Download This PDF File
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
The Provider-Based Evaluation (Probe) 2014 Preliminary Report
The Provider-Based Evaluation (ProBE) 2014 Preliminary Report I. Background of ProBE 2014 The Provider-Based Evaluation (ProBE), continuation of the formerly known Malaysia Government Portals and Websites Assessment (MGPWA), has been concluded for the assessment year of 2014. As mandated by the Government of Malaysia via the Flagship Coordination Committee (FCC) Meeting chaired by the Secretary General of Malaysia, MDeC hereby announces the result of ProBE 2014. Effective Date and Implementation The assessment year for ProBE 2014 has commenced on the 1 st of July 2014 following the announcement of the criteria and its methodology to all agencies. A total of 1086 Government websites from twenty four Ministries and thirteen states were identified for assessment. Methodology In line with the continuous and heightened effort from the Government to enhance delivery of services to the citizens, significant advancements were introduced to the criteria and methodology of assessment for ProBE 2014 exercise. The year 2014 spearheaded the introduction and implementation of self-assessment methodology where all agencies were required to assess their own websites based on the prescribed ProBE criteria. The key features of the methodology are as follows: ● Agencies are required to conduct assessment of their respective websites throughout the year; ● Parents agencies played a vital role in monitoring as well as approving their agencies to be able to conduct the self-assessment; ● During the self-assessment process, each agency is required to record -

The Development of English Education in Kota Setar, 1909- 1957
International Journal of Academic Research in Business and Social Sciences Vol. 10, No. 9, 2020, E-ISSN: 2222 -6990 © 2020 HRMARS The Development of English Education in Kota Setar, 1909- 1957 Muhammad Qiwamuddin Alif Mahamad Najib, Khairi Ariffin To Link this Article: http://dx.doi.org/10.6007/IJARBSS/v10-i9/7981 DOI:10.6007/IJARBSS/v10-i9/7981 Received: 25 July 2020, Revised: 17 August 2020, Accepted: 30 August 2020 Published Online: 25 September 2020 In-Text Citation: (Najib, & Ariffin, 2020) To Cite this Article: Najib, M. Q. A. M., & Ariffin, K. (2020). The Development of English Education in Kota Setar, 1909-1957. International Journal of Academic Research in Business and Social Sciences. 10(9), 1011-1022. Copyright: © 2020 The Author(s) Published by Human Resource Management Academic Research Society (www.hrmars.com) This article is published under the Creative Commons Attribution (CC BY 4.0) license. Anyone may reproduce, distribute, translate and create derivative works of this article (for both commercial and non-commercial purposes), subject to full attribution to the original publication and authors. The full terms of this license may be seen at: http://creativecommons.org/licences/by/4.0/legalcode Vol. 10, No. 9, 2020, Pg. 1011 - 1022 http://hrmars.com/index.php/pages/detail/IJARBSS JOURNAL HOMEPAGE Full Terms & Conditions of access and use can be found at http://hrmars.com/index.php/pages/detail/publication-ethics 1011 International Journal of Academic Research in Business and Social Sciences Vol. 10, No. 9, 2020, E-ISSN: 2222 -6990 © 2020 HRMARS The Development of English Education in Kota Setar, 1909-1957 Muhammad Qiwamuddin Alif Mahamad Najib, Khairi Ariffin Sultan Idris Education University, 35900 Tanjong Malim, Perak Abstract This research aims to study the development of English education in Kota Setar from 1909 to 1957. -

(CPRC), Disease Control Division, the State Health Departments and Rapid Assessment Team (RAT) Representative of the District Health Offices
‘Annex 26’ Contact Details of the National Crisis Preparedness & Response Centre (CPRC), Disease Control Division, the State Health Departments and Rapid Assessment Team (RAT) Representative of the District Health Offices National Crisis Preparedness and Response Centre (CPRC) Disease Control Division Ministry of Health Malaysia Level 6, Block E10, Complex E 62590 WP Putrajaya Fax No.: 03-8881 0400 / 0500 Telephone No. (Office Hours): 03-8881 0300 Telephone No. (After Office Hours): 013-6699 700 E-mail: [email protected] (Cc: [email protected] and [email protected]) NO. STATE 1. PERLIS The State CDC Officer Perlis State Health Department Lot 217, Mukim Utan Aji Jalan Raja Syed Alwi 01000 Kangar Perlis Telephone: +604-9773 346 Fax: +604-977 3345 E-mail: [email protected] RAT Representative of the Kangar District Health Office: Dr. Zulhizzam bin Haji Abdullah (Mobile: +6019-4441 070) 2. KEDAH The State CDC Officer Kedah State Health Department Simpang Kuala Jalan Kuala Kedah 05400 Alor Setar Kedah Telephone: +604-7741 170 Fax: +604-7742 381 E-mail: [email protected] RAT Representative of the Kota Setar District Health Office: Dr. Aishah bt. Jusoh (Mobile: +6013-4160 213) RAT Representative of the Kuala Muda District Health Office: Dr. Suziana bt. Redzuan (Mobile: +6012-4108 545) RAT Representative of the Kubang Pasu District Health Office: Dr. Azlina bt. Azlan (Mobile: +6013-5238 603) RAT Representative of the Kulim District Health Office: Dr. Sharifah Hildah Shahab (Mobile: +6019-4517 969) 71 RAT Representative of the Yan District Health Office: Dr. Syed Mustaffa Al-Junid bin Syed Harun (Mobile: +6017-6920881) RAT Representative of the Sik District Health Office: Dr. -

Infiltration Study for Urban Soil: Case Study of Sungai Kedah Ungauged Catchment
Journal of Environmental Science and Engineering B 3 (2014) 291-299 doi: 10.17265/2162-5263/2014.06.001 D DAVID PUBLISHING Infiltration Study for Urban Soil: Case Study of Sungai Kedah Ungauged Catchment Steven Poh Tze Wei and Khirluddin Bin Abdullah Department of Irrigation and Drainage, Division of Water Resources and Hydrology, Kuala Lumpur 68000, Malaysia Abstract: The DID (Department of Irrigation and Drainage) in Malaysia has produced a manual on urban stromwater management specifically for the Malaysia region with usage of infiltration method towards controlling the quantity and quality of surface runoff. With this method, the volume of surface runoff can be reduced and flood problems in major cities can be eliminated. The study areas of Sungai Kedah ungauged catchment are located at the northern region of Malaysia. The Kota Setar sub-catchment is located at the downstream of Sungai Kedah with the newly completed development of control barrage at the upper Kota Setar. This paper will describe the analyses of the infiltration curves at Kota Setar. The resulting infiltration maps have developed based on the infiltration capacities. Key words: Sungai Kedah ungauged catchment, type of soil, infiltration curve, infiltration map. 1. Introduction 2. Study Area Undeveloped land has a little surface runoff, due to The study area, Sungai Kedah catchment, is located most precipitation infiltrate into the topsoil and the at the northern region of Malaysia as shown in Fig. 2. occurrence of hydraulic conductivity flow through as The nonlinear rainfall-runoff model [2] has been interflow into stream [1]. As a result of this process, applied to the Sungai Kedah catchment, which is located the precipitation effects are averaged out over a long in the northern region of Malaysia. -

Household Expenditure 2019 Kedah
MALAYSIA LAPORAN SURVEI PERBELANJAAN ISI RUMAH MENGIKUT NEGERI DAN DAERAH PENTADBIRAN HOUSEHOLD EXPENDITURE SURVEY REPORT BY STATE AND ADMINISTRATIVE DISTRICT KEDAH 2019 Pemakluman/Announcement: Kerajaan Malaysia telah mengisytiharkan Hari Statistik Negara (MyStats Day) pada 20 Oktober setiap tahun. Tema sambutan MyStats Day 2020 adalah “Connecting The World With Data We Can Trust”. The Government of Malaysia has declared National Statistics Day (MyStats Day) on 20th October each year. MyStats Day 2020 theme is “Connecting The World With Data We Can Trust”. JABATAN PERANGKAAN MALAYSIA DEPARTMENT OF STATISTICS, MALAYSIA Diterbitkan dan dicetak oleh/Published and printed by: Jabatan Perangkaan Malaysia Department of Statistics, Malaysia Blok C6, Kompleks C, Pusat Pentadbiran Kerajaan Persekutuan, 62514 Putrajaya, MALAYSIA Tel. : 03-8885 7000 Faks : 03-8888 9248 Portal : https://www.dosm.gov.my Facebook / Twitter / Instagram : StatsMalaysia Emel / Email : [email protected] (pertanyaan umum/general enquiries) [email protected] (pertanyaan & permintaan data/ data request & enquiries) Harga / Price : RM30.00 Diterbitkan pada Julai 2020/Published on July 2020 Hakcipta terpelihara/All rights reserved. Tiada bahagian daripada terbitan ini boleh diterbitkan semula, disimpan untuk pengeluaran atau ditukar dalam apa-apa bentuk atau alat apa jua pun kecuali setelah mendapat kebenaran daripada Jabatan Perangkaan Malaysia. Pengguna yang mengeluarkan sebarang maklumat dari terbitan ini sama ada yang asal atau diolah semula hendaklah meletakkan kenyataan -

Original Article Factors Associated with Thalassaemia Carrier Among Form Four Students in Kedah, Malaysia
Malaysian Journal of Public Health Medicine 2021, Vol. 21 (1): 134-140 ORIGINAL ARTICLE FACTORS ASSOCIATED WITH THALASSAEMIA CARRIER AMONG FORM FOUR STUDENTS IN KEDAH, MALAYSIA Rosidah Omar1, Norizan Ahmad1 and Ngee Wen Sze1 1 Family Health Unit, Kedah State Health Department, Ministry of Health Malaysia, Simpang Kuala, Jalan Kuala Kedah, 05400 Alor Setar, Kedah, Malaysia Corresponding author: Rosidah Omar Email: [email protected] ABSTRACT Thalassaemia and abnormal haemoglobins are the most common genetic disorder worldwide. School-based screening thalassaemia program for form four students was introduced with the objective to screen for the thalassaemia status. There is paucity in the data in Kedah on distribution of thalassaemia carrier and the associated factors. Hence this study aims to identify the factors associated with being a thalassaemia carrier and to describe the laboratory cost for the thalassaemia screening. This study used secondary data from the school-based thalassaemia screening in 2018 obtained from Kedah State Health Department. Results showed the prevalence of thalassaemia carrier among form four students in Kedah was 10.91%. Multivariate logistic regression showed that students from Baling, Padang Terap and Yan were 1.40, 1.34 and 1.23 times more likely to be a thalassaemia carrier respectively compared to Kota Setar (aOR Baling 1.40;95% CI 1.21,1.64; aOR Padang Terap 1.34;95% CI 1.11,1.61 and aOR Yan 1.23;95% CI 1.03,1.47). Malay and Siamese students were five times more likely be thalassaemia carriers compared to Indian (aOR Malay 5.16;95%CI 3.42,7.79, aOR Siamese 5.63;95%CI 3.19,9.97). -
03 CN18 PR Appendix 5 Infras
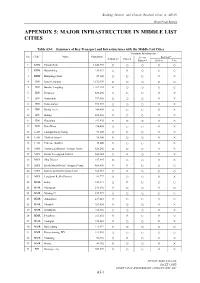
Building Disaster and Climate Resilient Cities in ASEAN Draft Final Report APPENDIX 5: MAJOR INFRASTRUCTURE IN MIDDLE LIST CITIES Table A5-1 Summary of Key Transport and Infrastructures with the Middle List Cities Transport Infrastructure *1 No. Code Name Population Access Railway*5 Airport*2 Port*3 Road*4 Station Line 1 KHM Phnom Pénh 1,242,992 ○ ○ ○ ○ ○ 2 KHM Băttâmbâng 140,533 ○ × ○ ○ ○ 3 KHM Kâmpóng Cham 47,300 ○ ○ ○ × × 4 IDN Kota Semarang 1,672,999 ○ ○ ○ ○ ○ 5 IDN Bandar Lampung 1,167,101 × ○ ○ ○ ○ 6 IDN Denpasar 880,600 ○ ○ ○ × × 7 IDN Samarinda 797,006 ○ ○ ○ × × 8 IDN Kota Ambon 395,423 ○ ○ ○ × × 9 IDN Banda Aceh 249,499 ○ ○ ○ × × 10 IDN Bitung 202,204 × ○ ○ × × 11 IDN Gorontalo 197,970 × ○ ○ × × 12 IDN Kota Bima 156,400 ○ ○ ○ × × 13 LAO Luangprabang (luang) 90,300 ○ ○ ○ × × 14 LAO Thalhek (kham) 90,800 × ○ ○ × × 15 LAO Pakxane (bolikh) 45,000 × ○ ○ × × 16 MYS Timur Laut District (George Town) 520,242 ○ ○ ○ × × 17 MYS Kuala Terengganu District 343,284 ○ × ○ × × 18 MYS Sibu District 247,995 ○ ○ ○ × × 19 MYS Kuala Muda District (Sungai Petani) 456,605 × × ○ ○ ○ 20 MYS Kota Setar District (Alor Setar) 366,787 ○ × ○ ○ ○ 21 MYS Langkawi Kedha District 94,777 ○ ○ ○ × × 22 MMR Kalay 348,573 ○ × ○ ○ ○ 23 MMR Myingyan 276,096 × ○ ○ × ○ 24 MMR Nyaung-U 239,947 ○ ○ ○ ○ ○ 25 MMR Amarapura 237,618 ○ ○ ○ ○ ○ 26 MMR Mrauk-U 189,630 × ○ ○ × × 27 MMR Kyaukpyu 165,352 ○ ○ ○ × × 28 MMR Pwintbyu 163,692 × × ○ × ○ 29 MMR Toungup 158,341 × ○ ○ × × 30 MMR Rathedaung 111,974 × ○ ○ ○ ○ 31 MMR Kyimyindaing-WY 111,514 ○ ○ ○ ○ ○ 32 MMR Manaung 56,966 ○ × ○ × × 33 MMR Hakha 48,352 × ○ ○ × × 34 PHL Batangas city 305,607 × ○ ○ × × NIPPON KOEI CO.,LTD. PAC ET C ORP. -

Appendix 3 Selection of Candidate Cities for Demonstration Project
Building Disaster and Climate Resilient Cities in ASEAN Final Report APPENDIX 3 SELECTION OF CANDIDATE CITIES FOR DEMONSTRATION PROJECT Table A3-1 Long List Cities (No.1-No.62: “abc” city name order) Source: JICA Project Team NIPPON KOEI CO.,LTD. PAC ET C ORP. EIGHT-JAPAN ENGINEERING CONSULTANTS INC. A3-1 Building Disaster and Climate Resilient Cities in ASEAN Final Report Table A3-2 Long List Cities (No.63-No.124: “abc” city name order) Source: JICA Project Team NIPPON KOEI CO.,LTD. PAC ET C ORP. EIGHT-JAPAN ENGINEERING CONSULTANTS INC. A3-2 Building Disaster and Climate Resilient Cities in ASEAN Final Report Table A3-3 Long List Cities (No.125-No.186: “abc” city name order) Source: JICA Project Team NIPPON KOEI CO.,LTD. PAC ET C ORP. EIGHT-JAPAN ENGINEERING CONSULTANTS INC. A3-3 Building Disaster and Climate Resilient Cities in ASEAN Final Report Table A3-4 Long List Cities (No.187-No.248: “abc” city name order) Source: JICA Project Team NIPPON KOEI CO.,LTD. PAC ET C ORP. EIGHT-JAPAN ENGINEERING CONSULTANTS INC. A3-4 Building Disaster and Climate Resilient Cities in ASEAN Final Report Table A3-5 Long List Cities (No.249-No.310: “abc” city name order) Source: JICA Project Team NIPPON KOEI CO.,LTD. PAC ET C ORP. EIGHT-JAPAN ENGINEERING CONSULTANTS INC. A3-5 Building Disaster and Climate Resilient Cities in ASEAN Final Report Table A3-6 Long List Cities (No.311-No.372: “abc” city name order) Source: JICA Project Team NIPPON KOEI CO.,LTD. PAC ET C ORP. -

Molecular Characterization of Clinical Isolate of Vibrio Cholerae Isolated from Outbreaks Cases in Malaysia
International Food Research Journal 19 (3): 1267-1274 (2012) Molecular characterization of clinical isolate of Vibrio cholerae isolated from outbreaks cases in Malaysia 1, *Patrick, G. B., 3Nishibuchi, M., 2Tunung, R. and 2Son, R. 1Allied Health Sciences Division, Ministry of Health, Level 2, Block A, Chancery Place Main Building, Jalan Diplomatik 2, Presint Diplomatik, Presint 15, 62050 Putrajaya, Malaysia 2Department of Food Science, Faculty of Food Science and Technology, University Putra Malaysia, 43400 UPM Serdang, Selangor, Malaysia, 3Center for Southeast Asian Studies, Kyoto University, Yoshida, Sakyo-ku, Kyoto 606-8501, Japan Abstract: A total of 32 clinical strains of Vibrio cholerae, including members of the 01 and 0139 serogroup were collected from Klang, Selangor; Penang Island; Samarahan, Sarawak and Miri, Sarawak in Malaysia. In general, all the isolates except the 0139 serotype expressed low resistance to all the antibiotics tested with their Multiple Antibiotic Resistance (MAR) indices ranged from 0.10 to 0.48. The presence of ctx gene that encoded the cholera toxin was confirmed in all these clinical isolates by polymerase chain reaction. The results from the RAPD-PCR were analyzed using the RAPDistance software (Version 1.04). From the dendrogram generated, two main groups were observed which were subdivided into two clusters each. The Selangor’s isolates and the 0139 Penang’s isolates formed one group whereas the Samarahan, Sarawak isolates and the Miri, Sarawak isolates made up the other group, thus delineating their different sources of origin based on their geographical location. Keywords: Vibrio cholerae O1 and O139, outbreak, antibiotic resistance, PCR Introduction its first isolation from the coastal areas of the Bay of Bengal) appeared as large epidemic in India and Cholera is an infectious disease of the Bangladesh. -

Demographic Characteristics and Intravenous Drug Use Among Hepatitis C Patients in the Kota Setar District, Kedah, Malaysia
Epidemiology and Health Volume: 37, Article ID: e2015032, 6 pages Epidemiology and Health http://dx.doi.org/10.4178/epih/e2015032 ORIGINAL ARTICLE Open Access Demographic characteristics and intravenous drug use among hepatitis C patients in the Kota Setar district, Kedah, Malaysia Wei Leong Tan1, Goh Yihui2, Muhammad Radzi Abu Hassan1 1Clinical Research Center, Sultanah Bahiyah Hospital, Kedah; 2Department of Opthalmology, Sultanah Bahiyah Hospital, Kedah, Malaysia OBJECTIVES: This study explored the demographic characteristics of hepatitis C patients in the Kota Setar (KS) district, Kedah, Malaysia, the prevalence of intravenous drug use (IVDU) as a risk factor among these pa- tients, and the associations between IVDU and demographic characteristics. METHODS: Retrospective data pertaining to 713 patients from January 2009 to December 2013 were re- trieved from hospital and disease notification records for analysis. The risk factors for hepatitis C virus (HCV) infection were grouped into IVDU and non-IVDU risk factors for analysis using multiple logistic regression. RESULTS: Of the hepatitis C patients included in this study, the most common age group was 31 to 40 years (30.2%), and male patients (91.2%) made up the overwhelming majority. Ethnic Malays constituted approxi- mately 80.4% of the patients, and IVDU was the main risk factor (77.8%) for HCV infection. Multiple logistic regression showed that male patients were 59 times more likely to have IVDU as a risk factor for HCV infec- tion. Single patients were 2.5 times more likely to have IVDU as a risk factor. Patients aged ≥ 71 years were much less likely than patients aged ≤ 30 years to have IVDU as a risk factor for HCV infection. -

A Case Study in Kedah, Malaysia
Available online at www.sciencedirect.com Procedia - Social and Behavioral Sciences 65 ( 2012 ) 20 – 25 International Congress on Interdisciplinary Business and Social Science (ICIBSoS 2012) A Preference Analysis Model for Selecting Tourist Destinations Based on Motivational Factors: A Case Study in Kedah, Malaysia Daud Mohamada,*, Rozana Mohd Jamilb a,bFaculty of Computer and Mathematical Sciences, Universiti Teknologi MARA, 40450 Shah Alam, Selangor, Malaysia Abstract This paper presents an evaluation of the critical factors influencing local tourists choice of destinations in Kedah and determination of the tourists preference for destinations with respect to these factors using Fuzzy Hierarchical TOPSIS (FHTOPSIS) method. This study focuses on the internal factors that motivate tourists to choose their preference of destination. The result shows the purpose of visiting friends and relatives is the most important factors that motivate their visit to Kedah, while novelty seeking is the least motivating factors influencing the choice of destinations. The best destination to be selected among five destinations under consideration in this study is Langkawi, followed by Alor Setar, Sedim River, Bujang Valley and Bukit Kayu Hitam. This study can assist relevant authorities and travel agencies to plan and promote the places of attraction in Kedah with effective marketing strategies besides assisting tourists to decide where to go to main attractions in Kedah. © 20122012 The Published Authors. by Published Elsevier by Ltd. Elsevier Selection Ltd. and/or peer-review under responsibility of JIBES University, Jakarta Selection and peer-review under responsibility of JIBES University, Jakarta Keywords: Tourism; Tourist destination; Preference analysis; Decision making; Fuzzy hierarchical TOPSIS. 1. Introduction According to the annual report of Tourism Malaysia in 2010 (Tourism Malaysia, 2010), the tourism industry has played a significant role in increasing the GDP where there were 24.6 million tourists arrived of Malaysia with generated revenue of RM56.5 billion. -

Effectiveness of the Colorapp Mobile App for Health Education and Promotion for Colorectal Cancer: Quasi-Experimental Study
JMIR HUMAN FACTORS Yaacob et al Original Paper Effectiveness of the ColorApp Mobile App for Health Education and Promotion for Colorectal Cancer: Quasi-Experimental Study Nor Azwany Yaacob1*, MD, MCM; Muhamad Fadhil Mohamad Marzuki1*, MBBS, MPH, DrPH; Najib Majdi Yaacob2, MD, MPH, DrPH; Shahrul Bariyah Ahmad3, MBBS, MPH; Muhammad Radzi Abu Hassan4, MB BCh BAO, MMed 1Department of Community Medicine, School of Medical Sciences, Universiti Sains Malaysia Health Campus, Kubang Kerian, Kelantan, Malaysia 2Unit of Biostatistics and Research Methodology, School of Medical Sciences, Universiti Sains Malaysia Health Campus, Kubang Kerian, Malaysia 3Non-Communicable Disease Control Unit, Kedah State Health Department, Alor Setar, Kedah, Malaysia 4Clinical Research Centre, Hospital Sultanah Bahiyah, Alor Setar, Kedah, Malaysia *these authors contributed equally Corresponding Author: Nor Azwany Yaacob, MD, MCM Department of Community Medicine School of Medical Sciences Universiti Sains Malaysia Health Campus Universiti Sains Malaysia Kubang Kerian, Kelantan, 16150 Malaysia Phone: 60 9767 6622 ext 6621 Email: [email protected] Abstract Background: Lack of knowledge and poor attitude are barriers to colorectal cancer screening participation. Printed material, such as pamphlets and posters, have been the main approach in health education on disease prevention in Malaysia. Current information technology advancements have led to an increasing trend of the public reading from websites and mobile apps using their mobile phones. Thus, health information dissemination should also be diverted to websites and mobile apps. Increasing knowledge and awareness could increase screening participation and prevent late detection of diseases such as colorectal cancer. Objective: This study aimed to assess the effectiveness of the ColorApp mobile app in improving the knowledge and attitude on colorectal cancer among users aged 50 years and older, who are the population at risk for the disease in Kedah.