NCEZID's Strategic Plan 2012
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Arboviral Infection Surveillance Protocol
April 2013 Arboviral Infection Surveillance Protocol Arboviruses endemic to the U.S. include Eastern equine encephalitis virus (EEE), La Crosse encephalitis virus (LAC), Saint Louis encephalitis virus (SLE), West Nile virus (WNV), Western equine encephalitis virus (WEE), and the tickborne Powassan encephalitis virus (POW). See other materials for information on non-endemic arboviruses (e.g., dengue fever and yellow fever) Provider Responsibilities 1. Report suspect and confirmed cases of arbovirus infection (including copies of lab results) to the local health department within one week of diagnosis. Supply requested clinical information to the local health department to assist with case ascertainment. 2. Assure appropriate testing is completed for patients with suspected arboviral infection. The preferred diagnostic test is testing of virus-specific IgM antibodies in serum or cerebrospinal fluid (CSF). In West Virginia, appropriate arbovirus testing should include EEE, LAC, SLE, and WNV. Testing for a complete arboviral panel is available free of charge through the West Virginia Office of Laboratory Services (OLS). Laboratory Responsibilities 1. Report positive laboratory results for arbovirus infection to the local health department within 1 week. 2. Submit positive arboviral samples to the Office of Laboratory Services within 1 week. 3. Appropriate testing for patients with suspected arboviral infection includes testing of virus-specific IgM antibodies in serum or CSF. In West Virginia, testing should routinely be conducted for WNV, EEE, SLE, and LAC. A complete arboviral panel is available free of charge through OLS. For more information go to: http://www.wvdhhr.org/labservices/labs/virology/arbovirus.cfm Local Health Responsibilities 1. Conduct an appropriate case investigation. -

ABSTRACT DRAKE, STEPHENIE LYNN. the Ecology Vibrio
ABSTRACT DRAKE, STEPHENIE LYNN. The Ecology Vibrio vulnificus and Vibrio parahaemolyticus from Oyster Harvest Sites in the Gulf of Mexico. (Under the direction of Dr. Lee-Ann Jaykus). The Vibrionaceae are environmentally ubiquitous to estuarine waters. Two species in particular, V. vulnificus and V. parahaemolyticus, are important human pathogens that are transmitted by the consumption of contaminated molluscan shellfish. There is limited information available for the recent risk assessments; accordingly, the purpose of this study was to address some of these data gaps in the V. vulnificus and V. parahaemolyticus risk assessments. The objectives of this study were to (i) quantify the levels of total estuarine bacteria, total Vibrio spp., and specific levels of non-pathogenic and pathogenic V. vulnificus and V. parahaemolyticus over the harvest period; and (ii) determine if length of harvest time affects the levels of V. vulnificus. Oyster and water samples were harvested seasonally from 3 U.S. Gulf Coast sites over 2 years. Environmental parameters were monitored during harvesting. Both surface and bottom water samples (1 L) were taken at the beginning of harvesting and at the end of harvesting. Oyster samples (15 specimens for each time point) were taken at 0, 2.5, 5.0, 7.5, and 10 hrs intervals after being held at ambient temperature during harvesting. Samples were processed for many different bacteria. For enumeration of total V. parahaemolyticus, pathogenic V. parahaemolyticus, and V. vulnificus was done using colony lift hybridization (tlh, tdh+ and/or trh+, and vvhA gene targets, respectively). MPN methods were also used to obtain estimates of pathogenic V. -

MDHHS BOL Mosquito-Borne and Tick-Borne Disease Testing
MDHHS BUREAU OF LABORATORIES MOSQUITO-BORNE AND TICK-BORNE DISEASE TESTING MOSQUITO-BORNE DISEASES The Michigan Department of Health and Human Services Bureau of Laboratories (MDHHS BOL) offers comprehensive testing on clinical specimens for the following viral mosquito-borne diseases (also known as arboviruses) of concern in Michigan: California Group encephalitis viruses including La Crosse encephalitis virus (LAC) and Jamestown Canyon virus (JCV), Eastern Equine encephalitis virus (EEE), St. Louis encephalitis virus (SLE), and West Nile virus (WNV). Testing is available free of charge through Michigan healthcare providers for their patients. Testing for mosquito-borne viruses should be considered in patients presenting with meningitis, encephalitis, or other acute neurologic illness in which an infectious etiology is suspected during the summer months in Michigan. Methodologies include: • IgM detection for five arboviruses (LAC, JCV, EEE, SLE, WNV) • Molecular detection (PCR) for WNV only • Plaque Reduction Neutralization Test (PRNT) is also available and may be performed on select samples when indicated The preferred sample for arbovirus serology at MDHHS BOL is cerebral spinal fluid (CSF), followed by paired serum samples (acute and convalescent). In cases where CSF volume may be small, it is recommended to also include an acute serum sample. Please see the following document for detailed instructions on specimen requirements, shipping and handling instructions: http://www.michigan.gov/documents/LSGArbovirus_IgM_Antibody_Panel_8347_7.doc Michigan residents may also be exposed to mosquito-borne viruses when traveling domestically or internationally. In recent years, the most common arboviruses impacting travelers include dengue, Zika and chikungunya virus. MDHHS has the capacity to perform PCR for dengue, chikungunya and Zika virus and IgM for dengue and Zika virus to confirm commercial laboratory arbovirus findings or for complicated medical investigations. -

Kellie ID Emergencies.Pptx
4/24/11 ID Alert! recognizing rapidly fatal infections Susan M. Kellie, MD, MPH Professor of Medicine Division of Infectious Diseases, UNMSOM Hospital Epidemiologist UNMHSC and NMVAHCS Fever and…. Rash and altered mental status Rash Muscle pain Lymphadenopathy Hypotension Shortness of breath Recent travel Abdominal pain and diarrhea Case 1. The cross-country trucker A 30 year-old trucker driving from Oklahoma to California is hospitalized in Deming with fever and headache He is treated with broad-spectrum antibiotics, but deteriorates with obtundation, low platelet count, and a centrifugal petechial rash and is transferred to UNMH 1 4/24/11 What is your diagnosis? What is the differential diagnosis of fever and headache with petechial rash? (in the US) Tickborne rickettsioses ◦ RMSF Bacteria ◦ Neisseria meningitidis Key diagnosis in this case: “doxycycline deficiency” Key vector-borne rickettsioses treated with doxycycline: RMSF-case-fatality 5-10% ◦ Fever, nausea, vomiting, myalgia, anorexia and headache ◦ Maculopapular rash progresses to petechial after 2-4 days of fever ◦ Occasionally without rash Human granulocytotropic anaplasmosis (HGA): case-fatality<1% Human monocytotropic ehrlichiosis (HME): case fatality 2-3% 2 4/24/11 Lab clues in rickettsioses The total white blood cell (WBC) count is typicallynormal in patients with RMSF, but increased numbers of immature bands are generally observed. Thrombocytopenia, mild elevations in hepatic transaminases, and hyponatremia might be observed with RMSF whereas leukopenia -

1.1.1.2 Tick-Borne Encephalitis Virus
This thesis has been submitted in fulfilment of the requirements for a postgraduate degree (e.g. PhD, MPhil, DClinPsychol) at the University of Edinburgh. Please note the following terms and conditions of use: • This work is protected by copyright and other intellectual property rights, which are retained by the thesis author, unless otherwise stated. • A copy can be downloaded for personal non-commercial research or study, without prior permission or charge. • This thesis cannot be reproduced or quoted extensively from without first obtaining permission in writing from the author. • The content must not be changed in any way or sold commercially in any format or medium without the formal permission of the author. • When referring to this work, full bibliographic details including the author, title, awarding institution and date of the thesis must be given. Transcriptomic and proteomic analysis of arbovirus-infected tick cells Sabine Weisheit Thesis submitted for the degree of Doctor of Philosophy The Roslin Institute and Royal (Dick) School of Veterinary Studies, University of Edinburgh 2014 Declaration .................................................................................................... i Acknowledgements ..................................................................................... ii Abstract of Thesis ....................................................................................... iii List of Figures .............................................................................................. v List -

What Is Veterinary Public Health? Zoonosis
Your Zoonosis Connection Veterinary Public Health Division Volume 4, Issue 1 March 2012 612 Canino Rd., Houston, Texas 77076 Phone: 281-999-3191 Fax: 281-847-1911 Harris County Rabies Update Inside this issue: Rabies continues to be a serious health threat to people and domestic What is Veterinary 2 animals. In the United States prior to 1960, the majority of all animal cases re- Public Health ported to the Centers for Disease Control and Prevention were seen in do- Rabies Submissions 3 mestic animals. Now more than 90% of the cases occur in wild animals. Since the 1950s, human rabies deaths have declined from more than a 100 annually Continuing Education 3 to a couple each year. This reduction in the number of human deaths associat- ed with rabies can be attributed to the implementation of rabies vaccination Zoonosis Trivia 4 laws, oral rabies vaccination programs, improved public health practices and the increased administration of post-exposure prophylaxis. Did you know? Veterinarians are In Harris County, rabies was last documented in a dog in 1979 and in a cat in uniquely qualified to 1986. However, rabies continues to be enzootic in our bat population. In address issues and 2011, 4.3% of bats submitted for testing were positive for rabies, which has de- concerns related to clined from 7.9% in 2010 (see table below). Last year, one horse and two the interactions of skunks tested positive for rabies in Harris County. The horse was infected people, animals, and with the South Central Skunk strain of rabies, which often spills over into oth- the environment. -

Vol. XXV Issue No. 2 June 2004
Vol. XXV Issue No. 2 June 2004 Report on the Enhanced Surveillance for Chlamydia West Nile Virus - 2003 Summary and in Women - South Carolina, 1998-2002 the Upcoming Season WAYNE A. DUFFUS, MD, PhD LENA M. BRETOUS, MD, MPH Medical Consultant Medical Consultant Extent of Chlamydia Problem Chlamydia remains a significant health threat among In 2003, South Carolina recorded six human cases of women and adolescents. Most estimates predict that 1 in 20 West Nile Virus (WNV). Surveillance numbers for other WNV sexually active woman of childbearing age or 1 in 10 adoles- positives in 2003 include: 282 birds, 54 equine, 3 mosquito cent girls are infected with chlamydia. In fact, 90% of all pools, and 1 alpaca. See table on page reported cases are in individuals less than 24 years of age. three for human case description. INSIDE THIS ISSUE Unfortunately, 60 – 80% of infected women have no symp- Because of the long stretch of toms, and therefore are not aware of their infection and may warm weather in spring and fall, in- Report on the Enhanced not seek health care. fected mosquitoes have a longer win- Surveillance for Chlamydia is the most commonly reported sexually dow to spread the disease in South Chlamydia in Women - South Carolina, transmitted infection among women in the United States (US). Carolina. The first human WNV case 1998 - 2002 The southeast led the nation in chlamydia prevalence in 2002. in South Carolina during 2003 was also Pg. 1 For example, there were 451.1 cases/100,000 persons diag- the first recorded case in the country nosed in the U.S. -

ICD-9 Diagnosis Codes Effective 10/1/2011 (V29.0) Source: Centers for Medicare and Medicaid Services
ICD-9 Diagnosis Codes effective 10/1/2011 (v29.0) Source: Centers for Medicare and Medicaid Services 0010 Cholera d/t vib cholerae 00801 Int inf e coli entrpath 01086 Prim prg TB NEC-oth test 0011 Cholera d/t vib el tor 00802 Int inf e coli entrtoxgn 01090 Primary TB NOS-unspec 0019 Cholera NOS 00803 Int inf e coli entrnvsv 01091 Primary TB NOS-no exam 0020 Typhoid fever 00804 Int inf e coli entrhmrg 01092 Primary TB NOS-exam unkn 0021 Paratyphoid fever a 00809 Int inf e coli spcf NEC 01093 Primary TB NOS-micro dx 0022 Paratyphoid fever b 0081 Arizona enteritis 01094 Primary TB NOS-cult dx 0023 Paratyphoid fever c 0082 Aerobacter enteritis 01095 Primary TB NOS-histo dx 0029 Paratyphoid fever NOS 0083 Proteus enteritis 01096 Primary TB NOS-oth test 0030 Salmonella enteritis 00841 Staphylococc enteritis 01100 TB lung infiltr-unspec 0031 Salmonella septicemia 00842 Pseudomonas enteritis 01101 TB lung infiltr-no exam 00320 Local salmonella inf NOS 00843 Int infec campylobacter 01102 TB lung infiltr-exm unkn 00321 Salmonella meningitis 00844 Int inf yrsnia entrcltca 01103 TB lung infiltr-micro dx 00322 Salmonella pneumonia 00845 Int inf clstrdium dfcile 01104 TB lung infiltr-cult dx 00323 Salmonella arthritis 00846 Intes infec oth anerobes 01105 TB lung infiltr-histo dx 00324 Salmonella osteomyelitis 00847 Int inf oth grm neg bctr 01106 TB lung infiltr-oth test 00329 Local salmonella inf NEC 00849 Bacterial enteritis NEC 01110 TB lung nodular-unspec 0038 Salmonella infection NEC 0085 Bacterial enteritis NOS 01111 TB lung nodular-no exam 0039 -

Marburg Hemorrhagic Fever Fact Sheet
Marburg Hemorrhagic Fever Fact Sheet What is Marburg hemorrhagic fever? Marburg hemorrhagic fever is a rare, severe type of hemorrhagic fever which affects both humans and non-human primates. Caused by a genetically unique zoonotic (that is, animal-borne) RNA virus of the filovirus family, its recognition led to the creation of this virus family. The four species of Ebola virus are the only other known members of the filovirus family. Marburg virus was first recognized in 1967, when outbreaks of hemorrhagic fever occurred simultaneously in laboratories in Marburg and Frankfurt, Germany and in Belgrade, Yugoslavia (now Serbia). A total of 37 people became ill; they included laboratory workers as well as several medical personnel and Negative stain image of an isolate of Marburg virus, family members who had cared for them. The first people showing filamentous particles as well as the infected had been exposed to African green monkeys or characteristic "Shepherd's Crook." Magnification their tissues. In Marburg, the monkeys had been imported approximately 100,000 times. Image courtesy of for research and to prepare polio vaccine. Russell Regnery, Ph.D., DVRD, NCID, CDC. Where do cases of Marburg hemorrhagic fever occur? Recorded cases of the disease are rare, and have appeared in only a few locations. While the 1967 outbreak occurred in Europe, the disease agent had arrived with imported monkeys from Uganda. No other case was recorded until 1975, when a traveler most likely exposed in Zimbabwe became ill in Johannesburg, South Africa – and passed the virus to his traveling companion and a nurse. 1980 saw two other cases, one in Western Kenya not far from the Ugandan source of the monkeys implicated in the 1967 outbreak. -
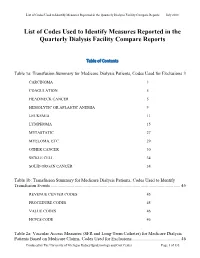
List of Codes Used to Identify Measures Reported in the QDFC
List of Codes Used to Identify Measures Reported in the Quarterly Dialysis Facility Compare Reports July 2018 List of Codes Used to Identify Measures Reported in the Quarterly Dialysis Facility Compare Reports Table of Contents Table 1a: Transfusion Summary for Medicare Dialysis Patients, Codes Used for Exclusions 3 CARCINOMA 3 COAGULATION 5 HEAD/NECK CANCER 5 HEMOLYTIC OR APLASTIC ANEMIA 9 LEUKEMIA 11 LYMPHOMA 15 METASTATIC 27 MYELOMA, ETC. 29 OTHER CANCER 30 SICKLE CELL 34 SOLID ORGAN CANCER 34 Table 1b: Transfusion Summary for Medicare Dialysis Patients, Codes Used to Identify Transfusion Events .................................................................................................................. 45 REVENUE CENTER CODES 45 PROCEDURE CODES 45 VALUE CODES 46 HCPCS CODE 46 Table 2a: Vascular Access Measures (SFR and Long-Term Catheter) for Medicare Dialysis Patients Based on Medicare Claims, Codes Used for Exclusions ........................................... 46 Produced by The University of Michigan Kidney Epidemiology and Cost Center Page 1 of 135 List of Codes Used to Identify Measures Reported in the Quarterly Dialysis Facility Compare Reports July 2018 COMA 46 END STAGE LIVER DISEASE 48 METASTATIC CANCER 48 Table 2b: Standardized Fistulae Rate (SFR) for Medicare Dialysis Patients Based on Medicare Claims, Codes Used for Prevalent Comorbidities Adjusted in Model .................................... 50 ANEMIA 50 CORONARY ARTERY DISEASE 52 CONGESTIVE HEART FAILURE 55 CEREBROVASCULAR DISEASE 56 CHRONIC OBSTRUCTIVE PULMONARY DISEASE 68 DIABETES 69 DRUG DEPENDENCE 79 INFECTIONS (NON-VASCULAR ACCESS-RELATED): 93 PERIPHERAL VASCULAR DISEASE (INCLUDES ARTERIAL, VENOUS AND NONSPECIFIC DISEASES) 124 Table 3: Dialysis Adequacy ................................................................................................... -

Client Services Manual Public Health Laboratory
CLIENT SERVICES MANUAL PUBLIC HEALTH LABORATORY COUNTY OF SANTA CLARA 2220 MOORPARK AVE, 2ND FLOOR SAN JOSE, CA 95128 (P) 408.885.4272 | (F) 408.885.4275 http://www.sccgov.org/sites /sccphd/en-us/HealthProviders/Lab Patricia Dadone, Public Health Laboratory Director Sara H. Cody, MD, Health Officer and Public Health Director Table of Contents 1 GENERAL INFORMATION ............................................................................................... 1.1 ROLE .............................................................................................................................................................. 1.1 MISSION STATEMENT ..................................................................................................................................... 1.1 ABBREVIATIONS.............................................................................................................................................. 1.2 LABORATORY CERTIFICATIONS ........................................................................................................................ 1.4 CLIENT SERVICES ............................................................................................................................................ 1.5 Hours of Operation: .............................................................................................................................. 1.5 Supplies .................................................................................................................................................. -

COMENIUS UNIVERSITY in BRATISLAVA Faculty of Natural Sciences
COMENIUS UNIVERSITY IN BRATISLAVA Faculty of Natural Sciences UNIVERSITY OF CAGLIARI Department of Biomedical Sciences MOLECULAR EPIDEMIOLOGY OF HANTAVIRUSES IN CENTRAL EUROPE AND ANTIVIRAL SCREENING AGAINST ZOONOTIC VIRUSES CAUSING HEMORRHAGIC FEVERS DISSERTATION 2017 RNDr. PaedDr. Róbert SZABÓ COMENIUS UNIVERSITY IN BRATISLAVA Faculty of Natural Sciences UNIVERSITY OF CAGLIARI Department of Biomedical Sciences MOLECULAR EPIDEMIOLOGY OF HANTAVIRUSES IN CENTRAL EUROPE AND ANTIVIRAL SCREENING AGAINST ZOONOTIC VIRUSES CAUSING HEMORRHAGIC FEVERS Dissertation Study program: Virology Molecular and Translational Medicine Field of Study: Virology Place of the study: Biomedical Research Center, SAS in Bratislava, Slovakia Department of Biomedical Sciences, Cittadella Universitaria, Monserrato, Italy Supervisors: RNDr. Boris Klempa, DrSc. Prof. Alessandra Pani Bratislava, 2017 RNDr. PaedDr. Róbert SZABÓ 25276874 Univerzita Komenského v Bratislave Prírodovedecká fakulta ZADANIE ZÁVEREČNEJ PRÁCE Meno a priezvisko študenta: RNDr. PaedDr. Róbert Szabó Študijný program: virológia (Jednoodborové štúdium, doktorandské III. st., denná forma) Študijný odbor: virológia Typ záverečnej práce: dizertačná Jazyk záverečnej práce: anglický Sekundárny jazyk: slovenský Názov: Molecular epidemiology of hantaviruses in Central Europe and antiviral screening against zoonotic viruses causing hemorrhagic fevers Molekulárna epidemiológia hantavírusov v strednej Európe a antivírusový skríning proti zoonotickým vírusom spôsobujúcim hemoragické horúčky Cieľ: Main objectives