Protease Activity As a Prognostic Factor for Wound Healing in Venous Leg Ulcers (Protocol)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Microbial Enzymes and Their Applications in Industries and Medicine
BioMed Research International Microbial Enzymes and Their Applications in Industries and Medicine Guest Editors: Periasamy Anbu, Subash C. B. Gopinath, Arzu Coleri Cihan, and Bidur Prasad Chaulagain Microbial Enzymes and Their Applications in Industries and Medicine BioMed Research International Microbial Enzymes and Their Applications in Industries and Medicine Guest Editors: Periasamy Anbu, Subash C. B. Gopinath, Arzu Coleri Cihan, and Bidur Prasad Chaulagain Copyright © 2013 Hindawi Publishing Corporation. All rights reserved. This is a special issue published in “BioMed Research International.” All articles are open access articles distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Contents Microbial Enzymes and Their Applications in Industries and Medicine,PeriasamyAnbu, Subash C. B. Gopinath, Arzu Coleri Cihan, and Bidur Prasad Chaulagain Volume 2013, Article ID 204014, 2 pages Effect of C/N Ratio and Media Optimization through Response Surface Methodology on Simultaneous Productions of Intra- and Extracellular Inulinase and Invertase from Aspergillus niger ATCC 20611, Mojdeh Dinarvand, Malahat Rezaee, Malihe Masomian, Seyed Davoud Jazayeri, Mohsen Zareian, Sahar Abbasi, and Arbakariya B. Ariff Volume 2013, Article ID 508968, 13 pages A Broader View: Microbial Enzymes and Their Relevance in Industries, Medicine, and Beyond, Neelam Gurung, Sumanta Ray, Sutapa Bose, and Vivek Rai Volume 2013, Article -
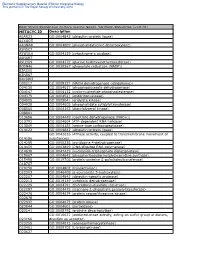
METACYC ID Description A0AR23 GO:0004842 (Ubiquitin-Protein Ligase
Electronic Supplementary Material (ESI) for Integrative Biology This journal is © The Royal Society of Chemistry 2012 Heat Stress Responsive Zostera marina Genes, Southern Population (α=0. -

Amyloid-Degrading Ability of Nattokinase from Bacillus Subtilis Natto
J. Agric. Food Chem. 2009, 57, 503–508 503 Amyloid-Degrading Ability of Nattokinase from Bacillus subtilis Natto †,‡ § § † RUEI-LIN HSU, KUNG-TA LEE, JUNG-HAO WANG, LILY Y.-L. LEE, AND ,†,‡ RITA P.-Y. CHEN* Institute of Biological Chemistry, Academia Sinica, Taipei 115, Taiwan, R. O. C., Institute of Biochemical Sciences, National Taiwan University, Taipei 106, Taiwan, R. O. C., and Department of Biochemical Science and Technology, National Taiwan University, Taipei 106, Taiwan, R. O. C. More than 20 unrelated proteins can form amyloid fibrils in vivo which are related to various diseases, such as Alzheimer’s disease, prion disease, and systematic amyloidosis. Amyloid fibrils are an ordered protein aggregate with a lamellar cross- structure. Enhancing amyloid clearance is one of the targets of the therapy of these amyloid-related diseases. Although there is debate on whether the toxicity is due to amyloids or their precursors, research on the degradation of amyloids may help prevent or alleviate these diseases. In this study, we explored the amyloid-degrading ability of nattokinase, a fibrinolytic subtilisin-like serine protease, and determined the optimal conditions for amyloid hydrolysis. This ability is shared by proteinase K and subtilisin Carlsberg, but not by trypsin or plasmin. KEYWORDS: Nattokinase; amyloid; natto; subtilisin NAT; amyloid degradation; fibril; amyloidosis INTRODUCTION of cardiovascular disease. Dietary supplementation with natto Natto, a fermented food made from boiled soybeans, has suppresses the intimal thickening of arteries and leads to the been eaten for more than 1000 years in Asia. The fermenta- lysis of mural thrombi seen after endothelial injury (12). tion microbe isolated from natto is the Gram-positive Other clinically thrombolytic agents, such as urokinase and endospore-forming bacterium Bacillus subtilis natto (formerly streptokinase, are costly and unstable in the intestinal tract designated Bacillus natto)(1). -

Identification and Phylogenetic Analysis of Keratinase Producing Bacteria SNP1 from Poultry Field
International Journal of Biotechnology and Biochemistry ISSN 0973-2691 Volume 15, Number 1 (2019) pp. 39-51 © Research India Publications http://www.ripublication.com Identification and Phylogenetic Analysis of Keratinase Producing Bacteria SNP1 from Poultry Field Divya Balakrishnan and Nithadas Sathyadas Padmanabhan Department of Biotechnology, Sree Narayana College, Kollam-691001, Kerala, India. (*Corresponding author) Abstract The study was conduct to select the best promising keratinolytic bacterial strain. A keratinase positive bacterial strain was isolated from the soil samples of poultry field, Attingal, Thiruvananthapuram. Each sample was plated on skim milk agar and feather meal agar plates containing 5 g feather. The well grown isolates which produced the largest clear zone on skimmed milk plate were selected for keratinase assays. Out of 26 bacterial isolates, 7 isolates were selected. Among the selected strain, the best keratinase producing bacterium SNP1was selected for further analysis. The SNP1 potential strain was later confirmed as Bacillus haynessi based on molecular and phylogenetic analysis. The medium components and culture conditions were optimized to enhance keratinase production through optimization. Keratin and feather powder (10g/l) were identified as good substrates for the highest keratinase production. The strain SNP1 resulted maximum enzyme production at 96h of incubation at 37°C and pH 8 under 120 rpm. Therefore, Bacillus hayneisi might be used for large scale production of keratinase for industrial purposes. Keywords: Keratinase, Bacillus sp., Optimization, Enzyme activity, 16SrRNA Keratin is a hard-degrading fibrous and recalcitrant structural protein, which forms the third most abundant polymer in nature after cellulose and chitin (Lene et al ., 2016). In the native state, the feather keratin resists the degradation by proteolytic enzymes such as trypsin and pepsin due to tightpeptide-chains held together by disulfide bridges by means of cysteine residues (Weeranut, 2017; Korniłłowicz-Kowalska and Bohacz, 2011). -

(12) United States Patent (10) Patent No.: US 6,395,889 B1 Robison (45) Date of Patent: May 28, 2002
USOO6395889B1 (12) United States Patent (10) Patent No.: US 6,395,889 B1 Robison (45) Date of Patent: May 28, 2002 (54) NUCLEIC ACID MOLECULES ENCODING WO WO-98/56804 A1 * 12/1998 ........... CO7H/21/02 HUMAN PROTEASE HOMOLOGS WO WO-99/0785.0 A1 * 2/1999 ... C12N/15/12 WO WO-99/37660 A1 * 7/1999 ........... CO7H/21/04 (75) Inventor: fish E. Robison, Wilmington, MA OTHER PUBLICATIONS Vazquez, F., et al., 1999, “METH-1, a human ortholog of (73) Assignee: Millennium Pharmaceuticals, Inc., ADAMTS-1, and METH-2 are members of a new family of Cambridge, MA (US) proteins with angio-inhibitory activity', The Journal of c: - 0 Biological Chemistry, vol. 274, No. 33, pp. 23349–23357.* (*) Notice: Subject to any disclaimer, the term of this Descriptors of Protease Classes in Prosite and Pfam Data patent is extended or adjusted under 35 bases. U.S.C. 154(b) by 0 days. * cited by examiner (21) Appl. No.: 09/392, 184 Primary Examiner Ponnathapu Achutamurthy (22) Filed: Sep. 9, 1999 ASSistant Examiner William W. Moore (51) Int. Cl." C12N 15/57; C12N 15/12; (74) Attorney, Agent, or Firm-Alston & Bird LLP C12N 9/64; C12N 15/79 (57) ABSTRACT (52) U.S. Cl. .................... 536/23.2; 536/23.5; 435/69.1; 435/252.3; 435/320.1 The invention relates to polynucleotides encoding newly (58) Field of Search ............................... 536,232,235. identified protease homologs. The invention also relates to 435/6, 226, 69.1, 252.3 the proteases. The invention further relates to methods using s s s/ - - -us the protease polypeptides and polynucleotides as a target for (56) References Cited diagnosis and treatment in protease-mediated disorders. -

Cross-Linking of Alpha 2-Plasmin Inhibitor to Fibrin by Fibrin- Stabilizing Factor
Cross-linking of alpha 2-plasmin inhibitor to fibrin by fibrin- stabilizing factor. Y Sakata, N Aoki J Clin Invest. 1980;65(2):290-297. https://doi.org/10.1172/JCI109671. Research Article The concentration of alpha 2-plasmin inhibitor in blood plasma is higher than that in serum obtained from the blood clotted in the presence of calcium ions, but is the same as that in serum obtained in the absence of calcium ions. Radiolabeled alpha2-plasmin inhibitor was covalently bound to fibrin only when calcium ions were present at the time of clotting of plasma or fibrinogen. Whereas, when batroxobin, a snake venom enzyme that lacks the ability to activate fibrin- stabilizing factor, was used for clotting fibrinogen, the binding was not observed. When fibrin-stablizing, factor-deficient plasma was clotted, the specific binding of alpha 2-plasmin inhibitor to fibrin did not occur even in the presence of calcium ions and the concentration of alpha 2-plasmin inhibitor in serum was the same as that in plasma. Monodansyl cadaverine, a fluorescent substrate of the fibrin-stablizing factor, was incorporated into alpha 2-plasmin inhibitor by activated fibrin-stablizing factor. All these findings indicate that alpha 2-plasmin inhibitor is cross-linked to fibrin by activated fibrin-stabilizing factor when blood is clotted. Analysis of alpha 2-plasmin inhibitor-incorporated fibrin by sodium dodecyl sulfate gel electrophoresis showed that the inhibitor was mainly cross-linked to polymerized alpha-chains of cross-linked fibrin. Cross-linking of alpha 2-plasmin inhibitor to fibrin renders fibrin clot less susceptible to fibrinolysis by plasmin. -

Application of Plant Proteolytic Enzymes for Tenderization of Rabbit Meat
Biotechnology in Animal Husbandry 34 (2), p 229-238 , 2018 ISSN 1450-9156 Publisher: Institute for Animal Husbandry, Belgrade-Zemun UDC 637.5.039'637.55'712 https://doi.org/10.2298/BAH1802229D APPLICATION OF PLANT PROTEOLYTIC ENZYMES FOR TENDERIZATION OF RABBIT MEAT Maria Doneva, Iliana Nacheva, Svetla Dyankova, Petya Metodieva, Daniela Miteva Institute of Cryobiology and Food Technology, Cherni Vrah 53, 1407, Sofia, Bulgaria Corresponding author: Maria Doneva, e-mail: [email protected] Original scientific paper Abstract: The purpose of this study is to assess the tenderizing effect of plant proteolytic enzymes upon raw rabbit meat. Tests are performed on rabbit meat samples treated with papain and two vegetal sources of natural proteases (extracts of kiwifruit and ginger root). Two variants of marinade solutions are prepared from each vegetable raw materials– 50% (w/w) and 100 % (w/w), with a duration of processing 2h, 24h, and 48h. Changes in the following physico- chemical characteristics of meat have been observed: pH, water-holding capacity, cooking losses and quantity of free amino acids. Differences in values of these characteristics have been observed, both between control and test samples, as well as depending of treatment duration. For meat samples marinated with papain and ginger extracts, the water-holding capacity reached to 6.74 ± 0.04 % (papain), 5.58 ± 0.09 % (variant 1) and 6.80 ± 0.11 % (variant 2) after 48 hours treatment. In rabbit meat marinated with kiwifruit extracts, a significant increase in WHC was observed at 48 hours, 3.37 ± 0.07 (variant 3) and 6.84 ± 0.11 (variant 4). -

Insulysin Hydrolyzes Amyloid Β Peptides to Products That Are Neither Neurotoxic Nor Deposit on Amyloid Plaques
The Journal of Neuroscience, December 1, 2000, 20(23):8745–8749 Insulysin Hydrolyzes Amyloid  Peptides to Products That Are Neither Neurotoxic Nor Deposit on Amyloid Plaques Atish Mukherjee,1 Eun-suk Song,1 Muthoni Kihiko-Ehmann,2 Jack P. Goodman Jr,3 Jan St. Pyrek,3 Steven Estus,2 and Louis B. Hersh1 1Department of Biochemistry, 2Department of Physiology and Sanders-Brown Center on Aging, and 3Mass Spectrometry Facility, University of Kentucky, Lexington, Kentucky 40536-0298   Insulysin (EC. 3.4.22.11) has been implicated in the clearance of action of insulysin on A 1–40 and A 1–42 was shown to eliminate  amyloid peptides through hydrolytic cleavage. To further study the neurotoxic effects of these peptides. Insulysin was further   the action of insulysin on A peptides recombinant rat insulysin shown to prevent the deposition of A 1–40 onto a synthetic   was used. Cleavage of both A 1–40 and A 1–42 by the recombi- amyloid. Taken together these results suggest that the use of nant enzyme was shown to initially occur at the His 13-His 14, insulysin to hydrolyze A peptides represents an alternative gene His 14-Gln 15, and Phe 19-Phe 20 bonds. This was followed by a therapeutic approach to the treatment of Alzheimer’s disease. slower cleavage at the Lys 28-Gly 29,Val18-Phe 19, and Phe 20- Ala 21 positions. None of the products appeared to be further Key words: amyloid peptide metabolism; metallopeptidase; metabolized by insulysin. Using a rat cortical cell system, the insulysin; A neurotoxicity; A deposition; A cleavage The major pathological feature of Alzheimer’s disease is the pres- Kurochkin and Goto (1994) showed that another zinc metal- ence of senile plaques in the brain of affected individuals. -

B1–Proteases As Molecular Targets of Drug Development
Abstracts B1–Proteases as Molecular Targets of Drug Development B1-001 lin release from the beta cells. Furthermore, GLP-1 also stimu- DPP-IV structure and inhibitor design lates beta cell growth and insulin biosynthesis, inhibits glucagon H. B. Rasmussen1, S. Branner1, N. Wagtmann3, J. R. Bjelke1 and secretion, reduces free fatty acids and delays gastric emptying. A. B. Kanstrup2 GLP-1 has therefore been suggested as a potentially new treat- 1Protein Engineering, Novo Nordisk A/S, Bagsvaerd, Denmark, ment for type 2 diabetes. However, GLP-1 is very rapidly degra- 2Medicinal Chemistry, Novo Nordisk A/S, Maaloev, Denmark, ded in the bloodstream by the enzyme dipeptidyl peptidase IV 3Discovery Biology, Novo Nordisk A/S, Maaloev, DENMARK. (DPP-IV; EC 3.4.14.5). A very promising approach to harvest E-mail: [email protected] the beneficial effect of GLP-1 in the treatment of diabetes is to inhibit the DPP-IV enzyme, thereby enhancing the levels of The incretin hormones GLP-1 and GIP are released from the gut endogenously intact circulating GLP-1. The three dimensional during meals, and serve as enhancers of glucose stimulated insu- structure of human DPP-IV in complex with various inhibitors 138 Abstracts creates a better understanding of the specificity and selectivity of drug-like transition-state inhibitors but can be utilized for the this enzyme and allows for further exploration and design of new design of non-transition-state inhibitors that compete for sub- therapeutic inhibitors. The majority of the currently known DPP- strate binding. Besides carrying out proteolytic activity, the IV inhibitors consist of an alpha amino acid pyrrolidine core, to ectodomain of memapsin 2 also interacts with APP leading to which substituents have been added to optimize affinity, potency, the endocytosis of both proteins into the endosomes where APP enzyme selectivity, oral bioavailability, and duration of action. -

Serine Proteases with Altered Sensitivity to Activity-Modulating
(19) & (11) EP 2 045 321 A2 (12) EUROPEAN PATENT APPLICATION (43) Date of publication: (51) Int Cl.: 08.04.2009 Bulletin 2009/15 C12N 9/00 (2006.01) C12N 15/00 (2006.01) C12Q 1/37 (2006.01) (21) Application number: 09150549.5 (22) Date of filing: 26.05.2006 (84) Designated Contracting States: • Haupts, Ulrich AT BE BG CH CY CZ DE DK EE ES FI FR GB GR 51519 Odenthal (DE) HU IE IS IT LI LT LU LV MC NL PL PT RO SE SI • Coco, Wayne SK TR 50737 Köln (DE) •Tebbe, Jan (30) Priority: 27.05.2005 EP 05104543 50733 Köln (DE) • Votsmeier, Christian (62) Document number(s) of the earlier application(s) in 50259 Pulheim (DE) accordance with Art. 76 EPC: • Scheidig, Andreas 06763303.2 / 1 883 696 50823 Köln (DE) (71) Applicant: Direvo Biotech AG (74) Representative: von Kreisler Selting Werner 50829 Köln (DE) Patentanwälte P.O. Box 10 22 41 (72) Inventors: 50462 Köln (DE) • Koltermann, André 82057 Icking (DE) Remarks: • Kettling, Ulrich This application was filed on 14-01-2009 as a 81477 München (DE) divisional application to the application mentioned under INID code 62. (54) Serine proteases with altered sensitivity to activity-modulating substances (57) The present invention provides variants of ser- screening of the library in the presence of one or several ine proteases of the S1 class with altered sensitivity to activity-modulating substances, selection of variants with one or more activity-modulating substances. A method altered sensitivity to one or several activity-modulating for the generation of such proteases is disclosed, com- substances and isolation of those polynucleotide se- prising the provision of a protease library encoding poly- quences that encode for the selected variants. -

R&D Assay for Alzheimer's Disease
R&DR&D assayassay forfor Alzheimer’sAlzheimer’s diseasedisease Target screening⳼ Ⲽ㬔 antibody array, ᢜ⭉㬔 ⸽ἐⴐ Amyloid β-peptide Alzheimer’s disease⯸ ኸᷠ᧔ ᆹ⸽ inhibitor, antibody, ELISA kit Surwhrph#Surilohu#Dqwlerg|#Duud| 6OUSFBUFE 1."5SFBUFE )41 $3&# &3, &3, )41 $3&# &3, &3, 壤伡庰䋸TBNQMF ɅH 侴䋸嵄䍴䋸BOBMZUFT䋸䬱娴哜塵 1$ 1$ 1$ 1$ 5IFNPTUSFGFSFODFEBSSBZT 1$ 1$ QQ α 34, .4, 503 Q α 34, .4, 503 %SVHTDSFFOJOH0òUBSHFUFòFDUT0ATHWAY涭廐 6OUSFBUFE 堄币䋸4BNQMF侴䋸8FTUFSOPS&-*4"䍘䧽 1."5SFBUFE P 8FTUFSOCMPU廽喜儤应侴䋸0, Z 4VCTUSBUF -JHIU )31DPOKVHBUFE1BO "OUJQIPTQIPUZSPTJOF .FBO1JYFM%FOTJUZ Y $BQUVSF"OUJCPEZ 5BSHFU"OBMZUF "SSBZ.FNCSBOF $3&# &3, &3, )41 .4, Q α 34, 503 Human XL Cytokine Array kit (ARY022, 102 analytes) Adiponectin,Aggrecan,Angiogenin,Angiopoietin-1,Angiopoietin-2,BAFF,BDNF,Complement,Component C5/C5a,CD14,CD30,CD40L, Chitinase 3-like 1,Complement Factor D,C-Reactive Protein,Cripto-1,Cystatin C,Dkk-1,DPPIV,EGF,EMMPRIN,ENA-78,Endoglin, Fas L,FGF basic,FGF- 7,FGF-19,Flt-3 L,G-CSF,GDF-15,GM-CSF,GRO-α,Grow th Hormone,HGF,ICAM-1,IFN-γ,IGFBP-2,IGFBP-3, IL-1α,IL-1β, IL-1ra,IL-2,IL-3,IL-4,IL- 5,IL-6,IL-8, IL-10,IL-11,IL-12, IL-13,IL-15,IL-16,IL-17A,IL-18 BPa,IL-19,IL-22, IL-23,IL-24,IL-27, IL-31,IL-32α/β/γ,IL-33,IL-34,IP-10,I-TAC,Kallikrein 3,Leptin,LIF,Lipocalin-2,MCP-1,MCP-3,M-CSF,MIF,MIG,MIP-1α/MIP-1β,MIP-3α,MIP-3β,MMP-9, Myeloperoxidase,Osteopontin, p70, PDGF-AA, PDGF-AB/BB,Pentraxin-3, PF4, RAGE, RANTES,RBP4,Relaxin-2, Resistin,SDF-1α,Serpin E1, SHBG, ST2, TARC,TFF3,TfR,TGF- ,Thrombospondin-1,TNF-α, uPAR, VEGF, Vitamin D BP Human Protease (34 analytes) / -

Current IUBMB Recommendations on Enzyme Nomenclature and Kinetics$
Perspectives in Science (2014) 1,74–87 Available online at www.sciencedirect.com www.elsevier.com/locate/pisc REVIEW Current IUBMB recommendations on enzyme nomenclature and kinetics$ Athel Cornish-Bowden CNRS-BIP, 31 chemin Joseph-Aiguier, B.P. 71, 13402 Marseille Cedex 20, France Received 9 July 2013; accepted 6 November 2013; Available online 27 March 2014 KEYWORDS Abstract Enzyme kinetics; The International Union of Biochemistry (IUB, now IUBMB) prepared recommendations for Rate of reaction; describing the kinetic behaviour of enzymes in 1981. Despite the more than 30 years that have Enzyme passed since these have not subsequently been revised, though in various respects they do not nomenclature; adequately cover current needs. The IUBMB is also responsible for recommendations on the Enzyme classification naming and classification of enzymes. In contrast to the case of kinetics, these recommenda- tions are kept continuously up to date. & 2014 The Author. Published by Elsevier GmbH. This is an open access article under the CC BY license (http://creativecommons.org/licenses/by/3.0/). Contents Introduction...................................................................75 Kinetics introduction...........................................................75 Introduction to enzyme nomenclature ................................................76 Basic definitions ................................................................76 Rates of consumption and formation .................................................76 Rate of reaction .............................................................76