Community Vulnerability to Epidemics in Nepal: a High-Resolution Spatial Assessment Amidst COVID-19 Pandemic
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

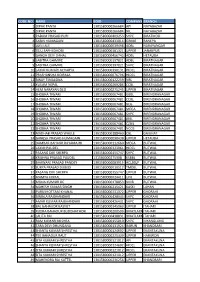
Code Under Name Girls Boys Total Girls Boys Total 010290001
P|D|LL|S G8 G10 Code Under Name Girls Boys Total Girls Boys Total 010290001 Maiwakhola Gaunpalika Patidanda Ma Vi 15 22 37 25 17 42 010360002 Meringden Gaunpalika Singha Devi Adharbhut Vidyalaya 8 2 10 0 0 0 010370001 Mikwakhola Gaunpalika Sanwa Ma V 27 26 53 50 19 69 010160009 Phaktanglung Rural Municipality Saraswati Chyaribook Ma V 28 10 38 33 22 55 010060001 Phungling Nagarpalika Siddhakali Ma V 11 14 25 23 8 31 010320004 Phungling Nagarpalika Bhanu Jana Ma V 88 77 165 120 130 250 010320012 Phungling Nagarpalika Birendra Ma V 19 18 37 18 30 48 010020003 Sidingba Gaunpalika Angepa Adharbhut Vidyalaya 5 6 11 0 0 0 030410009 Deumai Nagarpalika Janta Adharbhut Vidyalaya 19 13 32 0 0 0 030100003 Phakphokthum Gaunpalika Janaki Ma V 13 5 18 23 9 32 030230002 Phakphokthum Gaunpalika Singhadevi Adharbhut Vidyalaya 7 7 14 0 0 0 030230004 Phakphokthum Gaunpalika Jalpa Ma V 17 25 42 25 23 48 030330008 Phakphokthum Gaunpalika Khambang Ma V 5 4 9 1 2 3 030030001 Ilam Municipality Amar Secondary School 26 14 40 62 48 110 030030005 Ilam Municipality Barbote Basic School 9 9 18 0 0 0 030030011 Ilam Municipality Shree Saptamai Gurukul Sanskrit Vidyashram Secondary School 0 17 17 1 12 13 030130001 Ilam Municipality Purna Smarak Secondary School 16 15 31 22 20 42 030150001 Ilam Municipality Adarsha Secondary School 50 60 110 57 41 98 030460003 Ilam Municipality Bal Kanya Ma V 30 20 50 23 17 40 030460006 Ilam Municipality Maheshwor Adharbhut Vidyalaya 12 15 27 0 0 0 030070014 Mai Nagarpalika Kankai Ma V 50 44 94 99 67 166 030190004 Maijogmai Gaunpalika -

FOREIGN COOPERATION BRANCH Nepal India Regional Trade and Transport Project
Terms of Reference GOVERNMENT OF NEPAL MINISTRY OF PHYSICAL INFRASTRUCTURE AND TRANSPORT DEPARTMENT OF ROADS FOREIGN COOPERATION BRANCH Nepal India Regional Trade and Transport Project TERMS OF REFERENCE of Bridge Engineer (Resident Engineer) For CONSTRUCTION SUPERVISION OF Construction of Khani Khola, Mauri Khola , Dasdhunga Khola and Jalbire Khola Bridge on Narayanghat – Mugling Road Road January, 2018 Jwagal, Lalitpur Page 1 of 9 Terms of Reference TERMS OF REFERENCE of Bridge Engineer (Resident Engineer) For CONSTRUCTION SUPERVISION OF Construction of Khani Khola, Mauri Khola , Dasdhunga Khola and Jalbire Khola Bridge on Narayanghat – Mugling Road Road 1. INTRODUCTION AND BACKGROUND The Government of Nepal has received financing from the World Bank toward the cost of the Nepal India Regional Trade and Transport Project for the improvement of Naryanghat – Mugling Road. Under the project it has started to construct the new bridges in following rivers: a) Khani Khola b) Mauri Khola c) Dasdhunga Khola and d) Jalbire Khola Nepal India Regional Trade and Transport Project has procured contracts of ”Construction of Bridges over Khani, Mauri, Dasdhunga and Jalbire River” in two following contracts which are in construction stage. Contract ID No. Name of Contractor Bridge Name Lama Construction Company Construction of RCC Bridges over NIRTTP-DOR-W-NCB- Pvt Ltd, Maharajgunj, Khani, Mauri and Dasdhunga River 4 Kathmandu along Narayanghat – Mugling Road Rautaha Construction Pvt Ltd, Construction of Prestressed Concrete NIRTTP-DOR-W-NCB- Triyuga municipality, Udaypur Bridge over Jalbire River along 5 Narayanghat – Mugling Road Nepal India Regional Trade and Transport Project, Foreign Cooperation Branch, Department of Roads under the Ministry of Physical Infrastructure and Transport intends to apply part of the proceeds for consulting service of the Bridge Engineer (Resident Engineer). -

Nepal: SASEC Road Connectivity Project: Leguwaghat-Bhojpur
Initial Environmental Examination February 2013 NEP: SASEC Road Connectivity Project Leguwaghat — Bhojpur Subproject Prepared by the Department of Road, Ministry of Physical Planning, Works and Transport Management for the Asian Development Bank. 16. ii CURRENCY EQUIVALENTS (as of 21 February 2013) Currency unit – Nepalese rupee (NR) NR1.00 – $ 0.0115340254 $1.00 – NR86.700000 ABBREVIATIONS EPR Environmental Protection Rules ES Environmental Specialist EWH East-West Highway FIDIC Federation International Des Ingenieurs- Conseils FS Feasibility Study GESU Geo-Environmental and Social Unit GHG Green House Gas IA Implementing Agency ICIMOD International Centre for Integrated Mountain Development IEE Initial Environmental Examination IUCN International Union for Conservation of Nature JICA Japan International Co-operative Agency LPG Liquefied Petroleum Gas MCT Main Central Trust MHH Mid-Hill Highway MOE Ministry of Environment MoPPW Ministry of Physical Planning and Works MRM Mahendra Raj Marg NAAQS Nepal Ambient Air Quality Standard NEP Nepal NGO Non Government Organization NOx Nitrogen Oxide OD Origin-Destination PD Project Directorate pH Percentage of Hydrogen PPE Personal Protective Equipment PIP Priority Investment Plan PPMO Public Procurement Monitoring Office RCP Road Connectivity Project - ADB RAP Rural Access Programmme -DFID RAP Rural Access Program RCC Reinforced Cement Concrete RCSP Road Connectivity Sector Project - ADB iii REA Rapid Environmental Assessment RIP Road Improvement Project- DOR RNDP Road Network Development Project -

Pro-Poor Tourism Case Study from Humla District, West
48 6. Appendices 6.1 Data on tourist numbers in Humla Table A1 Number of trekking permits issued16 1993 1994 1995 1996 1997 1998 1999 2000 28 209 191 462 404 558 949 595 Table A2 Nationality of tourists registering at Simikot Police Station 1996-2000 (top ten nationalities account for 97% of visitors ) % of total tourists SN Country over 4 years 1 Germany 27.13 2 Australia/Austria 13.65 3 Switzerland 11.61 4 USA 11.45 5 France 9.36 6 UK 7.76 7 Italy 5.12 8 Spain 2.64 9 Netherlands 2.20 10 Japan 1.65 16 Source: Paudyal & Sharma 2000 49 6.2 Background information on SNV’s programmes in Humla preceding the DPP sustainable tourism programme 1985-1992 A Trail and Bridge Building Project was run to improve infrastructure in the Karnali Zone because this was seen to be a pre-requisite for developing the area generally. The project completed a total of 21 bridges, 2 trails and 10 drinking water schemes covering several Karnali Zone districts. In Humla, work on trails, 7 bridges, and several drinking water projects were completed. On the Simikot - Hilsa trail a suspension bridge crossing the Karnali River at Yalbang and a section of trail called ‘Salli-Salla’ were constructed. 1993 – September 1999 The Karnali Local Development Programme was run to further develop infrastructural improvements and to integrate these with social development by building capacity at community and local NGO levels. The district level activities included • District Development Committee (DDC) (i.e. local government) capacity building in participatory planning; • Improvement of intra-district infrastructure; and • Support of NGOs committed to work in the Karnali Zone. -
Code No Name Boid Company Branch 1 Dipak Panta
CODE NO NAME BOID COMPANY BRANCH 1 DIPAK PANTA 1301580000266684 API NAYABAZAR 2 DIPAK PANTA 1301580000266684 NIL NAYABAZAR 3 PADAM PRASAD PURI 1301580000409253 SHPC BIRATMOD 4 SABIN HUMAGAIN 1301580000433014 GBIME BANEPA 5 UJELI ALE 1301580000039498 ADBL NARAYANGAR 6 TEJU SAPHI DHOBI 1301580000181321 UPPER JANAKPUR 7 GANGA DEVI DAHAL 1301580000456743 ADBL HETAUDA 8 SABITRA GHIMIRE 1301580000197821 ADBL BIRATNAGAR 9 SABITRA GHIMIRE 1301580000197821 SHPC BIRATNAGAR 10 LAXMI KUMARI ACHARYA 1301580000390131 HIDCL BIRATNAGAR 11 PRASHANSHA KOIRALA 1301580000076796 HIDCL BIRATNAGAR 12 BINAY TIMALSINA 1301580000122259 NBL BIRATNAGAR 13 KUSUM NEPAL 1301580000269286 CCBL BIRATNAGAR 14 HEM NARAYAN DEO 1301580000275245 UPPER BIRATNAGAR 15 SHOBHA TIWARI 1301580000067481 GBBL BIRENDRANAGAR 16 SHOBHA TIWARI 1301580000067481 CCBL BIRENDRANAGAR 17 SHOBHA TIWARI 1301580000067481 NLG BIRENDRANAGAR 18 SHOBHA TIWARI 1301580000067481 MEGA BIRENDRANAGAR 19 SHOBHA TIWARI 1301580000067481 SHPC BIRENDRANAGAR 20 SHOBHA TIWARI 1301580000067481 JBBL BIRENDRANAGAR 21 SHOBHA TIWARI 1301580000067481 CZBIL BIRENDRANAGAR 22 SHOBHA TIWARI 1301580000067481 NCCB BIRENDRANAGAR 23 MADHAB PRASAD WAGLE 1301580000188460 CBL GAIGHAT 24 GANESH PRASAD HUMAGAIN 1301580000098438 UPPER HETAUDA 25 DAMBAR BAHAUR RAYAMAJHI 1301580000112660 MEGA BUTWAL 26 LAXMI PAUDEL 1301580000323961 HIDCL BUTWAL 27 PASANG DIKI SHERPA 1301580000155747 SHPC BUTWAL 28 KRISHNA PRASAD PAUDEL 131580000275908 KSBBL BUTWAL 29 BHAWANI PRASAD PANDEY 1301580000083915 ACLBSLP BUTWAL 30 SURYA PRASAD DUBEDI 1301580000010512 -
Preparation of GPS Based Digital Profile of Godawari Municipality
Godawari Municipality Godawari, Lalitpur Final Report Preparation of GPS based Digital Profile of Godawari Municipality Submitted to Godawari Municipality Bajrabarahi, Lalitpur, Nepal Submitted by ArchieSoft Technology Lalitpur Metropolitan City 21, Lalitpur, Nepal Phone: +977 -1-5553000 Email: [email protected] Web: www.archiesoft.com.np 1 Table of Contents Chapter 1: Project Description ............................................................................................................... 4 1.1 Background ......................................................................................................................................... 4 1.2 Objective of the assignment ............................................................................................................... 4 1.3 Key Deliverables ................................................................................................................................. 5 1.4 Methodology/ process ....................................................................................................................... 5 1.5 Project Location .................................................................................................................................. 6 1.6 Time line of assignment/ study .......................................................................................................... 7 Chapter 2: Godawari Municipality an Introduction ............................................................................... 9 2.1 Background: ....................................................................................................................................... -
Sustainable Development Goals Baseline Report of Province No
Sustainable Development Goals Baseline Report of Province No. Five Province Planning Commission, Government of Province, Province No. Five 2 Sustainable Development Goals Baseline Report Province Planning Commission, Government of Province, Province No. Five This report was prepared and published in 2019 by the Province Planning Commission, Government of Province, Province No. Five, with the support from United Nations Development Programme. Photo Credit: UNDP Nepal, Laxmi Prasad Ngakhusi, CP Khanal Preface The government of Province No. 5 has been forward for achieving the goals so that formulating first five-year plan (2019/20 - no one will be left behind. This report has 2023/24) of the province with a vision of helped us to set the targets to be achieved 'prosperous province, happy people'. The in our five-year plan. Local governments, goals and priorities of the plan match with civil society organizations, private sector of the Sustainable Development Goals (SDGs) this province and interested development agreed by the global community for the partners will also benefit from this report period of 2016-2030. As the Government to identify the areas where they need to of Nepal has shown its commitment on the focus to help the provincial government in realization of SDGs at the international level, achieving the SDGs. this province intends to localize the SDGs to the provincial context to contribute in The Province Planning Commission would the fulfillment of the national commitment. like to thank the UNDP for helping us to This SDG baseline report is produced under prepare this milestone report and also to technical and financial support from UNDP the team of experts Dr. -

Feasibility Study of Kailash Sacred Landscape
Kailash Sacred Landscape Conservation Initiative Feasability Assessment Report - Nepal Central Department of Botany Tribhuvan University, Kirtipur, Nepal June 2010 Contributors, Advisors, Consultants Core group contributors • Chaudhary, Ram P., Professor, Central Department of Botany, Tribhuvan University; National Coordinator, KSLCI-Nepal • Shrestha, Krishna K., Head, Central Department of Botany • Jha, Pramod K., Professor, Central Department of Botany • Bhatta, Kuber P., Consultant, Kailash Sacred Landscape Project, Nepal Contributors • Acharya, M., Department of Forest, Ministry of Forests and Soil Conservation (MFSC) • Bajracharya, B., International Centre for Integrated Mountain Development (ICIMOD) • Basnet, G., Independent Consultant, Environmental Anthropologist • Basnet, T., Tribhuvan University • Belbase, N., Legal expert • Bhatta, S., Department of National Park and Wildlife Conservation • Bhusal, Y. R. Secretary, Ministry of Forest and Soil Conservation • Das, A. N., Ministry of Forest and Soil Conservation • Ghimire, S. K., Tribhuvan University • Joshi, S. P., Ministry of Forest and Soil Conservation • Khanal, S., Independent Contributor • Maharjan, R., Department of Forest • Paudel, K. C., Department of Plant Resources • Rajbhandari, K.R., Expert, Plant Biodiversity • Rimal, S., Ministry of Forest and Soil Conservation • Sah, R.N., Department of Forest • Sharma, K., Department of Hydrology • Shrestha, S. M., Department of Forest • Siwakoti, M., Tribhuvan University • Upadhyaya, M.P., National Agricultural Research Council -

Federal Democratic Republic of Nepal
FEDERAL DEMOCRATIC REPUBLIC OF NEPAL MINISTRY OF IRRIGATION MINISTRY OF AGRICULTURE DEVELOPMENT FEDERAL DEMOCRATIC REPUBLIC OF NEPAL NEPAL AGRICULTURE RESEARCH COUNCIL MINISTRY OF IRRIGATION MINISTRY OF AGRICULTURE DEVELOPMENT NEPAL AGRICULTUREPREPARATORY RESEARCH SURVEY COUNCIL ON JICA'S COOPERATION PROGRAM FOR AGRICULTUREPREPARATORY AND RURAL SURVEY DEVELOPMENT IN NEPALON JICA'S COOPERATION PROGRAM - FOODFOR AGRICULTURE PRODUCTION ANDAND AGRICULTURERURAL DEVELOPMENT IN TERAI - IN NEPAL - FOOD PRODUCTION AND AGRICULTURE IN TERAI - FINAL REPORT MAIN REPORT FINAL REPORT MAIN REPORT OCTOBER 2013 JAPAN INTERNATIONAL COOPERATION AGENCY OCTOBER(JICA) 2013 JAPAN INTERNATIONALNIPPON KOEI COOPERATION CO., LTD. AGENCY VISION AND SPIRIT(JICA) FOR OVERSEAS COOPERATION (VSOC) CO., LTD. NIPPON KOEI CO., LTD. C.D.C. INTERNATIONAL CORPORATION VISION AND SPIRIT FOR OVERSEAS COOPERATION (VSOC) CO., LTD. 4R C.D.C. INTERNATIONAL CORPORATION JR 13 - 031 FEDERAL DEMOCRATIC REPUBLIC OF NEPAL MINISTRY OF IRRIGATION MINISTRY OF AGRICULTURE DEVELOPMENT FEDERAL DEMOCRATIC REPUBLIC OF NEPAL NEPAL AGRICULTURE RESEARCH COUNCIL MINISTRY OF IRRIGATION MINISTRY OF AGRICULTURE DEVELOPMENT NEPAL AGRICULTUREPREPARATORY RESEARCH SURVEY COUNCIL ON JICA'S COOPERATION PROGRAM FOR AGRICULTUREPREPARATORY AND RURAL SURVEY DEVELOPMENT IN NEPALON JICA'S COOPERATION PROGRAM - FOODFOR AGRICULTURE PRODUCTION ANDAND AGRICULTURERURAL DEVELOPMENT IN TERAI - IN NEPAL - FOOD PRODUCTION AND AGRICULTURE IN TERAI - FINAL REPORT MAIN REPORT FINAL REPORT MAIN REPORT OCTOBER 2013 JAPAN INTERNATIONAL -
Forests and Watershed Profile of Local Level (744) Structure of Nepal
Forests and Watershed Profile of Local Level (744) Structure of Nepal Volumes: Volume I : Forest & Watershed Profile of Province 1 Volume II : Forest & Watershed Profile of Province 2 Volume III : Forest & Watershed Profile of Province 3 Volume IV : Forest & Watershed Profile of Province 4 Volume V : Forest & Watershed Profile of Province 5 Volume VI : Forest & Watershed Profile of Province 6 Volume VII : Forest & Watershed Profile of Province 7 Government of Nepal Ministry of Forests and Soil Conservation Department of Forest Research and Survey Kathmandu July 2017 © Department of Forest Research and Survey, 2017 Any reproduction of this publication in full or in part should mention the title and credit DFRS. Citation: DFRS, 2017. Forests and Watershed Profile of Local Level (744) Structure of Nepal. Department of Forest Research and Survey (DFRS). Kathmandu, Nepal Prepared by: Coordinator : Dr. Deepak Kumar Kharal, DG, DFRS Member : Dr. Prem Poudel, Under-secretary, DSCWM Member : Rabindra Maharjan, Under-secretary, DoF Member : Shiva Khanal, Under-secretary, DFRS Member : Raj Kumar Rimal, AFO, DoF Member Secretary : Amul Kumar Acharya, ARO, DFRS Published by: Department of Forest Research and Survey P. O. Box 3339, Babarmahal Kathmandu, Nepal Tel: 977-1-4233510 Fax: 977-1-4220159 Email: [email protected] Web: www.dfrs.gov.np Cover map: Front cover: Map of Forest Cover of Nepal FOREWORD Forest of Nepal has been a long standing key natural resource supporting nation's economy in many ways. Forests resources have significant contribution to ecosystem balance and livelihood of large portion of population in Nepal. Sustainable management of forest resources is essential to support overall development goals. -

Food Insecurity and Undernutrition in Nepal
SMALL AREA ESTIMATION OF FOOD INSECURITY AND UNDERNUTRITION IN NEPAL GOVERNMENT OF NEPAL National Planning Commission Secretariat Central Bureau of Statistics SMALL AREA ESTIMATION OF FOOD INSECURITY AND UNDERNUTRITION IN NEPAL GOVERNMENT OF NEPAL National Planning Commission Secretariat Central Bureau of Statistics Acknowledgements The completion of both this and the earlier feasibility report follows extensive consultation with the National Planning Commission, Central Bureau of Statistics (CBS), World Food Programme (WFP), UNICEF, World Bank, and New ERA, together with members of the Statistics and Evidence for Policy, Planning and Results (SEPPR) working group from the International Development Partners Group (IDPG) and made up of people from Asian Development Bank (ADB), Department for International Development (DFID), United Nations Development Programme (UNDP), UNICEF and United States Agency for International Development (USAID), WFP, and the World Bank. WFP, UNICEF and the World Bank commissioned this research. The statistical analysis has been undertaken by Professor Stephen Haslett, Systemetrics Research Associates and Institute of Fundamental Sciences, Massey University, New Zealand and Associate Prof Geoffrey Jones, Dr. Maris Isidro and Alison Sefton of the Institute of Fundamental Sciences - Statistics, Massey University, New Zealand. We gratefully acknowledge the considerable assistance provided at all stages by the Central Bureau of Statistics. Special thanks to Bikash Bista, Rudra Suwal, Dilli Raj Joshi, Devendra Karanjit, Bed Dhakal, Lok Khatri and Pushpa Raj Paudel. See Appendix E for the full list of people consulted. First published: December 2014 Design and processed by: Print Communication, 4241355 ISBN: 978-9937-3000-976 Suggested citation: Haslett, S., Jones, G., Isidro, M., and Sefton, A. (2014) Small Area Estimation of Food Insecurity and Undernutrition in Nepal, Central Bureau of Statistics, National Planning Commissions Secretariat, World Food Programme, UNICEF and World Bank, Kathmandu, Nepal, December 2014. -

Enterprises for Self Employment in Banke and Dang
Study on Enterprises for Self Employment in Banke and Dang Prepared for: USAID/Nepal’s Education for Income Generation in Nepal Program Prepared by: EIG Program Federation of Nepalese Chambers of Commerce and Industry Shahid Sukra Milan Marg, Teku, Kathmandu May 2009 TABLE OF CONTENS Page No. Acknowledgement i Executive Summary ii 1 Background ........................................................................................................................ 9 2 Objective of the Study ....................................................................................................... 9 3 Methodology ...................................................................................................................... 9 3.1 Desk review ............................................................................................................... 9 3.2 Focus group discussion/Key informant interview ..................................................... 9 3.3 Observation .............................................................................................................. 10 4 Study Area ....................................................................................................................... 10 4.1 Overview of Dang and Banke district ...................................................................... 10 4.2 General Profile of Five Market Centers: .................................................................. 12 4.2.1 Nepalgunj ........................................................................................................