Headache Caused by Sinus Disease
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

MR Imaging of the Orbital Apex
J Korean Radiol Soc 2000;4 :26 9-0 6 1 6 MR Imaging of the Orbital Apex: An a to m y and Pat h o l o g y 1 Ho Kyu Lee, M.D., Chang Jin Kim, M.D.2, Hyosook Ahn, M.D.3, Ji Hoon Shin, M.D., Choong Gon Choi, M.D., Dae Chul Suh, M.D. The apex of the orbit is basically formed by the optic canal, the superior orbital fis- su r e , and their contents. Space-occupying lesions in this area can result in clinical d- eficits caused by compression of the optic nerve or extraocular muscles. Even vas c u l a r changes in the cavernous sinus can produce a direct mass effect and affect the orbit ap e x. When pathologic changes in this region is suspected, contrast-enhanced MR imaging with fat saturation is very useful. According to the anatomic regions from which the lesions arise, they can be classi- fied as belonging to one of five groups; lesions of the optic nerve-sheath complex, of the conal and intraconal spaces, of the extraconal space and bony orbit, of the cav- ernous sinus or diffuse. The characteristic MR findings of various orbital lesions will be described in this paper. Index words : Orbit, diseases Orbit, MR The apex of the orbit is a complex region which con- tains many nerves, vessels, soft tissues, and bony struc- Anatomy of the orbital apex tures such as the superior orbital fissure and the optic canal (1-3), and is likely to be involved in various dis- The orbital apex region consists of the optic nerve- eases (3). -
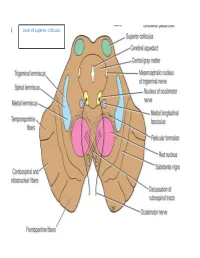
Level of Superior Colliculus ° Edinger- Westphal Nucleus ° Pretectal Nucleus: Close to the Lateral Part of the Superior Colliculus
Level of superior colliculus ° Edinger- Westphal nucleus ° pretectal nucleus: close to the lateral part of the superior colliculus. Red nucleus • Rounded mass of gray matter • Situated bt cerebral aqueduct and substantia nigra • Reddish blue(vascularity & iron containing pigment) • Afferents from: cerebral cortex,cerebellum,substa ntia nigra, thalamic nuclei, spinal cord • Efferent to: spinal cord, reticular formation. thalamus and substantia nigra • involved in motor coordination. Crus cerebri • Corticospinal & corticonuclear fibers (middle) • Frontopontine fibers (medial) • Temporopontine fibers (lateral) these descending tracts connect the cerebral cortex with spinal cord, cranial nerves nuclei, pons & cerebellum Level at superior colliculus ° Superior colliculus ° Occulomotor nucleus (posterior to MLF) ° Occulomotor n emerges through red nucleus ° Edinger-Westphal nucleus ° pretectal nucleus: close to the lateral part of the superior colliculus. ° MLF ° Medial , trigeminal, spinal leminiscus ( no lateral leminiscus) ° Red nucleus ° Substantia nigra ° Crus cerebri ° RF Substantia nigra ° Large motor nucleus ° is a brain structure located in the midbrain ° plays an important role in reward, addiction, and movement. ° Substantia nigra is Latin for "black substance" due to high levels of melanin ° has connections with basal ganglia ,cerebral cortex ° Concerned with muscle tone ° Parkinson's disease is caused by the death of neurons in the substantia nigra Oculomotor Nerve (III) • Main oculomotor nucleus • Accessory parasympathetic nucleus -

Palatal Injection Does Not Block the Superior Alveolar Nerve Trunks: Correcting an Error Regarding the Innervation of the Maxillary Teeth
Open Access Review Article DOI: 10.7759/cureus.2120 Palatal Injection does not Block the Superior Alveolar Nerve Trunks: Correcting an Error Regarding the Innervation of the Maxillary Teeth Joe Iwanaga 1 , R. Shane Tubbs 2 1. Seattle Science Foundation 2. Neurosurgery, Seattle Science Foundation Corresponding author: Joe Iwanaga, [email protected] Abstract The superior alveolar nerves course lateral to the maxillary sinus and the greater palatine nerve travels through the hard palate. This difficult three-dimensional anatomy has led some dentists and oral surgeons to a critical misunderstanding in developing the anterior and middle superior alveolar (AMSA) nerve block and the palatal approach anterior superior alveolar (P-ASA) nerve block. In this review, the anatomy of the posterior, middle and anterior superior alveolar nerves, greater palatine nerve, and nasopalatine nerve are revisited in order to clarify the anatomy of these blocks so that the perpetuated anatomical misunderstanding is rectified. We conclude that the AMSA and P-ASA nerve blockades, as currently described, are not based on accurate anatomy. Categories: Anesthesiology, Medical Education, Other Keywords: anatomy, innervation, local anesthesia, maxillary nerve, nerve block, tooth Introduction And Background Anesthetic blockade of the posterior superior alveolar (PSA) branch of the maxillary nerve has played an important role in the endodontic treatment of irreversible acute pulpitis of the upper molar teeth except for the mesiobuccal root of the first molar tooth [1, 2]. This procedure requires precise anatomical knowledge of the pterygopalatine fossa and related structures in order to avoid unnecessary complications and to make the blockade most effective. The infraorbital nerve gives rise to middle superior alveolar (MSA) and anterior superior alveolar (ASA) branches. -

Nerves of the Orbit Optic Nerve the Optic Nerve Enters the Orbit from the Middle Cranial Fossa by Passing Through the Optic Canal
human anatomy 2016 lecture fourteen Dr meethak ali ahmed neurosurgeon Nerves of the Orbit Optic Nerve The optic nerve enters the orbit from the middle cranial fossa by passing through the optic canal . It is accompanied by the ophthalmic artery, which lies on its lower lateral side. The nerve is surrounded by sheath of pia mater, arachnoid mater, and dura mater. It runs forward and laterally within the cone of the recti muscles and pierces the sclera at a point medial to the posterior pole of the eyeball. Here, the meninges fuse with the sclera so that the subarachnoid space with its contained cerebrospinal fluid extends forward from the middle cranial fossa, around the optic nerve, and through the optic canal, as far as the eyeball. A rise in pressure of the cerebrospinal fluid within the cranial cavity therefore is transmitted to theback of the eyeball. Lacrimal Nerve The lacrimal nerve arises from the ophthalmic division of the trigeminal nerve. It enters the orbit through the upper part of the superior orbital fissure and passes forward along the upper border of the lateral rectus muscle . It is joined by a branch of the zygomaticotemporal nerve, whi(parasympathetic secretomotor fibers). The lacrimal nerve ends by supplying the skin of the lateral part of the upper lid. Frontal Nerve The frontal nerve arises from the ophthalmic division of the trigeminal nerve. It enters the orbit through the upper part of the superior orbital fissure and passes forward on the upper surface of the levator palpebrae superioris beneath the roof of the orbit . -

Regional Anesthesia in Head and Neck Surgery
TITLE: Regional Anesthesia in Head and Neck Surger SOURCE: Grand Rounds Presentation, UTMB, Dept. of Otolaryngology DATE: May 24, 2006 RESIDENT PHYSICIAN: Jacques Peltier, MD FACULTY PHYSICIAN: Francis B. Quinn, MD SERIES EDITORS: Francis B. Quinn, Jr., MD and Matthew W. Ryan, MD "This material was prepared by resident physicians in partial fulfillment of educational requirements established for the Postgraduate Training Program of the UTMB Department of Otolaryngology/Head and Neck Surgery and was not intended for clinical use in its present form. It was prepared for the purpose of stimulating group discussion in a conference setting. No warranties, either express or implied, are made with respect to its accuracy, completeness, or timeliness. The material does not necessarily reflect the current or past opinions of members of the UTMB faculty and should not be used for purposes of diagnosis or treatment without consulting appropriate literature sources and informed professional opinion." Introduction Local anesthetic techniques were popularized early in the history of surgery with the advent of injectable nerve blocking agents. Until their discovery, patients were either held down or knocked unconscious to perform procedures. In the early days of general anesthesia, local anesthesia was preferred in all cases that it was applicable due to the significant risks associated with general anesthesia. Many procedures performed today under general anesthesia, such as tonsillectomy, rhinoplasty, and even bronchoscopy, were performed under local anesthesia to avoid the perils of general anesthetics. With the introduction of pulse oximetry, safer inhaled anesthetics, and combined intravenous and inhaled general anesthesia techniques, general anesthesia has become much safer, resulting in many surgeons being unfamiliar with regional nerve blocks to perform surgery. -

Maxillary Nerve-Mediated Postseptoplasty Nasal Allodynia: a Case Report
E CASE REPORT Maxillary Nerve-Mediated Postseptoplasty Nasal Allodynia: A Case Report Shikha Sharma, MD, PhD,* Wilson Ly, MD, PharmD,* and Xiaobing Yu, MD*† Endoscopic nasal septoplasty is a commonly performed otolaryngology procedure, not known to cause persistent postsurgical pain or hypersensitivity. Here, we discuss a unique case of persis- tent nasal pain that developed after a primary endoscopic septoplasty, which then progressed to marked mechanical and thermal allodynia following a revision septoplasty. Pain symptoms were found to be mediated by the maxillary division of the trigeminal nerve and resolved after percuta- neous radiofrequency ablation (RFA) of bilateral maxillary nerves. To the best of our knowledge, this is the first report of maxillary nerve–mediated nasal allodynia after septoplasty. (A&A Practice. 2020;14:e01356.) GLOSSARY CT = computed tomography; FR = foramen rotundum; HIPAA = Health Insurance Portability and Accountability Act; ION = infraorbital nerve; LPP = lateral pterygoid plate; MRI = magnetic reso- nance imaging; RFA = radiofrequency ablation; SPG = sphenopalatine ganglion; US = ultrasound ndoscopic nasal septoplasty is a common otolaryn- septoplasty for chronic nasal obstruction with resection of gology procedure with rare incidence of postsurgical the cartilage inferiorly and posteriorly in 2010. Before this Ecomplications. Minor complications include epistaxis, surgery, the patient only occasionally experienced mild septal hematoma, septal perforation, cerebrospinal fluid leak, headaches. However, his postoperative course was compli- and persistent obstruction.1 Numbness or hypoesthesia of the cated by significant pain requiring high-dose opioids. After anterior palate, secondary to injury to the nasopalatine nerve, discharge, patient continued to have persistent deep, “ach- has been reported, but is usually rare and temporary, resolv- ing” nasal pain which radiated toward bilateral forehead ing over weeks to months.2 Acute postoperative pain is also and incisors. -

Simple Ways to Dissect Ciliary Ganglion for Orbital Anatomical Education
OkajimasDetection Folia Anat. of ciliary Jpn., ganglion94(3): 119–124, for orbit November, anatomy 2017119 Simple ways to dissect ciliary ganglion for orbital anatomical education By Ming ZHOU, Ryoji SUZUKI, Hideo AKASHI, Akimitsu ISHIZAWA, Yoshinori KANATSU, Kodai FUNAKOSHI, Hiroshi ABE Department of Anatomy, Akita University Graduate School of Medicine, Akita, 010-8543 Japan –Received for Publication, September 21, 2017– Key Words: ciliary ganglion, orbit, human anatomy, anatomical education Summary: In the case of anatomical dissection as part of medical education, it is difficult for medical students to find the ciliary ganglion (CG) since it is small and located deeply in the orbit between the optic nerve and the lateral rectus muscle and embedded in the orbital fat. Here, we would like to introduce simple ways to find the CG by 1): tracing the sensory and parasympathetic roots to find the CG from the superior direction above the orbit, 2): transecting and retracting the lateral rectus muscle to visualize the CG from the lateral direction of the orbit, and 3): taking out whole orbital structures first and dissecting to observe the CG. The advantages and disadvantages of these methods are discussed from the standpoint of decreased laboratory time and students as beginners at orbital anatomy. Introduction dissection course for the first time and with limited time. In addition, there are few clear pictures in anatomical The ciliary ganglion (CG) is one of the four para- textbooks showing the morphology of the CG. There are sympathetic ganglia in the head and neck region located some scientific articles concerning how to visualize the behind the eyeball between the optic nerve and the lateral CG, but they are mostly based on the clinical approaches rectus muscle in the apex of the orbit (Siessere et al., rather than based on the anatomical procedure for medical 2008). -

Morfofunctional Structure of the Skull
N.L. Svintsytska V.H. Hryn Morfofunctional structure of the skull Study guide Poltava 2016 Ministry of Public Health of Ukraine Public Institution «Central Methodological Office for Higher Medical Education of MPH of Ukraine» Higher State Educational Establishment of Ukraine «Ukranian Medical Stomatological Academy» N.L. Svintsytska, V.H. Hryn Morfofunctional structure of the skull Study guide Poltava 2016 2 LBC 28.706 UDC 611.714/716 S 24 «Recommended by the Ministry of Health of Ukraine as textbook for English- speaking students of higher educational institutions of the MPH of Ukraine» (minutes of the meeting of the Commission for the organization of training and methodical literature for the persons enrolled in higher medical (pharmaceutical) educational establishments of postgraduate education MPH of Ukraine, from 02.06.2016 №2). Letter of the MPH of Ukraine of 11.07.2016 № 08.01-30/17321 Composed by: N.L. Svintsytska, Associate Professor at the Department of Human Anatomy of Higher State Educational Establishment of Ukraine «Ukrainian Medical Stomatological Academy», PhD in Medicine, Associate Professor V.H. Hryn, Associate Professor at the Department of Human Anatomy of Higher State Educational Establishment of Ukraine «Ukrainian Medical Stomatological Academy», PhD in Medicine, Associate Professor This textbook is intended for undergraduate, postgraduate students and continuing education of health care professionals in a variety of clinical disciplines (medicine, pediatrics, dentistry) as it includes the basic concepts of human anatomy of the skull in adults and newborns. Rewiewed by: O.M. Slobodian, Head of the Department of Anatomy, Topographic Anatomy and Operative Surgery of Higher State Educational Establishment of Ukraine «Bukovinian State Medical University», Doctor of Medical Sciences, Professor M.V. -

Osteoma of Internal Auditory Canal - a Rare Pathology
Jemds.com Case Report Osteoma of Internal Auditory Canal - A Rare Pathology Bhushita Nilesh Guru1, Bhushan Narayan Lakhkar2 1Department of Radiology, Datta Meghe Institute of Medical Sciences, Sawangi (Meghe), Wardha, Maharashtra, India. 2Department of Radiology, Datta Meghe Institute of Medical Sciences, Sawangi (Meghe), Wardha, Maharashtra, India. PRESENTATION OF CASE A 27-year-old female patient visited the Department of Radiology with complaints of Corresponding Author: right sided facial palsy and sensory-neural hearing loss from past 10 years. Otologic Dr. Bhushita Nilesh Guru, examination revealed both tympanic membranes to be normal. Audiometry revealed Associate Professor, Datta Meghe Institute of right sided sensory neural hearing loss. The patient was also having multiple facial Medical Sciences, Sawangi (M), spasms. Wardha, Maharashtra, India. HRCT temporal bone of the patient was done, and it showed a well-defined round E-mail: [email protected] to oval bony out-pouching arising from posterior wall of right internal auditory canal causing severe stenosis of porus acusticus with only 7 mm patency. (Figure 1) The DOI: 10.14260/jemds/2020/625 lesion was noted to be over the vestibulo-cochlear and the facial nerves. The cortex of the lesion was continuous with that of the parent bone. (Figure 2). The left internal How to Cite This Article: auditory canal was normal. Guru BN, Lakhkar BN. Osteoma of internal auditory canal: a rare pathology. J Evolution Med Dent Sci 2020;9(38):2863- 2864, DOI: 10.14260/jemds/2020/625 DISCUSSION Submission 19-06-2020, Peer Review 13-08-2020, Osteomas are one of the common benign bone pathologies. -

Surgical Anatamic of Paranasal Sinuses
SURGICAL ANATAMIC OF PARANASAL SINUSES DR. SEEMA MONGA ASSOCIATE PROFESSOR DEPARTMENT OF ENT-HNS HIMSR MIDDLE TURBINATE 1. Anterior attachment : vertically oriented, sup to the lateral border of cribriform plate. 2. Second attachment :Obliquely oriented- basal lamella/ ground lamella, Attached to the lamina papyracea ( medial wall of orbit anterior, posterior air cells, sphenopala‐ tine foramen 3. Posterior attachment :medial wall of maxillary sinus, horizontally oriented. , supreme turbinate 3. Occasionally 4. fourth turbinate, 5. supreme meatus, if present 6. drains posterior ethmoid drains inferior, middle, superior turbinates and, occasionally, the supreme turbinate, the fourth turbinate. e. Lateral to these turbinates are the corresponding meatuses divided per their drainage systems ANATOMICAL VARIATIONS OF THE TURBINATES 1. Concha bullosa, 24–55%, often bilateral, 2. Interlamellar cell of grunwald: pneumatization is limited to the vertical part of middle turbinate, usually not causing narrowing of the ostiomeatal unit 3. Paradoxic middle turbinate: 26%,. Occasionally, it can affect the patency of the ostiomeatal unit 4. Pneumatized basal lamella, falsely considered, posterior ethmoid air cell Missed basal lamella – attaches to lateral maxillary sinus wall Ostiomeatal unit Anterior ostiomeatal unit, maxillary, anterior ethmoid, frontal sinuses, (1) ethmoid infundibulum, (2) middle meatus, (3) hiatus semilunaris, (4) maxillaryOstium, (5) ethmoid bulla, (6) frontal recess, (7) uncinate process. , sphenoethmoidal recess Other draining osteomeatal unit, posterior in the nasal cavity, posterior ethmoid sinus, lateral to the superior turbinate, . sphenoid Sinus medial to the superior turbinate Uncinate Process Crescent‐shaped, thin individual bone inferiorly- ethmoidal process of inferior turbinate, anterior, lacrimal bone, posteriorly- hiatus Semilunaris, medial -ethmoid infundibulum, laterally, middle meatus superior attachment- variability, direct effect on frontal sinus drainage pathway. -

98796-Anatomy of the Orbit
Anatomy of the orbit Prof. Pia C Sundgren MD, PhD Department of Diagnostic Radiology, Clinical Sciences, Lund University, Sweden Lund University / Faculty of Medicine / Inst. Clinical Sciences / Radiology / ECNR Dubrovnik / Oct 2018 Lund University / Faculty of Medicine / Inst. Clinical Sciences / Radiology / ECNR Dubrovnik / Oct 2018 Lay-out • brief overview of the basic anatomy of the orbit and its structures • the orbit is a complicated structure due to its embryological composition • high number of entities, and diseases due to its composition of ectoderm, surface ectoderm and mesoderm Recommend you to read for more details Lund University / Faculty of Medicine / Inst. Clinical Sciences / Radiology / ECNR Dubrovnik / Oct 2018 Lund University / Faculty of Medicine / Inst. Clinical Sciences / Radiology / ECNR Dubrovnik / Oct 2018 3 x 3 Imaging technique 3 layers: - neuroectoderm (retina, iris, optic nerve) - surface ectoderm (lens) • CT and / or MR - mesoderm (vascular structures, sclera, choroid) •IOM plane 3 spaces: - pre-septal •thin slices extraconal - post-septal • axial and coronal projections intraconal • CT: soft tissue and bone windows 3 motor nerves: - occulomotor (III) • MR: T1 pre and post, T2, STIR, fat suppression, DWI (?) - trochlear (IV) - abducens (VI) Lund University / Faculty of Medicine / Inst. Clinical Sciences / Radiology / ECNR Dubrovnik / Oct 2018 Lund University / Faculty of Medicine / Inst. Clinical Sciences / Radiology / ECNR Dubrovnik / Oct 2018 Superior orbital fissure • cranial nerves (CN) III, IV, and VI • lacrimal nerve • frontal nerve • nasociliary nerve • orbital branch of middle meningeal artery • recurrent branch of lacrimal artery • superior orbital vein • superior ophthalmic vein Lund University / Faculty of Medicine / Inst. Clinical Sciences / Radiology / ECNR Dubrovnik / Oct 2018 Lund University / Faculty of Medicine / Inst. -

Cranial Neuralgias
CRANIAL NEURALGIAS Presented by: Neha Sharma M.D. Date: September 27th, 2019 TYPES OF NEURALGIAS ❖ TRIGEMINAL NEURALGIA ❖ GLOSSOPHARYNGEAL NEURALGIA ❖ NASOCILIARY NEURALGIA ❖ SUPERIOR LARYNGEAL NEURALGIA ❖ SUPRAORBITAL NEURALGIA ❖ OCCIPITAL NEURALGIA ❖ SPHENOPALATINE NEURALGIA ❖ GREAT AURICULAR NEURALGIA ❖ NERVUS INTERMEDIUS NEURALGIA ❖ TROCHLEAR NEURALGIA WHAT IS CRANIAL NEURALGIA? ❖ Paroxysmal pain of head, face and/or neck ❖ Unilateral sensory nerve distribution ❖ Pain is described as sharp, shooting, lancinating ❖ Primary or Secondary causes ❖ Multiple triggers TRIGEMINAL (CN V) NEURALGIA TRIGEMINAL NEURALGIA ❖ Also called Tic Douloureux ❖ Sudden, unilateral, electrical, shock-like, shooting, sharp pain. Presents affecting Cranial Nerve V; primarily V2 and V3 branches ❖ F>M; 3:1 TRIGEMINAL NEURALGIA ❖ Anatomy of Trigeminal Nerve ❖ Cranial Nerve V ❖ Three Branches: Ophthalmic, Maxillary and Mandibular ❖ Sensory supply to forehead/supraorbital, cheeks and jaw https://www.nf2is.org/cn5.php TRIGEMINAL NEURALGIA – TRIGGERS ❖ Mastication (73%) ❖ Eating (59%) ❖ Touch (69%) ❖ Talking (58%) ❖ Brushing Teeth (66%) ❖ Cold wind (50%) TYPES OF TRIGEMINAL NEURALGIA ❖ Primary/Classic/Idiopathic ❖ Vascular compression of the nerve – superior cerebellar artery ❖ Secondary/Symptomatic ❖ Caused by intracranial lesions ❖ Tumors, Strokes, Multiple Sclerosis (4%) ❖ Typical vs. Atypical ❖ Paroxysmal (79%) vs. Continuous (21%) IASP/IHS & CLASSIFICATIONS OF TRIGEMINAL NEURALGIA ❖ IASP – International Association ❖ Classifications for the Study of Pain ❖ I