Sleepy Times
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A National Strategy for the Elimination of Hepatitis B and C: Phase Two Report
THE NATIONAL ACADEMIES PRESS This PDF is available at http://www.nap.edu/24731 SHARE A National Strategy for the Elimination of Hepatitis B and C: Phase Two Report DETAILS 296 pages | 6 x 9 | PAPERBACK ISBN 978-0-309-45729-3 | DOI: 10.17226/24731 CONTRIBUTORS GET THIS BOOK Gillian J. Buckley and Brian L. Strom, Editors; Committee on a National Strategy for the Elimination of Hepatitis B and C; Board on Population Health and Public Health Practice; Health and Medicine FIND RELATED TITLES Division; National Academies of Sciences, Engineering, and Medicine Visit the National Academies Press at NAP.edu and login or register to get: – Access to free PDF downloads of thousands of scientific reports – 10% off the price of print titles – Email or social media notifications of new titles related to your interests – Special offers and discounts Distribution, posting, or copying of this PDF is strictly prohibited without written permission of the National Academies Press. (Request Permission) Unless otherwise indicated, all materials in this PDF are copyrighted by the National Academy of Sciences. Copyright © National Academy of Sciences. All rights reserved. A National Strategy for the Elimination of Hepatitis B and C: Phase Two Report Gillian J. Buckley and Brian L. Strom, Editors Committee on a National Strategy for the Elimination of Hepatitis B and C Board on Population Health and Public Health Practice Health and Medicine Division A Report of Copyright © National Academy of Sciences. All rights reserved. A National Strategy for the Elimination of Hepatitis B and C: Phase Two Report THE NATIONAL ACADEMIES PRESS 500 Fifth Street, NW Washington, DC 20001 This activity was supported by the American Association for the Study of Liver Diseases, the Infectious Diseases Society of America, the National Viral Hepatitis Roundtable, and the U.S. -

UMBC Alumnae Racing to Develop Coronavirus Vaccine
Newsletter SPRING 2020 To our UMBC/Meyerhoff families: We hope you and your families are all doing well during this strange and stressful time of Covid- 19. Although the world has changed quickly with so many things shut down and many of us sheltering at home, we hope this newsletter will represent a ray of sunshine during a dark and difficult time. Please enjoy this positive representation of our student and alumni community. MPA Board UMBC Alumnae Racing to Develop Coronavirus Vaccine Kizzmekia Corbett ’08, M16, biological sciences, says it feels like she’s “living in a constant adrenaline rush.” Maybe that’s because she and her team at the Vaccine Research Center at the National Insti- tute of Allergy and Infectious Diseases have been working around the clock for weeks. They’re racing to develop a vaccine for the coronavirus faster than it can race across the globe. “To be living in this moment where I have the opportunity to work on something that has imminent global importance…it’s just a surre- al moment for me,” Corbett says. Despite it feeling surreal, the advances Corbett and her team are making are very real, and they’re setting records. “We are making better progress than I could have ever hoped for,” she says. After three months of studies in test tubes and in animals, the vaccine her team developed is about to enter a phase I clinical trial, a crucial hur- dle on the way to FDA approval. Read the complete article about Kizzmekia and her team’s efforts to develop a Covid-19 vaccine in the latest UMBC magazine at https:// Kizzmekia Corbett, NIH magazine.umbc.edu/umbc-alumnae-racing-to-develop- coronavirus-vaccine/. -
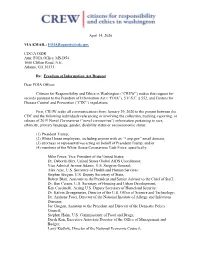
[email protected] CDC/ATSDR Attn
April 14, 2020 VIA EMAIL: [email protected] CDC/ATSDR Attn: FOIA Office, MS-D54 1600 Clifton Road, N.E. Atlanta, GA 30333 Re: Freedom of Information Act Request Dear FOIA Officer: Citizens for Responsibility and Ethics in Washington (“CREW”) makes this request for records pursuant to the Freedom of Information Act (“FOIA”), 5 U.S.C. § 552, and Centers for Disease Control and Prevention (“CDC”) regulations. First, CREW seeks all communications from January 29, 2020 to the present between the CDC and the following individuals referencing or involving the collection, tracking, reporting, or release of 2019 Novel Coronavirus (“novel coronavirus”) information pertaining to race, ethnicity, primary language, gender, disability status or socioeconomic status: (1) President Trump; (2) White House employees, including anyone with an “*.eop.gov” email domain; (3) attorneys or representatives acting on behalf of President Trump; and/or (4) members of the White House Coronavirus Task Force, specifically: Mike Pence, Vice President of the United States; Dr. Deborah Birx, United States Global AIDS Coordinator; Vice Admiral Jerome Adams, U.S. Surgeon General; Alex Azar, U.S. Secretary of Health and Human Services; Stephen Biegun, U.S. Deputy Secretary of State; Robert Blair, Assistant to the President and Senior Advisor to the Chief of Staff; Dr. Ben Carson, U.S. Secretary of Housing and Urban Development; Ken Cuccinelli, Acting U.S. Deputy Secretary of Homeland Security; Dr. Kelvin Droegemeier, Director of the U.S. Office of Science and Technology; Dr. Anthony Fauci, Director of the National Institute of Allergy and Infectious Diseases; Joe Grogan, Assistant to the President and Director of the Domestic Policy Council; Stephen Hahn, U.S. -

White House Briefing Call Notes 7.8.2020
Office of Intergovernmental Affairs State, Local, and Tribal Leaders – Thank you to the State, local, and Tribal leaders who joined for the White House COVID-19 National Briefing Call on Wednesday, July 8. Attendees heard comprehensive updates and insights on continuing support for State, local, and Tribal response, recovery, and reopening efforts from Larry Kudlow (Assistant to the President for Economic Policy), Secretary Robert Wilkie (U.S. Department of Veterans Affairs), Ambassador Deborah Birx (White House Coronavirus Task Force Coordinator), U.S. Surgeon General Gerome Adams, Deputy Surgeon General Erica Schwartz, and Assistant Secretary Frank Brogan (U.S. Department of Education). Below, please find pertinent announcements from across the Federal family and a brief recap of yesterday's call, including information and guidance from the White House Summit on Reopening America’s Schools. We would also like to flag CDC’s online testing resource page where you can find up-to-date testing information. Recent Announcements Paycheck Protection Program (PPP) Extended Through August: On July 4, President Trump signed legislation (S. 4116) reauthorizing the Paycheck Protection Program through August 8, 2020. Enacted in March as part of the CARES Act, the $669 billion program has approved more than 4.8 million loans totaling more than $520 billion and supporting over 51 million jobs to date. The extension of the program through August will make available the remaining $134 billion to small businesses and qualifying entities. Learn more about the PPP here. Department of the Treasury’s OIG released reporting requirements for CRF recipients: On July 2, Department of the Treasury’s Office of Inspector General (OIG) released a memorandum with instructions for recipients of the CARES Act’s Coronavirus Relief Fund (CRF). -

Uniformed Services University Board of Regents
Uniformed Services University of the Health Sciences “Learning to Care for Those in Harm’s Way” Board of Regents Quarterly Meeting November 5, 2019 BOARD OF REGENTS UNIFORMED SERVICES UNIVERSITY OF THE HEALTH SCIENCES 208th MEETING November 5, 2019 | 8:00 a.m. Alvarez Board of Regents Room (D-3001) | Bethesda, MD MEETING AGENDA OPEN MEETING 8:00 a.m.: Meeting Call to Order Designated Federal Officer Ms. Sarah Marshall 8:00 - 8:05 a.m.: Opening Comments Chair, USU Board of Regent Dr. Jonathan Woodson 8:05 - 8:10 a.m.: Matters of General Consent Declaration of Board Actions Dr. Woodson 8:10 - 8:20 a.m.: Board Actions Degree Conferrals, Hébert School of Medicine (SOM) Dean, SOM Dr. Arthur Kellermann Degree Conferrals, Inouye Graduate School of Nursing (GSN) Dean, GSN Dr. Carol Romano Degree Conferrals, College of Allied Health Sciences (CAHS) Dean, CAHS Dr. Mitchell Seal Faculty Appointments and Promotions, SOM Dean, SOM Dr. Kellermann Faculty Appointments and Promotions, PDC Executive Dean, PDC Dr. Schneid Faculty Awards, SOM Dean, SOM Dr. Kellermann 8:20 - 8:45 a.m.: Office of the President, Uniformed Services University of the Health Sciences (USU) Report President, USU Dr. Richard Thomas 8:45 - 9:25 a.m.: Member Reports Academics Summary Board Member Dr. Michael Johns Dr. Johns will provide the Board with a summary of reports from the University Registrar; the Office of Accreditation and Organizational Assessment; and the Faculty Senate. Finance and Administration Summary Board Member Dr. Leo Rouse Dr. Rouse will provide the Board with a summary of reports from the Office of the Vice President for Finance and Administration; the Office of the Vice President for Information and Education Technology; the Office of General Counsel; and the Henry M. -
The Enablers Barbara Kellerman Index More Information © in T
Cambridge University Press 978-1-108-83832-0 — The Enablers Barbara Kellerman Index More Information Index Access Hollywood tape, 89 Atlas, Scott, 237–238 Adams, Jerome, 136, 154, 239–240 authoritarianism Adelson, Sheldon, 47 of base supporters of Trump, 24–25 administration of Donald Trump democracy and, 266–267 Alex Azar, 186–188 soft dictatorship and, 270–271 demographics, 57 of Trump, 24–25, 266–267 dysfunctionality of, 57–58 Azar, Alex, 186–188 early signs of crowd size lies, 55 Bacow, Lawrence, 146–147 inaugural address, 54–55 bad leadership/followership categories family involvement, 56 ineffective, 15 Hope Hicks, 207–208 unethical, 15 H. R. McMaster, 60–61 Bannon, Steve, 73 James Mattis, 61–62 Barr, William, 181–186 John Kelly, 61 Barrack, Tom, 72–73 Kellyanne Conway, 207–208 base supporters of Trump loyalty tests, 64–67 COVID-19 and, 32 Mark Meadows, 196–199 deference to authoritarianism, 24–25 media savviness importance, 57 defined, 22 Mick Mulvaney, 195–196 demographics, 22–23, 33 Mike Pence, 171–176 devotion of, 19–21, 31–33 Mike Pompeo, 176–179 and economic disenfranchisement, military appointees, 56 24 Peter Navarro, 199–201 ethnicity of, 22–23 Rex Tillerson, 59–60 polling of, 265–266 Robert O’Brien, 201–202 relationship to truth, 33–34 Sonny Perdue, 271 types of, 21–22 Steven Mnuchin, 179–181 Bethrothed, The,94 subordinate subservience, 67–70 birtherism, 160 turnover, 61–64 Birx, Deborah, 121, 145, 197–198, wealth of, 56 242–246 William Barr, 181–186 Black Death, 96–98 advisors. See senior advisors, Trump Black Lives Matter, -

Sault Tribe Membership Services Contacts
Win Awenen Nisitotung June 21, 2019 • Vol. 40 No. 6 Strawberry Moon Ode’imin Giizis Official newspaper of the Sault Ste. Marie Tribe of Chippewa Indians ARC brings REDress Project to Sault Ste. Marie Photo by Rick Smith BY RICK SMITH Canadian Metis artist Jaime Last April, the Not Invisible murder is the third leading cause prayer circle on May 5 as a way Over a dozen red dresses hung Black initiated the project several Act of 2019 was introduced in the of death among American Indian of healing, sharing stories and among the trees along Shunk years ago, it spread across Canada Senate. The bill would increase women; and reliable data on raising awareness for missing and Road in Sault Ste. Marie, Mich., and into the United States. coordination between federal the prevalence of MMIW is not murdered indigenous women and appeared as phantoms when first In the meantime, the subject agencies to identify and combat available. girls. noticed. The display was part of MMIW reached the chambers violent crime in Indian Country The U.S. Senate also des- The ARC staff said they were of the The REDress Project, an of the U.S. Congress as well as and of Indians. The bill notes ignated May 5 as a national thrilled to see the community international campaign to call those of the National Congress the National Institute of Justice Day of Awareness for missing involvement in raising awareness attention to the plight of mur- of American Indians (NCAI). In reports more than 80 percent of and murdered Native women and the REDress display was just dered and missing indigenous 2016, the NCAI passed a resolu- American Indian men and women and girls. -

COVID-19 Updates Memo
October 13, 2020 TO: ALL COUNTY COMMISSIONERS, COUNTY EXECUTIVES, COUNTY COUNCIL MEMBERS, COUNTY ADMINISTRATORS AND COUNTY CLERKS FROM: CHERYL SUBLER, EXECUTIVE DIRECTOR RACHEL MASSOUD, POLICY ANALYST ADAM SCHWIEBERT, POLICY ANALYST RE: OCTOBER 13, 2020 COVID-19 UPDATES Key Resources 1. CCAO CARES Act Funds Resources Webpage 2. Important Deadlines for CARES Act Coronavirus Relief Funds 3. OBM Ideas on How to Use Coronavirus Relief Funding 4. OBM CARES Act Funds Guidance 10.1.2020 5. CCAO Guidance on Using CARES Act Funds 6. Treasury Guidance CARES Act Funds 9.2.2020 7. Treasury CARES Act Funds FAQs 9.2.2020 CCAO COVID-19 Resources Page Gov. DeWine’s Press Conference During today’s press conference, Gov. DeWine discussed Ohio’s increasing positivity rate for COVID-19. The administration added a new Lab Capacity dashboard to help private entities administering COVID-19 tests find labs that can run the samples. The dashboard is available at coronavirus.ohio.gov. There was an increase of 1,447 total COVID-19 cases statewide from yesterday’s data. For more COVID-19 numbers, visit coronavirus.ohio.gov. A video of the governor’s October 13th press conference can be found here. The next COVID-19 press conference is scheduled for Thursday, October 15th at 2 p.m. Press conferences can be viewed on www.ohiochannel.org. White House Briefing Call Registration – October 14th The White House Office of Intergovernmental Affairs will host a COVID-19 National Briefing Call for State, Local, and Tribal Officials on Wednesday, October 14, at 1:00 p.m. Eastern Time. -

Super Majorities Face Democrat Test 10 Races in House, Senate Races South and in Fort Wayne Will Determine Clout by BRIAN A
V20, N9 Thursday Oct. 9, 2014 Super majorities face Democrat test 10 races in House, Senate races south and in Fort Wayne will determine clout By BRIAN A. HOWEY INDIANAPOLIS – Beleaguered Indiana House Democrats need to make a net pickup of four House seats on Nov. 4 to break the 69- 31 seat Republican super majority. The reality is that with the retirement of State Rep. Kreg Battles in HD45 and the reemergence of former Republican representative Bruce Borders, that seat al- most certainly ends up Republican Reps. Ed Soliday (top left) and Jack Lutz (lower right) and Sens. Ron in the GOP column, so Grooms (top) and Jim Smith are all facing tough challenges from Democrats. Democrats need to pick up five seats elsewhere. While the odds are moderately against such a given the right conditions.” pickup, Republican operatives knew that in the right condi- In the Indiana Senate, three tossup races along tions, the loss of up to six House seats was not beyond the Ohio River, including two held by Republicans, and rac- doubt. As Indiana Democratic Chairman John Zody told es in Fort Wayne and a challenge to State Sen. Mike Delph HPI earlier this month, “There are enough seats in range Continued on page 3 Walorski & the toll road By JACK COLWELL SOUTH BEND – While pundits and pollsters evalu- ate issues of great pith and moment for effect on elec- tions, local peeves with no link to the great issues can decide a congressional race. Back in 2006, Chris “I think the time is coming down Chocola, then the Republican congressman in Indiana’s the road when it is going to be 2nd District, said early in that beyond only same-sex marriage. -

Covid-19: FDA Authorizes Moderna Vaccine As US Starts Vaccinating Health Workers
NEWS BMJ: first published as 10.1136/bmj.m4924 on 21 December 2020. Downloaded from New York Cite this as: BMJ 2020;371:m4924 Covid-19: FDA authorizes Moderna vaccine as US starts vaccinating http://dx.doi.org/10.1136/bmj.m4924 health workers Published: 21 December 2020 Janice Hopkins Tanne The US Food and Drug Administration (FDA) President Donald Trump has neither received the authorized the Moderna vaccine against covid-19 for vaccine nor made a statement about vaccine emergency use on 18 December, with the US on track distribution. to receive 20 million doses by the end of this month Side effects and a further 85-100 million doses in the first three months of 2021.1 Both Moderna’s and Pfizer-BioNTech’s vaccines use the new messenger RNA (mRNA) technology, but The move follows the authorization of the Moderna’s vaccine can be kept cold in an ordinary Pfizer-BioNTech vaccine for emergency use a week freezer, whereas the Pfizer-BioNTech vaccine must ago. Both vaccines are said to have around 95% be kept at –70°C. efficacy. Pfizer and Moderna have said that they will apply to the FDA for full licensure. Vaccines from Both vaccines require two injections: 21 days apart other makers are expected in early 2021. for the Pfizer vaccine and 28 days apart for the Moderna vaccine. Side effects have been reported Infections and deaths increase in the US every day. with both: pain at the injection site, muscle aches As of 20 December it recorded 193 947 new cases, 2628 and pains, and sometimes a slight fever. -

Black Scientist Suggests COVID-19 Is a 'Genocide' Against Blacks
4/21/2020 Black Scientist Suggests COVID-19 Is a 'Genocide' Against Blacks, Department of Health Launches Investigation Into Her Tweets Black Scientist Suggests COVID-19 Is a ‘Genocide’ Against Blacks, Department of Health Launches Investigation Into Her Tweets By Nefeteria Brewster - April 20, 2020 The Department of Health and Human Services is investigating a controversial series of tweets posted by a Black scientist who has been a vital researcher in the race to create a vaccine for COVID-19, Fox News reported. Many know Dr. Kizzmekia Corbett, a viral immunologist working with the National Institute of Allergy and Infectious Diseases, as a lead researcher with Dr. Barney Graham’s coronavirus team in the Vaccine Research Center, which is part of the National Institutes of Health. https://atlantablackstar.com/2020/04/20/black-scientist-suggests-covid-19-is-a-genocide-against-blacks-department-of-health-launches-investigation-into-her-tweets/ 1/7 4/21/2020 Black Scientist Suggests COVID-19 Is a 'Genocide' Against Blacks, Department of Health Launches Investigation Into Her Tweets Kizzmekia Corbett is a research fellow at the NIH Vaccine Research Center and a key member of a team helping to develop a vaccine for the COVID-19 virus. (Photo: UNC School of Medicine) Recently Corbett has been drawing public attention because of her social media presence, particularly several controversial tweets on her Twitter page. Some of the tweets date back to the beginning of February. On March 29 Corbett tweeted a link to a Bloomberg article about the impact of the virus on poor communities. In her accompanying comments, she suggested that doctors may choose to overlook Blacks if ventilators are in short supply. -

March 4, 2020 VIA EMAIL, FOIA ONLINE, ONLINE PORTAL OR FACSIMILE Michael Marquis Freedom of Information Officer Department of He
March 4, 2020 VIA EMAIL, FOIA ONLINE, ONLINE PORTAL OR FACSIMILE Michael Marquis Hugh Gilmore Freedom of Information Officer Freedom of Information Officer Department of Health and Human Centers for Medicare & Medicaid Services Services Hubert H. Humphrey Building, Room North Building, Room N2-20-06 729H 7500 Security Boulevard 200 Independence Avenue SW Baltimore, MD 21244 Washington, DC 20201 [email protected] [email protected] Freedom of Information Officer Freedom of Information Officer Administration for Children & Families U.S. Centers for Disease Control and U.S. Department of Health and Human Prevention Services 1600 Clifton Road NE 330 C Street SW Building 57, Room MS D-54 Washington, DC 20201 Atlanta, GA 30333 [email protected] [email protected] Office of Information Programs and NIH FOIA Office Services Building 31 Room 5B35 U.S. Department of State 31 Center Drive, MSC 2107 A/GIS/IPS/RL Bethesda, MD 20892 SA-2, Suite 8100 [email protected] Washington, DC 20522 [email protected] Robin Schofield National Institute of Allergy and Chief Privacy Officer/Chief FOIA Officer Infectious Diseases The Privacy Office Room 6G51 U.S. Department of Homeland Security 5601 Fishers Lane 245 Murray Lane SW Rockville, MD 20892 Washington, DC 20528 [email protected] [email protected] Sarah Kotler FOIA Public Liaison Freedom of Information Officer U.S. Department of Education Food and Drug Administration Office of Management 5630 Fishers Lane, Room 1035 Office of the Chief Privacy Officer Rockville, MD 20857 400 Maryland Avenue SW, LBJ 2E320 Facsimile: (301) 827-9267 Washington, DC 20202-4536 [email protected] 1030 15th Street NW, Suite B255, Washington, DC 20005 | AmericanOversight.org U.S.