FNP Student Skills Check Off
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Frequently Asked Questions
Frequently Asked Questions What are the requirements for license renewal? Licenses Expire Contact Hours Required Each three-year registration renewal period in the licensee’s month of birth. 36 contact hours How do I complete this course and receive my certificate of completion? On-Line Submission: Go to PT.EliteCME.com and follow the prompts.You will be able to print your certificate immediately upon completion of the course. Fax Submission: Fax to (386) 673-3563, be sure to include your credit card information. All completions will be processed within 2 business days of receipt and certificates e-mailed to the e-mail address provided.* Mail Submission: Use the envelope provided or mail to Elite, PO Box 37, Ormond Beach, FL 32175. All completions will be processed and certificates issued within 10 business days from the date it is mailed.* *Please note - providing a valid e-mail address is the quickest and most efficient way to receive your certificates when submitting via fax, e-mail or mail. Submissions without a valid e-mail address will be mailed to the address provided at registration. How much will it cost? Cost of Courses Course Title Contact Hours Price Acute Injury and Pain: A Strategy, Management and Rehabilitation Discussion for Physical 3 $18.00 Therapists An Overview of Oncology Rehabilitation 4 $24.00 Common Injuries and Therapy Management for Runners 4 $24.00 Lifestyle and Therapy Approaches to Osteoporosis 3 $18.00 Reducing and Eliminating Workplace Injuries Through Ergonomics 2 $12.00 Stroke: Risk Factor Assessment, Rehabilitation Protocols and Best Practices for Prevention 2 $12.00 BEST VALUE 18-HOUR COURSE BOOK PACKAGE SAVE $11.00 18 $97.00 Are you a department approved provider? Elite Professional Education, LLC is recognized by The New York State Education Department’s Board of Physical Therapy as an approved provider of physical therapy and physical therapist assistant continuing education. -
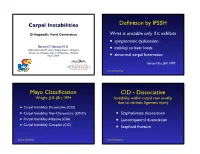
Carpal-Instability-Slide-Summary.Pdf
Carpal Instabilities Definition by IFSSH Orthopaedic Hand Conference Wrist is unstable only if it exhibits • symptomatic dysfunction Bernard F. Hearon, M.D. inability to bear loads Clinical Assistant Professor, Department of Surgery • University of Kansas School of Medicine - Wichita May 7, 2019 • abnormal carpal kinematics Garcia-Elias, JHS 1999 Carpal Instability Mayo Classification CID - Dissociative Wright, JHS (Br) 1994 Instability within carpal row usually due to intrinsic ligament injury • Carpal Instability Dissociative (CID) • Carpal Instability Non-Dissociative (CIND) • Scapholunate dissociation • Carpal Instability Adaptive (CIA) • Lunotriquetral dissociation • Carpal Instability Complex (CIC) • Scaphoid fracture Carpal Instability Carpal Instability CIND - Nondissociative Instability between carpal rows due CIA - Adaptive to extrinsic ligament injury Extra-carpal derangement causing carpal malalignment • CIND - Volar Intercalated Segment Instability (VISI) Midcarpal instability caused by malunited • CIND - Dorsal Intercalated fractures of the distal radius Segment Instability (DISI) Taleisnik, JHS 1984 • Combined CIND Carpal Instability Carpal Instability CIC - Complex Instability patterns with qualities of both CID and CIND patterns • Dorsal perilunate dislocations (lesser arc) Perilunate • Dorsal perilunate fracture-dislocations (greater arc injuries) Instability • Volar perilunate dislocations • Axial dislocations, fracture-dislocations Carpal Instability Carpal Instability Perilunate Dislocations Mayfield Classification Progressive -

A Comparative Study on Immediate Effects of Traction Straight Leg And
International Jour nal of Applie d Rese arc h 2019; 5(4): 274-278 ISSN Print: 2394-7500 ISSN Online: 2394-5869 A comparative study on immediate effects of traction Impact Factor: 5.2 IJAR 2019; 5(4): 274-278 straight leg and bent leg raise on hamstring muscle www.allresearchjournal.com Received: 07-02-2019 flexibility in normal individuals Accepted: 09-03-2019 Pooja D Kapadia Intern at Late Shree Fakirbhai Pooja D Kapadia and Dr. Virendra K Meshram Pansare Education Foundation’s College Of Abstract Physiotherapy, Nigdi, Pune, Background: Muscular flexibility is an important aspect of normal human function. Limited flexibility Maharashtra, India has been shown to predispose a person to several musculoskeletal overuse injuries and significantly affect a person’s level of function. The objective of our study was to find out the effect of mulligan Dr. Virendra K Meshram Traction Straight Leg Raise (TSLR) on hamstring flexibility, to find out the effect of Mulligan bent Leg Associate Professor, Raise (BLR) on hamstring flexibility & Comparison of Mulligan TSLR & Mulligan BLR on hamstring Department of Cardiovascular and Respiratory flexibility in normal individuals. Physiotherapy, Late Shree Method: For the present study, a total of 124 physiotherapy students were screened; of which 50 adults Fakirbhai Pansare education with hamstring muscle tightness were recruited and randomly divided into two groups: Group A- given Foundation’s College Of Mulligan Traction Straight Leg Raise and Group B- given Mulligan Bent Leg Raise. Hamstring Physiotherapy, Nigdi, Pune, flexibility was measured before and after the application of each stretching technique with the use of sit Maharashtra, India and reach test. -

Disorders of the Knee
DisordersDisorders ofof thethe KneeKnee PainPain Swelling,Swelling, effusioneffusion oror hemarthrosishemarthrosis LimitedLimited jointjoint motionmotion Screw home mechanism – pain, stiffness, fluid, muscular weakness, locking InstabilityInstability – giving way, laxity DeformityDeformity References: 1. Canale ST. Campbell’s operative orthopaedics. 10th edition 2003 Mosby, Inc. 2. Netter FH. The Netter collection of Medical illustrations – musculoskeletal system, Part I & II. 1997 Novartis Pharmaceuticals Corporation. 3. Magee DJ. Orthopedic Physical assessment. 2nd edition 1992 W. B. Saunders Company. 4. Hoppenfeld S. Physical examination of the spine and extremities. 1976 Appleton-century-crofts. AnteriorAnterior CruciateCruciate LigamentLigament Tibial insertion – broad, irregular, diamond-shaped area located directly in front of the intercondylar eminence Femoral attachment Femoral attachment Figure 43-24 In addition to their – semicircular area on the posteromedial synergistic functions, cruciate aspect of the lateral condyle and collateral ligaments exercise 33 mm in length basic antagonistic function 11 mm in diameter during rotation. A, In external Anteromedial bundle — tight in flexion rotation it is collateral ligaments that tighten and inhibit excessive Posterolateral bundle — tight in extension rotation by becoming crossed in 90% type I collagen space. B, In neutral rotation none 10% type III collagen of the four ligaments is under unusual tension. C, In internal Middle geniculate artery rotation collateral ligaments Fat -

Analysis of Rehabilitation Procedure Following Arthroplasty of the Knee with the Use of Complete Endoprosthesis
© Med Sci Monit, 2011; 17(3): CR165-168 WWW.MEDSCIMONIT.COM PMID: 21358604 Clinical Research CR Received: 2010.10.01 Accepted: 2010.12.23 Analysis of rehabilitation procedure following Published: 2011.03.01 arthroplasty of the knee with the use of complete endoprosthesis Authors’ Contribution: Magdalena Wilk-Frańczuk¹,²ACDEF, Wiesław Tomaszewski3ACDEF, Jerzy Zemła²ABDEF, A Study Design Henryk Noga4DEF, Andrzej Czamara3ADEF B Data Collection C Statistical Analysis 1 Andrzej Frycz Modrzewski Cracow University, Cracow, Poland D Data Interpretation 2 Cracow Rehabilitation Centre, Cracow, Poland E Manuscript Preparation 3 College of Physiotherapy, Wroclaw, Poland F Literature Search 4 Endoscopic Surgery Clinic and Sport Clinic Żory, Żory, Poland G Funds Collection Source of support: Departmental sources Summary Background: The use of endoprosthesis in arthroplasty requires adaptation of rehabilitation procedures in or- der to reinstate the correct model of gait, which enables the patient to recover independence and full functionality in everyday life, which in turn results in an improvement in the quality of life. Material/Methods: We studied 33 patients following an initial total arthroplasty of the knee involving endoprosthesis. The patients were divided into two groups according to age. The range of movement within the knee joints was measured for all patients, along with muscle strength and the subjective sensation of pain on a VAS, and the time required to complete the ‘up and go’ test was measured. The gait model and movement ability were evaluated. The testing was conducted at baseline and after com- pletion of the rehabilitation exercise cycle. Results: No significant differences were noted between the groups in the tests of the range of movement in the operated joint or muscle strength acting on the knee joint. -

SIMMONDS TEST: Patient Is Prone Doctor Flexes the Patients Knee to 90 Degrees Doctor Squeezes the Patient’S Calf
Clinical Orthopedic Testing Review SIMMONDS TEST: Patient is prone Doctor flexes the patients knee to 90 degrees Doctor squeezes the patient’s calf. Classical response: Failure of ankle plantarflexion Classical Importance= torn Achilles tendon Test is done bilaterally ACHILLES TAP: Patient is prone Doctor flexes the patient’s knee to 90 degree Doctor dorsiflexes the ankle and then strikes the Achilles tendon with a percussion hammer Classical response: Plantar response Classical Importance= Intact Achilles tendon Test is done bilaterally FOOT DRAWER TEST: Patient is supine with their ankles off the edge of the examination table Doctor grasps the heel of the ankle being tested with one hand and the tibia just above the ankle with the other. Doctor applies and anterior to posterior and then a posterior to anterior sheer force. Classical response: Anterior or posterior translation of the ankle Classical Importance= Anterior talofibular or posterior talofibular ligament laxity. Test is done bilaterally LATERAL STABILITY TEST: Patient is supine Doctor grasps the tibia with one hand and the foot with the other. Doctor rotates the foot into inversion Classical response: Excessive inversion Classical Importance= Anterior talofibular ligament sprain Test is done bilaterally MEDIAL STABILITY TEST: Patient is supine Doctor grasps the tibia with one hand and the foot with the other Doctor rotates the foot into eversion Classical response: Excessive eversion Classical Importance= Deltoid ligament sprain Test is done bilaterally 1 Clinical Orthopedic Testing Review KLEIGER’S TEST: Patient is seated with the legs and feet dangling off the edge of the examination table. Doctor grasps the patient’s foot while stabilizing the tibia with the other hand Doctor pulls the ankle laterally. -

Knee Pain in Children: Part I: Evaluation
Knee Pain in Children: Part I: Evaluation Michael Wolf, MD* *Pediatrics and Orthopedic Surgery, St Christopher’s Hospital for Children, Philadelphia, PA. Practice Gap Clinicians who evaluate knee pain must understand how the history and physical examination findings direct the diagnostic process and subsequent management. Objectives After reading this article, the reader should be able to: 1. Obtain an appropriate history and perform a thorough physical examination of a patient presenting with knee pain. 2. Employ an algorithm based on history and physical findings to direct further evaluation and management. HISTORY Obtaining a thorough patient history is crucial in identifying the cause of knee pain in a child (Table). For example, a history of significant swelling without trauma suggests bacterial infection, inflammatory conditions, or less likely, intra- articular derangement. A history of swelling after trauma is concerning for potential intra-articular derangement. A report of warmth or erythema merits consideration of bacterial in- fection or inflammatory conditions, and mechanical symptoms (eg, lock- ing, catching, instability) should prompt consideration of intra-articular derangement. Nighttime pain and systemic symptoms (eg, fever, sweats, night sweats, anorexia, malaise, fatigue, weight loss) are associated with bacterial infections, inflammatory conditions, benign and malignant musculoskeletal tumors, and other systemic malignancies. A history of rash or known systemic inflammatory conditions, such as systemic lupus erythematosus or inflammatory bowel disease, should raise suspicion for inflammatory arthritis. Ascertaining the location of the pain also can aid in determining the cause of knee pain. Anterior pain suggests patellofemoral syndrome or instability, quad- riceps or patellar tendinopathy, prepatellar bursitis, or apophysitis (patellar or tibial tubercle). -

Sacroiliac Joint N Ischium N Ilium N Pubis James R
Pelvic Anatomy Evidence-Based Evaluation & Treatment n Innominates of the Sacroiliac Joint n ischium n ilium n pubis James R. Scifers, DScPT, LAT, ATC Moravian College n Sacrum Athletic Training Program Articulations Biomechanics of the Pelvis n Function of the SI Joint n transmit vertical forces n Sacroiliac Joints n transmit ground n Pubic Symphysis reaction forces n Lumbo-Sacral Joint Sacral Motions Arthrokinematics of the SI Joint n During trunk flexion… n Sacral Base (S1) n Initially, sacral flexion occurs (base of sacrum n Sacral Apex (S5) moves anterior) n Flexion (nutation) n Later, sacral extension occurs with continued trunk flexion (base of sacrum moves posterior) n occurs during exhalation n Extension (counternutation) n occurs during inhalation 1 Dysfunction Classification Ilio-Sacral (IS) Dysfunctions n Sacroiliac Joint (SIJ) n Named for motion at n Any injury to SIJ PSIS n Ilio-Sacral (IS) n anterior rotation n ilium (innominate) n posterior rotation moving on sacrum n up-slip n Sacro-Iliac (SI) n down-slip (rare) n sacrum moving on ilium n in-flare n Pubic Shear n out-flare n Pubic symphysis / Pubic shear lesion Sacro-Iliac (SI) Dysfunctions Pubic Shear Lesions n Sacral Rotations n Named for “direction facing on axis” n Named for any movement at pubic n Forward Rotations symphysis n right on right n Indicates injury to pubic n left on left symphysis n Backward Rotations n right on left n left on right SI Evaluation Evidence-Based Practice (EBP) n Reliability (k) is reproducibility of test results, can be n History* intra-tester (within one clinician) or inter-tester (between n Observation** multiple clinicians) n Palpation** n Sensitivity (sens) is the ability of test to RULE OUT a condition. -

Musculoskeletal Clinical Vignettes a Case Based Text
Leading the world to better health MUSCULOSKELETAL CLINICAL VIGNETTES A CASE BASED TEXT Department of Orthopaedic Surgery, RCSI Department of General Practice, RCSI Department of Rheumatology, Beaumont Hospital O’Byrne J, Downey R, Feeley R, Kelly M, Tiedt L, O’Byrne J, Murphy M, Stuart E, Kearns G. (2019) Musculoskeletal clinical vignettes: a case based text. Dublin, Ireland: RCSI. ISBN: 978-0-9926911-8-9 Image attribution: istock.com/mashuk CC Licence by NC-SA MUSCULOSKELETAL CLINICAL VIGNETTES Incorporating history, examination, investigations and management of commonly presenting musculoskeletal conditions 1131 Department of Orthopaedic Surgery, RCSI Prof. John O'Byrne Department of Orthopaedic Surgery, RCSI Dr. Richie Downey Prof. John O'Byrne Mr. Iain Feeley Dr. Richie Downey Dr. Martin Kelly Mr. Iain Feeley Dr. Lauren Tiedt Dr. Martin Kelly Department of General Practice, RCSI Dr. Lauren Tiedt Dr. Mark Murphy Department of General Practice, RCSI Dr Ellen Stuart Dr. Mark Murphy Department of Rheumatology, Beaumont Hospital Dr Ellen Stuart Dr Grainne Kearns Department of Rheumatology, Beaumont Hospital Dr Grainne Kearns 2 2 Department of Orthopaedic Surgery, RCSI Prof. John O'Byrne Department of Orthopaedic Surgery, RCSI Dr. Richie Downey TABLE OF CONTENTS Prof. John O'Byrne Mr. Iain Feeley Introduction ............................................................. 5 Dr. Richie Downey Dr. Martin Kelly General guidelines for musculoskeletal physical Mr. Iain Feeley examination of all joints .................................................. 6 Dr. Lauren Tiedt Dr. Martin Kelly Upper limb ............................................................. 10 Department of General Practice, RCSI Example of an upper limb joint examination ................. 11 Dr. Lauren Tiedt Shoulder osteoarthritis ................................................. 13 Dr. Mark Murphy Adhesive capsulitis (frozen shoulder) ............................ 16 Department of General Practice, RCSI Dr Ellen Stuart Shoulder rotator cuff pathology ................................... -

Sacroiliac Joint Dysfunction a Case Study
NOR200188.qxd 3/8/11 9:53 PM Page 126 Sacroiliac Joint Dysfunction A Case Study CPT William Murray Pain is a widespread issue in the United States. Nine of physical therapist. She was evaluated and her treatment 10 Americans regularly suffer from pain, and nearly every consisted of a transcutaneous electrical nerve stimula- person will experience low back pain at one point in their lives. tion unit while in the PT clinic, aqua therapy, and ice Undertreated or unrelieved pain costs more than and heat application. $60 billion a year from decreased productivity, lost income, After several weeks, Ms. T returned to the primary care and medical expenses. The ability to diagnose and provide ap- provider and informed her that the pain has not decreased and “feels like that it is getting worse.” She also informed propriate medical treatment is imperative. This case study ex- the provider that she was having difficulty sleeping and amines a 23-year-old Active Duty woman who is preparing to constantly feeling tired secondary to pain. Throughout the be involuntarily released from military duty for an easily cor- next several months, the primary care provider tried nu- rectable medical condition. She has complained of chronic low merous medication trials with no relief for the patient. Ms. back pain that radiates into her hip and down her leg since ex- T gives a history of being prescribed numerous medica- periencing a work-related injury. She has been seen by numer- tions within several drug classifications. She stated vari- ous providers for the previous 11 months before being referred ous side effects that are related to the medications and to the chronic pain clinic. -

Clinical Examination of the Wrist TERRI M
Clinical Examination of the Wrist TERRI M. SKIRVEN, OTR/L, CHT AND A. LEE OSTERMAN, MD HISTORY OF THE INJURY OR ONSET PHYSICAL EXAMINATION INSPECTION OF THE WRIST GENERAL TESTS OBJECTIVE ASSESSMENTS SUMMARY DIAGNOSTIC INJECTION CRITICAL POINTS The wrist is a highly complex joint in a very compact space . Successful clinical evaluation of the wrist requires a 1. Successful clinical examination of the wrist requires a thorough knowledge of wrist anatomy, biomechanics, and thorough knowledge of wrist anatomy, biomechanics, pathology. Also required is knowledge of surface anatomy and pathology . and the corresponding underlying structures . The keys to a 2. The wrist examination includes a complete history, successful examination are to link the symptoms with the visual inspection, objective assessments, and a underlying palpable structures and to correlate the mecha- systematic physical examination, including palpation nism of the injury with the physical findings . Some common and provocative testing . conditions may be easily identified on the basis of the clinical 3. The keys to a successful examination are to link the examination, whereas others may require additional diagnos- symptoms with the underlying palpable structures and tic studies, imaging, and repeat evaluations . to correlate the mechanism of the injury with the The components of the wrist examination include a thor- physical findings . ough history, visual inspection, objective assessments, and a 4. Before the wrist is examined, a careful inspection of the systematic physical examination, including palpation and entire upper extremity should be performed to rule out provocative testing to identify tenderness and abnormal other extrinsic and more proximal causes for the wrist motion between bones. -

The Lower Extremity Exam for the Family Practitioner
Melinda A. Scott, D.O. THE LOWER EXTREMITY Orthopedic Associates of EXAM FOR THE FAMILY Dayton Board Certified in Primary Care PRACTITIONER Sports Medicine GOALS Identify landmarks necessary for exam of the lower extremity Review techniques for a quick but thorough exam Be familiar with normal findings and range of motion Review some special maneuvers and abnormal findings Review common diagnoses PRE-TEST QUESTIONS 20% 20% 20% 20% 20% If a patient has hip arthritis, where will he or she typically complain of pain? A. Buttock B. Low back C. Lateral hip D. Groin E. Posterior thigh 10 A. B. C. D. E. Countdown PRE-TEST QUESTIONS A positive straight leg raise test indicates 20% 20% 20% 20% 20% that the patient’s hip pain is from a A. Radicular/sciatic etiology B. Hip joint pathology C. Bursitis D. Tight Hamstrings E. Weak hip flexors 10 Countdown A. B. C. D. E. PRE-TEST QUESTIONS A positive McMurray’s tests is indicative of 20% 20% 20% 20% 20% a possible A. ACL tear B. MCL tear C. Patellar dislocation D. Joint effusion E. Meniscus tear 10 Countdown A. B. C. D. E. PRE-TEST QUESTIONS Anterior drawer test on the knee is performed with the knee in 20% 20% 20% 20% 20% A. 30 degrees flexion B. 90 degrees flexion C. Full extension D. 45 degrees flexion E. 130 degrees flexion 10 Countdown A. B. C. D. E. PRE-TEST QUESTIONS A positive squeeze test during an ankle 20% 20% 20% 20% 20% exam is indicative of A. Syndesmotic injury B.