What Is Heart Failure?
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Pulmonary Manifestations of Left Heart Failure*
The Pulmonary Manifestations of Left Heart Failure* Brian K. Gehlbach, MD; and Eugene Geppert, MD Determining whether a patient’s symptoms are the result of heart or lung disease requires an understanding of the influence of pulmonary venous hypertension on lung function. Herein, we describe the effects of acute and chronic elevations of pulmonary venous pressure on the mechanical and gas-exchanging properties of the lung. The mechanisms responsible for various symptoms of congestive heart failure are described, and the significance of sleep-disordered breathing in patients with heart disease is considered. While the initial clinical evaluation of patients with dyspnea is imprecise, measurement of B-type natriuretic peptide levels may prove useful in this setting. (CHEST 2004; 125:669–682) Key words: Cheyne-Stokes respiration; congestive heart failure; differential diagnosis; dyspnea; pulmonary edema; respiratory function tests; sleep apnea syndromes Abbreviations: CHF ϭ congestive heart failure; CSR-CSA ϭ Cheyne-Stokes respiration with central sleep apnea; CPAP ϭ continuous positive airway pressure; Dlco ϭ diffusing capacity of the lung for carbon monoxide; DM ϭ membrane conductance; FRC ϭ functional residual capacity; OSA ϭ obstructive sleep apnea; TLC ϭ total lung ϭ ˙ ˙ ϭ capacity; VC capillary volume; Ve/Vco2 ventilatory equivalent for carbon dioxide early 5 million Americans have congestive heart For a detailed review of the pathophysiology of N failure (CHF), with 400,000 new cases diag- high-pressure pulmonary edema, the reader is re- nosed each year.1 Unfortunately, despite the consid- ferred to several excellent recent reviews.2–4 erable progress that has been made in understanding the pathophysiology of pulmonary edema, the pul- monary complications of this condition continue to The Pathophysiology of Pulmonary challenge the bedside clinician. -

Your Pulse and Target Heart Rate
Skip to main content ×Close Menu We use cookies to improve your experience on our website. By closing this banner or interacting with our site, you acknowledge and agree to this. Legal Notices MobileClose Menu Find A Doctor Your Visit Pay a Bill Log in to MyGillette Learn more about MyGillette Patient Education Patient Services and Resources Your Rights and Medical Records Understanding Costs, Insurance and the Gillette Assistance Programs Services to Support Your Family Interpreter Services International Patients Parent Resources and Support Prepare for Your Visit Prepare for Clinic Visits and Tests Prepare for Surgery Take a Hospital Tour Transfer Your Medical Records Transportation and Accommodations Ways to Prepare and Comfort Your Child During Your Visit or Hospital Stay Commitment to a Safe and Healing Environment Our Hospital Units Your Hospital Room St. Paul Campus Amenities and Activities Visit or Contact a Patient Conditions & Care All Conditions Cerebral Palsy Neuromuscular Disorders Scoliosis Craniosynostosis Brain Injury All Tests & Treatments Shunt Surgery for Hydrocephalus Gait and Motion Analysis Selective Dorsal Rhizotomy (SDR) Gillette Craniocap© Orthosis Botulinum Toxin and Phenol (Injected Spasticity Medications) All Specialties & Services Orthopedics Rehabilitation Services Craniofacial and Plastic Surgery Neurology Neurosurgery Virtual Visits Pediatric Expert Consults Virtual Rehab Therapy Sleep Medicine Virtual Care Get Involved Advocating for Your Family Community Health United Cerebral Palsy of MN Donors & Supporters -

The Heart Institute
The Heart Institute Division of Cardiology 4650 Sunset Blvd., #34, Los Angeles, CA 90027 Phone: 323-361-2461 Fax: 323-361-1513 The Heart Institute at Children’s Hospital Los Angeles is CHLA.org/CARDIOLOGY one of the top-ranked pediatric heart programs in the Division of nation—with a long history of exceptional and innovative Cardiothoracic Surgery 4650 Sunset Blvd., #66 care for the most complex pediatric cardiac conditions. Los Angeles, CA 90027 Phone: 323-361-4148 Fax: 323-361-3668 We treat patients from fetus to adulthood and serve as CHLA.org/CTSurgery a major tertiary referral center for all forms of congenital Referrals Phone: 888-631-2452 and acquired heart disease. Fax: 323-361-8988 Email: [email protected] Physician Portal: https://myCHLA.CHLA.org We offer an integrated inpatient and outpatient Our Cardiothoracic Intensive Care Unit (CTICU) complement of services that brings together experts was the first of its kind on the West Coast, using in cardiology, cardiothoracic surgery, cardiothoracic innovative treatments including extracorporeal transplant, cardiothoracic intensive care and membrane oxygenation (ECMO) and ventricular cardiovascular acute care in a centrally located, assist services. state-of-the-art healing environment. With fewer steps to navigate, our patients and families receive care Our two state-of-the-art catheterization laboratories that is more streamlined and less stressful. use the latest technology to provide accurate cardiac data while reducing radiation. Our programmatic emphasis on high-complexity surgeries in neonates has produced outcomes that are among the best in the country, as shown in the most recent Society of Thoracic Surgeons report. -

Percutaneous Mitral Valve Therapies: State of the Art in 2020 LA ACP Annual Meeting
Percutaneous Mitral Valve Therapies: State of the Art in 2020 LA ACP Annual Meeting Steven R Bailey MD MSCAI, FACC, FAHA,FACP Professor and Chair, Department of Medicine Malcolm Feist Chair of Interventional Cardiology LSU Health Shreveport Professor Emeritus, UH Health San Antonio [email protected] SRB March 2020 Disclosure Statement of Financial Interest Within the past 12 months, I or my spouse/partner have had a financial interest/arrangement or affiliation with the organization(s) listed below. Affiliation/Financial Relationship Company • Grant/Research Support • None • Consulting Fees/Honoraria • BSCI, Abbot DSMB • Intellectual Property Rights • UTHSCSA • Other Financial Benefit • CCI Editor In Chief SRB March 2020 The 30,000 Ft View Maria SRB March 2020 SRB March 2020 Mitral Stenosis • The most common etiology of MS is rheumatic fever, with a latency of approximately 10 to 20 years after the initial streptococcal infection. Symptoms usually appear in adulthood • Other etiologies are rare but include: congenital MS radiation exposure atrial myxoma mucopolysaccharidoses • MS secondary to calcific annular disease is increasingly seen in elderly patients, and in patients with advanced chronic kidney disease. SRB March 2020 Mitral Stenosis • Mitral stenosis most commonly results from rheumatic heart disease fusion of the valve leaflet cusps at the commissures thickening and shortening of the chordae calcium deposition within the valve leaflets • Characteristic “fish-mouth” or “hockey stick” appearance on the echocardiogram (depending on view) SRB March 2020 Mitral Stenosis: Natural History • The severity of symptoms depends primarily on the degree of stenosis. • Symptoms often go unrecognized by patient and physician until significant shortness of breath, hemoptysis, or atrial fibrillation develops. -
Currentstateofknowledgeonaetiol
European Heart Journal (2013) 34, 2636–2648 ESC REPORT doi:10.1093/eurheartj/eht210 Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: a position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases Downloaded from Alida L. P. Caforio1†*, Sabine Pankuweit2†, Eloisa Arbustini3, Cristina Basso4, Juan Gimeno-Blanes5,StephanB.Felix6,MichaelFu7,TiinaHelio¨ 8, Stephane Heymans9, http://eurheartj.oxfordjournals.org/ Roland Jahns10,KarinKlingel11, Ales Linhart12, Bernhard Maisch2, William McKenna13, Jens Mogensen14, Yigal M. Pinto15,ArsenRistic16, Heinz-Peter Schultheiss17, Hubert Seggewiss18, Luigi Tavazzi19,GaetanoThiene4,AliYilmaz20, Philippe Charron21,andPerryM.Elliott13 1Division of Cardiology, Department of Cardiological Thoracic and Vascular Sciences, University of Padua, Padova, Italy; 2Universita¨tsklinikum Gießen und Marburg GmbH, Standort Marburg, Klinik fu¨r Kardiologie, Marburg, Germany; 3Academic Hospital IRCCS Foundation Policlinico, San Matteo, Pavia, Italy; 4Cardiovascular Pathology, Department of Cardiological Thoracic and Vascular Sciences, University of Padua, Padova, Italy; 5Servicio de Cardiologia, Hospital U. Virgen de Arrixaca Ctra. Murcia-Cartagena s/n, El Palmar, Spain; 6Medizinische Klinik B, University of Greifswald, Greifswald, Germany; 7Department of Medicine, Heart Failure Unit, Sahlgrenska Hospital, University of Go¨teborg, Go¨teborg, Sweden; 8Division of Cardiology, Helsinki University Central Hospital, Heart & Lung Centre, -
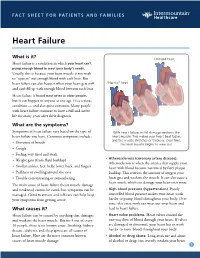
Heart Failure
FACT SHEET FOR PATIENTS AND FAMILIES Heart Failure What is it? Enlarged heart Heart failure is a condition in which your heart can’t pump enough blood to meet your body’s needs. Usually, this is because your heart muscle is too weak to “squeeze” out enough blood with each beat. But heart failure can also happen when your heart gets stiff “Normal” heart and can’t fill up with enough blood between each beat. Heart failure is found most often in older people, but it can happen to anyone at any age. It’s a serious condition — and also quite common. Many people with heart failure continue to have a full and active life for many years after their diagnosis. What are the symptoms? Symptoms of heart failure vary based on the type of With heart failure, initial damage weakens the heart failure you have. Common symptoms include: heart muscle. This makes your heart beat faster, and the muscle stretches or thickens. Over time, • Shortness of breath the heart muscle begins to wear out. • Cough • Feeling very tired and weak • Atherosclerosis (coronary artery disease). • Weight gain (from fluid buildup) Atherosclerosis is when the arteries that supply your • Swollen ankles, feet, belly, lower back, and fingers heart with blood become narrowed by fatty plaque • Puffiness or swelling around the eyes buildup. This restricts the amount of oxygen your • Trouble concentrating or remembering heart gets and weakens the muscle. It can also cause a heart attack, which can damage your heart even more. The main cause of heart failure (heart muscle damage and weakness) cannot be cured, but symptoms can be • High blood pressure (hypertension). -

Heart Disease and Diseases of the Circulatory System in Westchester
Westchester County 2016.01 Department of Health KEEP HEALTHY @wchealthdept AND Community Health Assessment Data Update GET #keephealthy THE STATS Heart Disease and Diseases of the Circulatory System in Westchester In this issue: Heart disease as a Heart disease is the number one cause of death in Westchester County. leading cause of death in Westchester county In 2012, heart disease accounted for 2,113 deaths or 31% of all deaths Deaths due to heart disease across different in the county. Adding in 490 deaths due to stroke and other diseases population and risk of the circulatory system, total deaths from circulatory disease are groups 60% higher than the next leading cause of death - cancer. Hospitalizations due to cardiovascular disease- related conditions, Selected Causes of Death in Westchester County, 2012 including diseases of the heart Emergency room visits 2% 3% 7% due to cardiovascular disease-related 3% conditions Selected risk factors 4% that contribute to Heart Disease, cardiovascular disease 4% in Westchester county 31% 5% 9% Cerebrovascular Jiali Li, Ph.D. Director of Disease (Stroke), Research & Evaluation Neoplasms 5% Planning & Evaluation (Cancer), 24% Other Circulatory, Renee Recchia, MPH 3% Acting Deputy Commissioner of Administration Heart Disease Cerebrovascular Disease (Stroke) Project Staff: Other Circulatory Neoplasms (Cancer) Bonnie Lam, MPH Respiratory Diseases External Causes (e.g. accidents) Medical Data Analyst Communicable Diseases Nervous System Diseases Milagros Venuti, MPA Digestive System Diseases -

Grade 6: the Heart and Circulatory System Lesson 1: the Heart Lesson 2: the Heart Rate Lesson 3: the Circulatory System and Blood
Grade 6: The Heart and Circulatory System Lesson 1: The Heart Lesson 2: The Heart Rate Lesson 3: The Circulatory System and Blood Objectives: 1. Students will identify the four chambers of the heart 2. Students will identify four important structures of the Circulatory System and what they do. 3. Students will explain heart rate and be able to take their resting and active heart rates. 4. Students will describe the major functions of the Circulatory System. 5. Students will explain the role of the heart in circulation 6. Students will give a basic explanation of the cardio-pulmonary sequence. 7. Students will describe systemic circulation. Materials: Lesson 1: • Animal heart (Example: cow, pig, sheep) • Note cards • Picture of the heart (See Figure 1) • Dissection tools (Scissors, pan, etc.) Lesson 2: • Small drum • Watch or clock with second hand, or time • Optional: Stethoscope Lesson 3: • Corn Syrup • Plastic Beads: flat red disks, white ovals, green or blue seed beads • “Explain” experiment (per group): o Two small balloons or large finger cots o One clear tube (1/2” diameter) about 8” long o One clear tube (3/4” diameter) about 8” long o 16 - 20 oz. water o Red food coloring o Measuring cup o Funnel o Two empty plastic containers (such as cottage cheese or yogurt cartons) Activity Summary: In this lesson students will learn the basic functioning of the heart, Circulatory System and blood, the connection to lung functioning, and the activity of the Grade 6: The Heart & Circulatory System – Revised 2008 Page 1 Circulatory System in the body. -

Basic Cardiac Rhythms – Identification and Response Module 1 ANATOMY, PHYSIOLOGY, & ELECTRICAL CONDUCTION Objectives
Basic Cardiac Rhythms – Identification and Response Module 1 ANATOMY, PHYSIOLOGY, & ELECTRICAL CONDUCTION Objectives ▪ Describe the normal cardiac anatomy and physiology and normal electrical conduction through the heart. ▪ Identify and relate waveforms to the cardiac cycle. Cardiac Anatomy ▪ 2 upper chambers ▪ Right and left atria ▪ 2 lower chambers ▪ Right and left ventricle ▪ 2 Atrioventricular valves (Mitral & Tricuspid) ▪ Open with ventricular diastole ▪ Close with ventricular systole ▪ 2 Semilunar Valves (Aortic & Pulmonic) ▪ Open with ventricular systole ▪ Open with ventricular diastole The Cardiovascular System ▪ Pulmonary Circulation ▪ Unoxygenated – right side of the heart ▪ Systemic Circulation ▪ Oxygenated – left side of the heart Anatomy Coronary Arteries How The Heart Works Anatomy Coronary Arteries ▪ 2 major vessels of the coronary circulation ▪ Left main coronary artery ▪ Left anterior descending and circumflex branches ▪ Right main coronary artery ▪ The left and right coronary arteries originate at the base of the aorta from openings called the coronary ostia behind the aortic valve leaflets. Physiology Blood Flow Unoxygenated blood flows from inferior and superior vena cava Right Atrium Tricuspid Valve Right Ventricle Pulmonic Valve Lungs Through Pulmonary system Physiology Blood Flow Oxygenated blood flows from the pulmonary veins Left Atrium Mitral Valve Left Ventricle Aortic Valve Systemic Circulation ▪ Blood Flow Through The Heart ▪ Cardiology Rap Physiology ▪ Cardiac cycle ▪ Represents the actual time sequence between -

682.Full.Pdf
Endogenous and nitrovasodilator-induced release of NO in the airways of end-stage cystic fibrosis patients To the Editors: blood pressure changes recorded, as described previously [8] and in the online supplementary material. A variety of isoforms of nitric oxide (NO) synthases are constitutively expressed in human airway and vascular Nearly undetectable levels of NO were found in CF patients endothelial cells continuously generating NO. NO plays an representing an output of 7.6¡6 ppb over 30 s. This is in important role in regulating lung function in health and contrast to patients presented for routine open heart surgery disease including modulation of pulmonary vascular resis- (91.4¡21 ppb over 30 s; fig. 1). Representative traces are tance, airway calibre and host defence. Production of NO and shown in figure 1A and C of the online supplementary its consumption by fluid-phase reactions can be detected and material. monitored in the exhaled air, providing an important window There was a significant increase in gas-phase NO above baseline to assess the dynamics of NO metabolism in health and levels by 250 mg GTN boluses in CF patients (36.7¡6ppb), inflammatory lung conditions, asthma in particular [1]. which was comparable to that seen in control patients with A series of milestone studies uncovered a relative deficiency of routine open heart surgery (48.7¡4 ppb; fig. 1). Representative pulmonary NO availability in cystic fibrosis (CF), a severe traces of GTN-induced exhaled NO are presented in figure 1B chronic inflammatory lung disease with studies generally and D of the online supplementary material. -

KNOW the FACTS ABOUT Heart Disease
KNOW THE FACTS ABOUT Heart Disease What is heart disease? Having high cholesterol, high blood pressure, or diabetes also can increase Heart disease is the leading cause of your risk for heart disease. Ask your death in the United States. More than doctor about preventing or treating these 600,000 Americans die of heart disease medical conditions. each year. That’s one in every four deaths in this country.1 What are the signs and symptoms? The term “heart disease” refers to several The symptoms vary depending on the types of heart conditions. The most type of heart disease. For many people, common type is coronary artery disease, chest discomfort or a heart attack is the which can cause heart attack. Other first sign. kinds of heart disease may involve the Someone having a heart attack may valves in the heart, or the heart may not experience several symptoms, including: pump well and cause heart failure. Some people are born with heart disease. l Chest pain or discomfort that doesn’t go away after a few minutes. l Pain or discomfort in the jaw, neck, Are you at risk? or back. Anyone, including children, can l Weakness, light-headedness, nausea develop heart disease. It occurs when (feeling sick to your stomach), or a substance called plaque builds up in a cold sweat. your arteries. When this happens, your arteries can narrow over time, reducing l Pain or discomfort in the arms blood flow to the heart. or shoulder. Smoking, eating an unhealthy diet, and l Shortness of breath. not getting enough exercise all increase If you think that you or someone you your risk for having heart disease. -

Cardiovascular Disease: a Costly Burden for America. Projections
CARDIOVASCULAR DISEASE: A COSTLY BURDEN FOR AMERICA PROJECTIONS THROUGH 2035 CARDIOVASCULAR DISEASE: A COSTLY BURDEN FOR AMERICA — PROJECTIONS THROUGH 2035 american heart association CVD Burden Report CVD Burden association heart american table of contents INTRODUCTION ...................................................................................5 ABOUT THIS STUDY ................................................................................................... 6 WHAT IS CVD? ......................................................................................................... 6 Atrial Fibrillation Congestive Heart Failure Coronary Heart Disease High Blood Pressure Stroke PROJECTIONS: PREVALENCE OF CVD .............................................................7 Latest Projections Age, Race, Sex – Differences That Matter PROJECTIONS: COSTS OF CVD ................................................................. 8-11 The Cost Generators: Aging Baby Boomers Medical Costs Breakdown Direct Costs + Indirect Costs RECOMMENDATIONS .............................................................................13-14 Research Prevention Affordable Health Care 3 CARDIOVASCULAR DISEASE: A COSTLY BURDEN FOR AMERICA — PROJECTIONS THROUGH 2035 american heart association CVD Burden Report CVD Burden association heart american Introduction Cardiovascular disease (CVD) has been the leading killer In addition, CVD has become our nation’s costliest chronic of Americans for decades. In years past, a heart attack disease. In 2014, stroke and heart