The Magazine for Alumni and Friends
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Crime, Law Enforcement, and Punishment
Shirley Papers 48 Research Materials, Crime Series Inventory Box Folder Folder Title Research Materials Crime, Law Enforcement, and Punishment Capital Punishment 152 1 Newspaper clippings, 1951-1988 2 Newspaper clippings, 1891-1938 3 Newspaper clippings, 1990-1993 4 Newspaper clippings, 1994 5 Newspaper clippings, 1995 6 Newspaper clippings, 1996 7 Newspaper clippings, 1997 153 1 Newspaper clippings, 1998 2 Newspaper clippings, 1999 3 Newspaper clippings, 2000 4 Newspaper clippings, 2001-2002 Crime Cases Arizona 154 1 Cochise County 2 Coconino County 3 Gila County 4 Graham County 5-7 Maricopa County 8 Mohave County 9 Navajo County 10 Pima County 11 Pinal County 12 Santa Cruz County 13 Yavapai County 14 Yuma County Arkansas 155 1 Arkansas County 2 Ashley County 3 Baxter County 4 Benton County 5 Boone County 6 Calhoun County 7 Carroll County 8 Clark County 9 Clay County 10 Cleveland County 11 Columbia County 12 Conway County 13 Craighead County 14 Crawford County 15 Crittendon County 16 Cross County 17 Dallas County 18 Faulkner County 19 Franklin County Shirley Papers 49 Research Materials, Crime Series Inventory Box Folder Folder Title 20 Fulton County 21 Garland County 22 Grant County 23 Greene County 24 Hot Springs County 25 Howard County 26 Independence County 27 Izard County 28 Jackson County 29 Jefferson County 30 Johnson County 31 Lafayette County 32 Lincoln County 33 Little River County 34 Logan County 35 Lonoke County 36 Madison County 37 Marion County 156 1 Miller County 2 Mississippi County 3 Monroe County 4 Montgomery County -

A National Strategy for the Elimination of Hepatitis B and C: Phase Two Report
THE NATIONAL ACADEMIES PRESS This PDF is available at http://www.nap.edu/24731 SHARE A National Strategy for the Elimination of Hepatitis B and C: Phase Two Report DETAILS 296 pages | 6 x 9 | PAPERBACK ISBN 978-0-309-45729-3 | DOI: 10.17226/24731 CONTRIBUTORS GET THIS BOOK Gillian J. Buckley and Brian L. Strom, Editors; Committee on a National Strategy for the Elimination of Hepatitis B and C; Board on Population Health and Public Health Practice; Health and Medicine FIND RELATED TITLES Division; National Academies of Sciences, Engineering, and Medicine Visit the National Academies Press at NAP.edu and login or register to get: – Access to free PDF downloads of thousands of scientific reports – 10% off the price of print titles – Email or social media notifications of new titles related to your interests – Special offers and discounts Distribution, posting, or copying of this PDF is strictly prohibited without written permission of the National Academies Press. (Request Permission) Unless otherwise indicated, all materials in this PDF are copyrighted by the National Academy of Sciences. Copyright © National Academy of Sciences. All rights reserved. A National Strategy for the Elimination of Hepatitis B and C: Phase Two Report Gillian J. Buckley and Brian L. Strom, Editors Committee on a National Strategy for the Elimination of Hepatitis B and C Board on Population Health and Public Health Practice Health and Medicine Division A Report of Copyright © National Academy of Sciences. All rights reserved. A National Strategy for the Elimination of Hepatitis B and C: Phase Two Report THE NATIONAL ACADEMIES PRESS 500 Fifth Street, NW Washington, DC 20001 This activity was supported by the American Association for the Study of Liver Diseases, the Infectious Diseases Society of America, the National Viral Hepatitis Roundtable, and the U.S. -

JEREMY E. WULFF Department of Chemistry, University of Victoria
CURRICULUM VITAE (Abbreviated) JEREMY E. WULFF Department of Chemistry, University of Victoria 1. EDUCATION and TRAINING a. Degrees Held degree institution year obtained PhD University of Calgary 2004 BSc (Hons., Co-op) University of Victoria 1999 b. Postdoctoral Experience NSERC Postdoctoral fellow, Harvard University 2005-2007 2. SELECTED POSITIONS HELD PRIOR to APPOINTMENT at UVic period company, job title, duties 1999 : 01-06 Methylgene, research assistant, synthetic organic methodology 1998 : 05-08 Dept. of National Defense, analytical chemist, ICP-MS analysis 1997 : 05-08 Merck Frosst Canada, research assistant, natural product total synthesis 3. ACADEMIC APPOINTMENTS period rank academic unit 07/2007-06/2013 Assistant Professor (renewed 2009) UVic Chemistry 07/2013- Associate Professor with Tenure UVic Chemistry 4. SIGNIFICANT ADMINISTRATIVE or LEADERSHIP ROLES period role 2013- Director, Chemistry for the Medical Sciences BSc Program 2015- Director, CAMTEC Facility for Biomolecular Sample Preparation 5. HONOURS and AWARDS 5a. Recent Awards (since Appointment at UVic): 2012-2022: Canada Research Chair (Tier II) in Bioactive Small Molecule Synthesis [Renewed in 2017] 2011-2019: Michael Smith Foundation for Health Research Career Scholar Award [Renewed in 2016] 2014: Thieme Chemistry Journal Award Top-20-Under-40 on Vancouver Island [Only academic awarded since the re-launch of the program] 2015: Selected for a Synform Young Career Focus Article th [7 researcher worldwide selected for summary] 5b. Earlier Fellowships and Awards: NSERC PDF, John Kendall Thesis Award, I.W. Killam Memorial Scholarship, AHFMR Studentship, NSERC PGSA and PGS-B, Don Tavares Teaching Excellence Award. page 1 of 9 CURRICULUM VITAE (Abbreviated) 6. MAJOR FIELD(S) of SCHOLARLY or PROFESSIONAL INTEREST Organic synthesis, medicinal chemistry, chemical biology, synthetic polymers 7. -

Download 2016
L’ORÉAL-UNESCO FOR WOMEN IN SCIENCE 2016 INTERNATIONAL AWARDS WOMEN IN SCIENCE have the power to change the world The L’Oréal-UNESCO For Women in Science programme was founded in 1998 with a simple aim; to ensure that women are fairly represented at all levels in science. We face unprecedented challenges in our world; climate change, sustainable energy, affordable healthcare, security among other issues. Part of the solutions will come from science and science needs women. Those recognized by the L’Oréal-UNESCO programme have already proved how transformative their science can be in addressing these challenges. Science is indeed part of the future, and it needs every talented mind available, be they men or women. The L’Oréal-UNESCO For Women in Science programme aims to ensure that research in every field takes full advantage of the intelligence, creativity and passion of one-half of the population of the planet. The world needs science, science needs women because women in science have the power to change the world. Isabel Marey Semper General Manager L’Oréal Foundation WOMEN IN SCIENCE have the power to change the world Gender equality is a global priority for UNESCO. In general, the situation for women and girls in terms of access to education, especially higher education, career progression and participation in decision making processes, remains a matter of concern. As ‘UNESCO Science Report: towards 2030’ shows, the disparity is particularly evident in the natural sciences where the number of women participating in science still lags behind in many areas like the physical sciences and engineering. -

UMBC Alumnae Racing to Develop Coronavirus Vaccine
Newsletter SPRING 2020 To our UMBC/Meyerhoff families: We hope you and your families are all doing well during this strange and stressful time of Covid- 19. Although the world has changed quickly with so many things shut down and many of us sheltering at home, we hope this newsletter will represent a ray of sunshine during a dark and difficult time. Please enjoy this positive representation of our student and alumni community. MPA Board UMBC Alumnae Racing to Develop Coronavirus Vaccine Kizzmekia Corbett ’08, M16, biological sciences, says it feels like she’s “living in a constant adrenaline rush.” Maybe that’s because she and her team at the Vaccine Research Center at the National Insti- tute of Allergy and Infectious Diseases have been working around the clock for weeks. They’re racing to develop a vaccine for the coronavirus faster than it can race across the globe. “To be living in this moment where I have the opportunity to work on something that has imminent global importance…it’s just a surre- al moment for me,” Corbett says. Despite it feeling surreal, the advances Corbett and her team are making are very real, and they’re setting records. “We are making better progress than I could have ever hoped for,” she says. After three months of studies in test tubes and in animals, the vaccine her team developed is about to enter a phase I clinical trial, a crucial hur- dle on the way to FDA approval. Read the complete article about Kizzmekia and her team’s efforts to develop a Covid-19 vaccine in the latest UMBC magazine at https:// Kizzmekia Corbett, NIH magazine.umbc.edu/umbc-alumnae-racing-to-develop- coronavirus-vaccine/. -
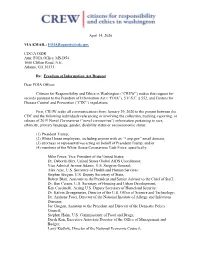
[email protected] CDC/ATSDR Attn
April 14, 2020 VIA EMAIL: [email protected] CDC/ATSDR Attn: FOIA Office, MS-D54 1600 Clifton Road, N.E. Atlanta, GA 30333 Re: Freedom of Information Act Request Dear FOIA Officer: Citizens for Responsibility and Ethics in Washington (“CREW”) makes this request for records pursuant to the Freedom of Information Act (“FOIA”), 5 U.S.C. § 552, and Centers for Disease Control and Prevention (“CDC”) regulations. First, CREW seeks all communications from January 29, 2020 to the present between the CDC and the following individuals referencing or involving the collection, tracking, reporting, or release of 2019 Novel Coronavirus (“novel coronavirus”) information pertaining to race, ethnicity, primary language, gender, disability status or socioeconomic status: (1) President Trump; (2) White House employees, including anyone with an “*.eop.gov” email domain; (3) attorneys or representatives acting on behalf of President Trump; and/or (4) members of the White House Coronavirus Task Force, specifically: Mike Pence, Vice President of the United States; Dr. Deborah Birx, United States Global AIDS Coordinator; Vice Admiral Jerome Adams, U.S. Surgeon General; Alex Azar, U.S. Secretary of Health and Human Services; Stephen Biegun, U.S. Deputy Secretary of State; Robert Blair, Assistant to the President and Senior Advisor to the Chief of Staff; Dr. Ben Carson, U.S. Secretary of Housing and Urban Development; Ken Cuccinelli, Acting U.S. Deputy Secretary of Homeland Security; Dr. Kelvin Droegemeier, Director of the U.S. Office of Science and Technology; Dr. Anthony Fauci, Director of the National Institute of Allergy and Infectious Diseases; Joe Grogan, Assistant to the President and Director of the Domestic Policy Council; Stephen Hahn, U.S. -

White House Briefing Call Notes 7.8.2020
Office of Intergovernmental Affairs State, Local, and Tribal Leaders – Thank you to the State, local, and Tribal leaders who joined for the White House COVID-19 National Briefing Call on Wednesday, July 8. Attendees heard comprehensive updates and insights on continuing support for State, local, and Tribal response, recovery, and reopening efforts from Larry Kudlow (Assistant to the President for Economic Policy), Secretary Robert Wilkie (U.S. Department of Veterans Affairs), Ambassador Deborah Birx (White House Coronavirus Task Force Coordinator), U.S. Surgeon General Gerome Adams, Deputy Surgeon General Erica Schwartz, and Assistant Secretary Frank Brogan (U.S. Department of Education). Below, please find pertinent announcements from across the Federal family and a brief recap of yesterday's call, including information and guidance from the White House Summit on Reopening America’s Schools. We would also like to flag CDC’s online testing resource page where you can find up-to-date testing information. Recent Announcements Paycheck Protection Program (PPP) Extended Through August: On July 4, President Trump signed legislation (S. 4116) reauthorizing the Paycheck Protection Program through August 8, 2020. Enacted in March as part of the CARES Act, the $669 billion program has approved more than 4.8 million loans totaling more than $520 billion and supporting over 51 million jobs to date. The extension of the program through August will make available the remaining $134 billion to small businesses and qualifying entities. Learn more about the PPP here. Department of the Treasury’s OIG released reporting requirements for CRF recipients: On July 2, Department of the Treasury’s Office of Inspector General (OIG) released a memorandum with instructions for recipients of the CARES Act’s Coronavirus Relief Fund (CRF). -

Sleepy Times
DEPARTMENT OF ANESTHESIA AND PERIOPERATIVE MEDICINE SLEEPY TIMES VOLUME 15, ISSUE 4 MAY 2020 Message from the Chairman: Surgeon General, Dr. Jerome Adams, This is our Pearl Harbor. -Scott T. Reeves, MD, MBA I had originally written this opening statement shortly after the Surgeon Inside This Issue: General’s visit to MUSC and months prior to the COVID 19 pandemic. Dr. Jerome Adams is frequently seen standing close to the President Message from Chairman 1-2 during his daily news updates. He is probably most remembered now for Department Champions 3-6 his statement, this is our Pearl Harbor. He was a strong advocate of social distancing prior to all the states coming on board. As you read the Patient Thank You 7 materials below, consider how thoughtful his priorities of Health and Research Corner 8 National Security and Community Health and Economic Prosperity are in light of the recent COVID 19 pandemic. Heart Walk 9 Dr. Jerome Adams is the 20th Surgeon General of the United States. He recently visited Faculty Council 10-11 MUSC and had several initiatives that made an impact personally on me. To start off, it Physician of the Month 11 is incredible that Dr. Adams is an anesthesiologist. Prior to his tenure as surgeon general he was the Health Commissioner of Indiana. As physicians and healthcare advocates, it Covid 19 Serological 12 is imperative that we have not only good intentions but a clear strategy on how to get our Testing message heard and policy implemented. Dr. Adams’ strategy is demonstrating the link Grand Rounds 13 between a community’s and hence persons health and the economic prosperity and I Hung the Moon 14 national security from a community, city, state and country. -

Uniformed Services University Board of Regents
Uniformed Services University of the Health Sciences “Learning to Care for Those in Harm’s Way” Board of Regents Quarterly Meeting November 5, 2019 BOARD OF REGENTS UNIFORMED SERVICES UNIVERSITY OF THE HEALTH SCIENCES 208th MEETING November 5, 2019 | 8:00 a.m. Alvarez Board of Regents Room (D-3001) | Bethesda, MD MEETING AGENDA OPEN MEETING 8:00 a.m.: Meeting Call to Order Designated Federal Officer Ms. Sarah Marshall 8:00 - 8:05 a.m.: Opening Comments Chair, USU Board of Regent Dr. Jonathan Woodson 8:05 - 8:10 a.m.: Matters of General Consent Declaration of Board Actions Dr. Woodson 8:10 - 8:20 a.m.: Board Actions Degree Conferrals, Hébert School of Medicine (SOM) Dean, SOM Dr. Arthur Kellermann Degree Conferrals, Inouye Graduate School of Nursing (GSN) Dean, GSN Dr. Carol Romano Degree Conferrals, College of Allied Health Sciences (CAHS) Dean, CAHS Dr. Mitchell Seal Faculty Appointments and Promotions, SOM Dean, SOM Dr. Kellermann Faculty Appointments and Promotions, PDC Executive Dean, PDC Dr. Schneid Faculty Awards, SOM Dean, SOM Dr. Kellermann 8:20 - 8:45 a.m.: Office of the President, Uniformed Services University of the Health Sciences (USU) Report President, USU Dr. Richard Thomas 8:45 - 9:25 a.m.: Member Reports Academics Summary Board Member Dr. Michael Johns Dr. Johns will provide the Board with a summary of reports from the University Registrar; the Office of Accreditation and Organizational Assessment; and the Faculty Senate. Finance and Administration Summary Board Member Dr. Leo Rouse Dr. Rouse will provide the Board with a summary of reports from the Office of the Vice President for Finance and Administration; the Office of the Vice President for Information and Education Technology; the Office of General Counsel; and the Henry M. -
The Enablers Barbara Kellerman Index More Information © in T
Cambridge University Press 978-1-108-83832-0 — The Enablers Barbara Kellerman Index More Information Index Access Hollywood tape, 89 Atlas, Scott, 237–238 Adams, Jerome, 136, 154, 239–240 authoritarianism Adelson, Sheldon, 47 of base supporters of Trump, 24–25 administration of Donald Trump democracy and, 266–267 Alex Azar, 186–188 soft dictatorship and, 270–271 demographics, 57 of Trump, 24–25, 266–267 dysfunctionality of, 57–58 Azar, Alex, 186–188 early signs of crowd size lies, 55 Bacow, Lawrence, 146–147 inaugural address, 54–55 bad leadership/followership categories family involvement, 56 ineffective, 15 Hope Hicks, 207–208 unethical, 15 H. R. McMaster, 60–61 Bannon, Steve, 73 James Mattis, 61–62 Barr, William, 181–186 John Kelly, 61 Barrack, Tom, 72–73 Kellyanne Conway, 207–208 base supporters of Trump loyalty tests, 64–67 COVID-19 and, 32 Mark Meadows, 196–199 deference to authoritarianism, 24–25 media savviness importance, 57 defined, 22 Mick Mulvaney, 195–196 demographics, 22–23, 33 Mike Pence, 171–176 devotion of, 19–21, 31–33 Mike Pompeo, 176–179 and economic disenfranchisement, military appointees, 56 24 Peter Navarro, 199–201 ethnicity of, 22–23 Rex Tillerson, 59–60 polling of, 265–266 Robert O’Brien, 201–202 relationship to truth, 33–34 Sonny Perdue, 271 types of, 21–22 Steven Mnuchin, 179–181 Bethrothed, The,94 subordinate subservience, 67–70 birtherism, 160 turnover, 61–64 Birx, Deborah, 121, 145, 197–198, wealth of, 56 242–246 William Barr, 181–186 Black Death, 96–98 advisors. See senior advisors, Trump Black Lives Matter, -

2021 Gruber Genetics Prize Recognizes Hematologist- Oncologist and Geneticist Stuart H
Media Contact: A. Sarah Hreha +1 (203) 432‐6231 [email protected] Online Newsroom: https://gruber.yale.edu/news‐media Hematologist-Oncologist Stuart Orkin Receives $500,000 Gruber Genetics Prize for His Groundbreaking Research on the Genetics of Inherited Blood Disorders Stuart H. Orkin March 2, 2021, New Haven, CT – The 2021 Gruber Genetics Prize recognizes hematologist‐ oncologist and geneticist Stuart H. Orkin, M.D., for his pioneering discoveries of the genetic underpinnings of blood disorders. His remarkable body of work has not only revolutionized our understanding of how these illnesses occur but has also led to promising new gene‐based therapies for thalassemia and sickle cell disease, two inherited blood disorders that affect millions of people around the world. Dr. Orkin is the David G. Nathan Distinguished Professor of Pediatrics at Harvard Medical School and the Dana‐Farber/Boston Children’s Cancer and Blood Disorders Center, and an Investigator of the Howard Hughes Medical Institute. The prize, which includes a $500,000 award, will be presented to Orkin at the annual meeting of the American Society of Human Genetics in October. “Dr. Orkin has led the field of hematology for more than 40 years,” says Eric Olson, professor at UT Southwestern and member of the Selection Advisory Board. “His work has been deeply mechanistic, groundbreaking and impactful. Through a series of seminal discoveries, he has helped to unravel key molecular mysteries behind how blood cells develop—and how inherited blood disorders occur.” Early in his career, Orkin identified many genetic mutations behind the various types of thalassemia, an inherited blood disorder characterized by inadequate production of the protein beta‐globin, one of two chains of hemoglobin, the oxygen‐carrying component of red cells. -

Return of Organization Exempt from Income
l efile GRAPHIC p rint - DO NOT PROCESS As Filed Data - DLN: 93493315014869 Return of Organization Exempt From Income Tax O M B No 1545-0047 Form 990 Under section 501 ( c), 527, or 4947 ( a)(1) of the Internal Revenue Code (except black lung benefit trust or private foundation) 2008_ Department of the Open -The organization may have to use a copy of this return to satisfy state reporting requirements Treasury Inspection Internal Revenue Service A For the 2008 calendar year, or tax year beginning 01-01-2008 and ending 12-31-2008 C Name of organization D Employer identification number B Check if applicable Please KAISER FOUNDATION HEALTH PLAN INC FAddress change use IRS 94-1340523 label or Doing Business As E Telephone number F Name change print or type . See (510 ) 271-6611 1 Initial return Specific N um b er and st reet (or P 0 box if mai l is not d e l ivered to st ree t a dd ress ) R oom/suite Instruc - ONE KAISER PLAZA SUITE 15L G Gross receipts $ 53 , 477 , 053 , 641 F_ Termination tions. (-Amended return City or town, state or country, and ZIP + 4 OAKLAND, CA 94612 F_ Application pending F Name and address of Principal Officer H(a) Is this a group return for GEORGE C HALVORSON affiliates ? F-Yes FNo ONE KAISER PLAZA SUITE 15L OAKLAND, CA 94612 H(b) Are all affiliates included ? F Yes F No I Tax - exempt status F 501( c) ( 3) 1 (insert no ) (- 4947(a)(1) or F_ 527 (If "No," attach a list See instructions 3 Web site : - N/A H(c) GroupExemptionNumber - K Type of organization F Corporation 1 trust F association F other I I L Year of Formation 1955 1 M State of legal domicile CA Summar y 1 Briefly describe the organization's mission or most significant activities TO PROVIDE HIGH-QUALITY, AFFORDABLE HEALTH CARE SERVICES TO IMPROVE THE HEALTH OF OUR MEMBERS AND W THE COMMUNITIES WE SERVE 2 Check this box F- if the organization discontinued its operations or disposed of more than 25% of its assets 3 Number ofvoting members of the governing body (Part VI, line 1a) .