contract Disputes, Law Suits, And Greedy Un- Scrupulous Promoters Began Taking Their Toll. After Touring With The Dick Clark Caravan Of Stars The Cavaliers Quit On The Road Returning Back To San Angelo. A Short Time Later Sonley Roush (Road Mgr.) Died In A Car Crash While Touring With J. Frank, Murry Kellum (Long Tall Texan), Travis Wammack (Scratchy), Jerry Graham (Bass), Phil Trunzo (Drums) And Buddy Croyle (Guitar/Sax). The Song, Last Kiss, Had Been Based On An Actual Event That Took The Lives Of 3 Teens In Georgia. -

The Righteous Brothers by Jerry Bfay At
The Righteous Brothers B yJerry Bfayat •— —■ a d i o , w i t h o u t a d o u b t , is t h e m o s t i m p o r - and “Leaving It All lip to You,” which years later tant vehicle for a recording artist. How became a Number One hit for Dale & Grace. Two- many times did y o u turn on your radio part harmony was not unique then - but a pair of and hear a great song b y a great a r t i s t s ! white boys emulating the great black two-part-har Rmaybe Johnny Otis singing “Willie and thm e Hand on y sound? That w as new. Jive,” the Magnificent Men doing “Peace of Mind,” or For Bobby Hatfield and Bill M edley (bom a m onth the Soul Survivors performing “Expressway (To Your apart in 1940), it began separately. Both started Heart)” - not realizing these were white performers, singing at Orange County, California, clubs as ones who had the soul and the ability to sound teenagers. In the early 1960s, Bobby had his group, black? Conversely, did you ever lis the Variations, and Bill his, the ten to an artist like Ella Fitzgerald, Paramours. In 1962, Bobby’s group Carmen McRae or Nancy Wilson incorporated with the Paramours. and say to yourself, “Wow, what a One of their first big shows together fantastic performer,” and assume was at the Rendezvous Ballroom, in she was white? That’s the wonder Balboa, California, a famous haunt ful thing about music: The great during the big-band era. -

Descendants of John Hugh Wilson
Descendants of John Hugh Wilson by Mary H. Ash Descendants of John Hugh Wilson Descendants of John Hugh Wilson Generation No. 1 1. JOHN HUGH1 WILSON was born 1689 in Londonderry, Ireland, and died July 09, 1773 in Letterkenny Twp, Cumberland, PA. Notes for JOHN HUGH WILSON: From "Scotch-Irish Pioneers in Ulster and America" Early settlers of Londonderry comprised many who remained but a short time and moved on to new plantations. In July and August, 1718, from five to seven hundred Protestant immigrants from Ireland entered the Port of Boston. Several followers of the Rev. Mr. McGregor set out early in autumn for Andover where they spent the winter. In 1719 there were seventy families at Nutfield, Mass. though not all of Scotch-Irish connection. Wilsons that were on this list included BENJAMIN WILLSON, ELIZABETH WILLSON, MARY WILLSON, THOMAS WILLSON, WILLIAM WILLSON, JAMES WILSON and ROBERT WILSON. The immigrants were given a 10 mile square tract of land for a town of their own. A list of proprietors of Londonderry in 1722 records about 100 Schotch-Irish land owners. Frank Shepherd in WILSON-BAIRD HISTORY states this John is John Hugh Wilson, and born about 1675 in Scotland. The following account is from OUR WILSONS, GASTONS, AND HUTTONS, Herman Wilson Craven, Washington D.C. 1926 The first Wilson of our family of whom we have positive information was one of the defenders of Londonderry, northern Ireland, in 1689. According to uncertain tradition as it came down to Martha Wilson, her sister Lucinda, and her brother Joseph, his name was John. -

Motown Pop and Southern Soul
UNIT 7 (P. 222-235) CHAPTER 6: MOTOWN POP AND SOUTHERN SOUL Intro Until early 60’s, many African-Americans blocks from mainstream success by white covers o Majority of African-American recording artists signed to independent labels, and recordings’ popularity could be easily eclipsed by major label versions British invasion bands took much of early inspiration from African-American popular music By 1965, situation in youth-music market had significantly improved for black artists wanting mainstream hits Among most important developments was music that came from Motown Records (independent company; most important era of success parallels that of the Beatles) and the emergence of southern soul from Memphis American rock press that emerged in mid-60’s often cast Motown as black pop music that made too many concessions to white sensibilities – selling out its “blackness” to make money in white market; while southern soul portrayed as music that makes no excuses for its blackness, staying closer to origins in black culture o Perception of racial authenticity after music accepted into white mainstream o Crossover so prevalent; December ’63 – January ’65, Billboard stopped tracking R&B charts separately Berry Gordy, Jr. and Black Music for White Audiences Go Where the Money Is: White Kids and Disposable Income Berry Gordy, Jr.: professional boxer in Detroit area, worked for father’s construction company, owned a record store, and worked on Ford assembly line; spent a lot of time in Detroit’s jazz clubs – jazz = not key to success in music -

May 2010 OPTIMIZED.Indd
Cool Issue 190 The Publication of the Linn County Blues Society - lcbs.org May 2010 O E D O E T O E COO TIME Free! Kids activities LIBERTY CENTRE Hot food BLUES & BBQ 2 7 6 2 - 6 0 4 2 5 Cold beer A I , s apid R r a d Ce Cool music 2 7 6 2 x o B O P SUNDAY, MAY 30 y t e oci S s e u l B y t n u o C n n i L Noon-10 p.m. Liberty Centre Park North Liberty BBQ’Loo & Blues Too Featuring: Corner of E. 4th & Mulberry Streets Dennis “Daddy-O” McMurrin Lincoln Park in downtown Waterloo & the Demolition Band Craig Erickson BBQ C Bob Dorr & The Blue Band Kids no test! Rib-EA ctivities! a ting Kevin “B.F.” Burt & the Instigatorg s C o n test! northlibertyiowa.org/bluesandbbq FREE EVENT! In this May 2010 issue — Friday, July 16 Saturday, July 17 Hot Hand Blues Band at Parlor City Pub 1st Annual Irish District Music/Arts Festival Bluesmore 2010 5:30-9:30PM 5:30PM - 9:30PM Big Mo’s CD review is in the bag! Avey Brothers Mark Selby Diplomats of Solid Sound still performing Plan to be there. Flock Of Funk rocks New Bohemia district at Parlor City Pub Other activities include a KCBS Sanctioned Local LIVE music schedules barbeque contest, kids activities, chili contest, rib-eating contest and some of the best BBQ around. Blues at CSPS McMurrin & Johnson bring Blues to the schools Main Street Waterloo is proud to support the LCBS ©2010 May-Linn County Blues Society The Linn County Blues Society is a way Hot Hand Blues Band cool, non-profi t organization dedicated Blues at CSPS to the preservation of Blues music in A very cool show at Parlor City Pub Eastern Iowa as well as to provide The Holmes Brothers May 5 • Carrie Rodriguez May 12 charitable contributions to other commu- photos and story by Bill Ray nity organizations. -
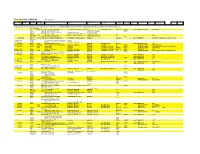
Motown Tape Index
Four Seasons at Motown 1971 to 1974 highlight indicates songs released Session/Mix Location Reel Nr MasterNr Title Writers Producer Arranger listing as Stereo Mix Release Record Nr Time Comment Date (16 track) (45rel/Other) (personnel) (2 track)reel Date (Eu notation) Original master references for 45 released tracks taken from: Off The Records - Motown By Master Number 1959-1989 - by Reginald J. Bartlette, PC Ink, MI, 1991-verified with Tape index In Reel Nr order ? 60516-7B Walk On, Don't Look Back The Corporation (with The 4Seasons) Corp &Gene Page FV&TFS P4496? Aug-72 Mo-West 5026FA 2:56 23/08/72 P2060 60692 My Heart Cries Out To You J. Marcellino - M.Larson T2043 P2079 60662 What Love Has Joined Together S.Robinson-B.Rogers Cleveland - Payton P2079 60665 Save The Children M.Gaye - A.Cleveland - R.Benson Cleveland - Payton P2082(M) 60693 Baby I Need Your Loving Holland - Dozier - Holland J. Marcellino - M.Larson FV 3:04 P2082(M) 60692 My Heart Cries Out To You J. Marcellino - M.Larson T2043 08/02/72 LA P2093 60597-S-034BJust Look What You Have Done Frank Wilson - R. Dean-Taylor Hal Davis 4Seasons Nov-74 MW-PR10 4:47 10/75 - Promo only - double "A" side (24 Track) Nov/Dec 1971 P2105 Oh Girl Everything Is Gonna Be Alright B.Moss Nov/Dec 1971 P2105 What It Is N.Whitfield – B.Strong 01/02/72 P2105 60758 When The Morning Comes B.Gaudio Dave Blumberg FV&TFS May-72 Mo-West 106LP 4:37 Nov/Dec 1971 P2105 60744-4A Love Isn't Here (Like It Used To Be) B.Gaudio - B.Gaudio B.Gaudio C.Calello FV P4333 Mo-West 5011FB 4:09 03/01/1972 01/02/72 P2105 60759 Sun Country B.Gaudio B.Gaudio C.Calello - Joe Scott FS P4336 Mo-West 5025FB 4:05 07/08/72 - Promo test pressing only 60759 Sun Country B.Gaudio B.Gaudio C.Calello - Joe Scott FV&TFS P4336 Mo-West 5026FB 4:05 23/08/72 Nov/Dec 1971 P2105 Touch The Rainchild B.Gaudio - A. -

Download This Issue As A
Columbia College Fall 2013 TODAY MAKING A DIFFERENCE Sheena Wright ’90, ’94L Breaks Ground as First Woman CEO of United Way of New York City NETWORK WITH COLUMBIA ALUMNI BILL CAMPBELL, CHAIRMAN OF THE BOARD OF TRUSTEES, COLUMBIA UNIVERSITY CHAIRMAN OF THE BOARD OF DIRECTORS, INTUIT MEMBER OF THE BOARD OF DIRECTORS, APPLE MEMBER OF THE COLUMBIA UNIVERSITY CLUB OF NEW YORK The perfect midtown location to network, dine with a client, hold events or business meetings, house guests in town for the weekend, and much more. To become a member, visit columbiaclub.org or call 212-719-0380. in residence at The Princeton Club of New York 15 WEST 43 STREET NEW YORK, NY 10036 Columbia Ad_famous alumni.indd 6 11/8/12 12:48 PM Contents FEATURES 14 Trail Blazer 20 Loyal to His Core Sheena Wright ’90, ’94L is breaking As a Columbia teacher, scholar and ground as the first female CEO of alumnus, Wm. Theodore de Bary ’41, ’53 United Way of New York City. GSAS has long exemplified the highest BY YELENA SHUSTER ’09 standards of character and service. BY JAMIE KATZ ’72, ’80 BUSINEss 26 New Orleans’ Music Man 34 Passport to India After 25 years in NOLA, Scott Aiges ’86 Students intern in Mumbai, among is dedicated to preserving and other global sites, via Columbia promoting its musical traditions. Experience Overseas. BY ALEXIS TONTI ’11 ARTS BY SHIRA BOss ’93, ’97J, ’98 SIPA Front cover: After participating in a United Way of New York City read-aloud program at the Mott Haven Public Library in the Bronx, Sheena Wright ’90, ’94L takes time out to visit a community garden in the neighborhood. -

The Temptations Wish It Would Rain & in a Mellow
The Temptations Wish It Would Rain & In A Mellow Mood mp3, flac, wma DOWNLOAD LINKS (Clickable) Genre: Funk / Soul Album: Wish It Would Rain & In A Mellow Mood Country: UK & Europe Released: 2000 Style: Soul MP3 version RAR size: 1301 mb FLAC version RAR size: 1297 mb WMA version RAR size: 1293 mb Rating: 4.3 Votes: 412 Other Formats: APE MP4 DTS ASF MMF WAV MP1 Tracklist Hide Credits Wish It Would Rain I Could Never Love Another 1 Producer – Norman WhitfieldWritten-By – Barrett Strong, Norman Whitfield, Roger Penzabene Cindy 2 Written-By, Producer – William "Smokey" Robinson* I Wish It Would Rain 3 Producer – Norman WhitfieldWritten-By – Barrett Strong, Norman Whitfield, Roger Penzabene Plese Return Your Love To Me 4 Producer – Norman WhitfieldWritten-By – Barbara Neely, Barrett Strong, Norman Whitfield Fan The Flame 5 Written-By, Producer – William "Smokey" Robinson* He Who Picks A Rose 6 Producer – Norman WhitfieldWritten By – SmileyWritten-By – Holland*, Whitfield* Why Did You Leave Me Darling 7 Written-By – Dean*, Lussier* I Truly, Truly Believe 8 Producer – Henry CosbyWritten-By – Allen Story, George Gordy, Margaret Gordy This Is My Beloved 9 Written-By – Nickolas Ashford/Valerie Simpson* Gonna Give Her All The Love I've Got 10 Producer – Norman WhitfieldWritten-By – Barrett Strong, Norman Whitfield I've Passed This Way Before 11 Written-By – Dean*, Witherspoon* No Man Can Love Her Like I Do 12 Producer – Norman WhitfieldWritten-By – Eddie Kendricks, Edward Holland Jr.*, Norman Whitfield In A Mellow Mood Hello, Young Lovers 13 Producer -

National Register of Historic Places Registration Form NOV 2 O Ip
Untttd States Department of the Interior National Park Service .- F C. fr 1 \/ ',r. National Register of Historic Places NOV 2 o ip SEP 3 0 I992i Registration Form NATIONAL REGISTER OHP Thla form to for uaa In nominating or requeetlng datarmlnatlona of eligibility for Individual propartiaa or dietrtcts. Saa Inetructton* in tor CompfcMng rVettona/ ftaofefar forma (National Register Bulletin 16). Complata aach Ham by marking "»" in tha appropriate box or by antahng tha raquaatad Information. H an rtam doaa not apply to tha proparly baing doeumantad, antar "N/A" for "not applicable." For functtone, atytee, matartalt, and areas of aignlficanca, antar onry tha catagorlaa and aubcatagoriaa liatad in tha Instructions. For additional apaoa uaa oomlnuatlon ahaatt (Form I0»800a). Typa all entries 1. Name of Property ""* hlatorlc nama Qlovne Court Hr>i-el othar names/sits number Cloyne Court 2, Location atn>et & number 2600 Ridae Road Nl^ not for publication Olft , town Berkeley jJT_ vicinity ftata coda CA oounty Alameda ood llDOOdt Claaalflcatlon Ownarahlp of Proparly Category of Proparty Numbar of Raaourota within Proparty prlvata bulldlng(a) Contributing Nonoontrlbutlng public-local district ^ bulldlngi publlc-Stata •Ita attai public-Federal atruoiura _ alructura i _ objact ,objacti .Total Nama of ralatad multlpla proptrty Hating: Numbtr of contributing raaourcaa pravlouily liatad In tha National Raglatar _. Q___ 4. Btata/Fadaril Agancy Cartlflcatlon Aa the designated authority under the National Hiatoric Preservation Act of 1066, as amended, I hereby certify that this Ol nomination CD requeat for determination of eligibility meats tha documentation atandarda for registering properties In the National Register of HiejSric Places and meets the procedural and professional requirements aet forth In 36 CFR Part 60. -

History of Ole Miss Football
HISTORY & RECORDS HISTORY OF OLE MISS FOOTBALL The University of Mississippi boasts a long and col- orful football history, which includes the formation of the first football team in the state, as well as one of the most successful programs in the history of collegiate football. In its 120-year history, the Ole Miss football pro- gram has claimed three national championships (1959, 1960 and 1962), six Southeastern Conference titles (1947, 1954, 1955, 1960, 1962, and 1963), and one SEC Western Division title (2003). In addition, Ole Miss has produced 54 first-team All-America selections and 162 First Team All-SEC selections, appeared in 34 bowl games with 22 wins, and sent almost 300 players into the professional ranks. REBEL FOOTBALL BEGINNINGS The beginnings of the program can be traced all the way back to 1890 when Dr. A.L. Bondurant, who would later serve as Dean of the Graduate School, urged Ole Miss students to help in the formation of an Athletic Association in the interests of football, baseball and ten- First Ole Miss All-American Bruiser Kinard (Left) nis. Such a group became a reality a short while later, and Kinard, in 1936. Kinard, who also earned All-America things to come for Ole Miss. During his 24-year tenure, in 1893, a football team was organized, with Bondurant first-team honors in 1937, would be the first of 46 Reb- the Rebels would have only one losing campaign. serving as the manager-coach. els to earn the prestigious national accolade. Vaught’s squads, however, didn’t stop at just That first squad set a precedent that was to be- Under Walker’s tenure, Ole Miss took another step winning league titles. -

The Cavaliers (1956-1964)
THE CAVALIERS (1956-1964) Although a stepping-stone to fame, for some, The Cavaliers were basically a weekend band from it's beginning to the present. The 45 record "Last Kiss" Josie 923 did reach #1 on The Cashbox Singles Charts, #1 Music World, #1 American Bandstand, and #2 on The Billboard Singles Charts in 1964 and then later released on compilation CD Collectables The History Of Rock The 60's, One Hit Wonders Of The 60's, Dick Bartley's Rock & Roll Oldies Show, Time-Life 60's Hits, The Best Of Tragedy, Billboard Top Rock' N' Roll Hits and Senior Prom 50 Great Golden Oldies. The "Last Kiss" LP reached #29 on The Cashbox Album Charts and #51 on The Billboard Album Charts in 1964. The 45 record follow-up "Hey, Little One" Josie 926 reached #85 on The Billboard Singles Charts in 1964. The 45 record "Last Kiss" released on Virgo 506 reached #80 in Cashbox and #90 in Billboard in 1973. The 45 record "Crazy Guitar" Jane 107, recorded in 1956, was distributed nationally by Jay-Gee Records in New York City in 1959 and in Europe on compilation Knoxville LP "Rock & Roll" Vol 2 in 1975, compilation White Label LP 8924 "Rock Moon Rock" in 1980 with "I've Decided" released on Cat CD 1035 "Calling All Rock N' Roll Collectors" Vol 3 in 1994. The Last Kiss Sessions CD from 1964 was released in 1998 on Collectables 0712. Books and magazines with related stories or references to The Cavaliers include: The Billboard Book of One Hit Wonders by Wayne Jancik, The 2002 revised addition of Who's Who Of West Texas Rock N' Roll Music by Bill Griggs, Song Hits Magazine April Edition 1965, The Billboard Book of Top 40 Hits 1955-2000 by Joel Whitburn, Roy Orbison Life & Legacy by Alan Clayson, Texas Music Magazine 2001, The Texas Monthly Magazine February 1992, The New Yorker Magazine August 1999, Time Magazine 1999, Movie Life Yearbook 1964, Music World (J.