Table of Contents
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

"National List of Vascular Plant Species That Occur in Wetlands: 1996 National Summary."
Intro 1996 National List of Vascular Plant Species That Occur in Wetlands The Fish and Wildlife Service has prepared a National List of Vascular Plant Species That Occur in Wetlands: 1996 National Summary (1996 National List). The 1996 National List is a draft revision of the National List of Plant Species That Occur in Wetlands: 1988 National Summary (Reed 1988) (1988 National List). The 1996 National List is provided to encourage additional public review and comments on the draft regional wetland indicator assignments. The 1996 National List reflects a significant amount of new information that has become available since 1988 on the wetland affinity of vascular plants. This new information has resulted from the extensive use of the 1988 National List in the field by individuals involved in wetland and other resource inventories, wetland identification and delineation, and wetland research. Interim Regional Interagency Review Panel (Regional Panel) changes in indicator status as well as additions and deletions to the 1988 National List were documented in Regional supplements. The National List was originally developed as an appendix to the Classification of Wetlands and Deepwater Habitats of the United States (Cowardin et al.1979) to aid in the consistent application of this classification system for wetlands in the field.. The 1996 National List also was developed to aid in determining the presence of hydrophytic vegetation in the Clean Water Act Section 404 wetland regulatory program and in the implementation of the swampbuster provisions of the Food Security Act. While not required by law or regulation, the Fish and Wildlife Service is making the 1996 National List available for review and comment. -

Rubiaceae) in Africa and Madagascar
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Springer - Publisher Connector Plant Syst Evol (2010) 285:51–64 DOI 10.1007/s00606-009-0255-8 ORIGINAL ARTICLE Adaptive radiation in Coffea subgenus Coffea L. (Rubiaceae) in Africa and Madagascar Franc¸ois Anthony • Leandro E. C. Diniz • Marie-Christine Combes • Philippe Lashermes Received: 31 July 2009 / Accepted: 28 December 2009 / Published online: 5 March 2010 Ó The Author(s) 2010. This article is published with open access at Springerlink.com Abstract Phylogeographic analysis of the Coffea subge- biogeographic differentiation of coffee species, but they nus Coffea was performed using data on plastid DNA were not congruent with morphological and biochemical sequences and interpreted in relation to biogeographic data classifications, or with the capacity to grow in specific on African rain forest flora. Parsimony and Bayesian analyses environments. Examples of convergent evolution in the of trnL-F, trnT-L and atpB-rbcL intergenic spacers from 24 main clades are given using characters of leaf size, caffeine African species revealed two main clades in the Coffea content and reproductive mode. subgenus Coffea whose distribution overlaps in west equa- torial Africa. Comparison of trnL-F sequences obtained Keywords Africa Á Biogeography Á Coffea Á Evolution Á from GenBank for 45 Coffea species from Cameroon, Phylogeny Á Plastid sequences Á Rubiaceae Madagascar, Grande Comore and the Mascarenes revealed low divergence between African and Madagascan species, suggesting a rapid and radial mode of speciation. A chro- Introduction nological history of the dispersal of the Coffea subgenus Coffea from its centre of origin in Lower Guinea is pro- Coffeeae tribe belongs to the Ixoroideae monophyletic posed. -

In Search of the Perfect Aphrodisiac: Parallel Use of Bitter Tonics in West Africa and the Caribbean
Journal of Ethnopharmacology 143 (2012) 840–850 Contents lists available at SciVerse ScienceDirect Journal of Ethnopharmacology journal homepage: www.elsevier.com/locate/jep In search of the perfect aphrodisiac: Parallel use of bitter tonics in West Africa and the Caribbean Tinde van Andel a,n, Sylvia Mitchell b, Gabriele Volpato c, Ina Vandebroek d, Jorik Swier e, Sofie Ruysschaert f, Carlos Ariel Renterı´a Jime´nez g, Niels Raes a a Naturalis Biodiversity Center, Section National Herbarium of the Netherlands, PO Box 9514, 2300 RA Leiden, The Netherlands b Medicinal Plant Research Group, Biotechnology Centre, University of the West Indies, 2 St. John’s Close, Mona Campus, Kingston 7, Jamaica c CERES Research School, De Leeuwenborch, Wageningen University and Research Centre, Hollandseweg 1, 6706 KN Wageningen, The Netherlands d Institute of Economic Botany, New York Botanical Garden, 2900 Southern Boulevard Bronx, 10458 NY, United States e Wageningen University and Research Center, Droevendaalsesteeg 2, 6708 PB Wageningen, The Netherlands f Laboratory of Tropical and Subtropical Agriculture and Ethnobotany, Ghent University, Coupure Links 653, 9000 Ghent, Belgium g Instituto de Investigaciones Ambientales del Pacı´fico ‘‘John Von Neumann’’, Cra 6 Nro 37–39, Quibdo´, Colombia article info abstract Article history: Ethnopharmacological relevance: Enslaved Africans in the Americas had to reinvent their medicinal flora Received 30 June 2012 in an unknown environment by adhering to plants that came with them, learning from Amerindians Accepted 7 August 2012 and Europeans, using their Old World knowledge and trial and error to find substitutes for their Available online 17 August 2012 homeland herbs. This process has left few written records, and little research has been done on Keywords: transatlantic plant use. -

Diplomarbeit
DIPLOMARBEIT Titel der Diplomarbeit Blütenbiologische Beobachtungen an ausgewählten Rubiaceen des Esquinas-Regenwaldes (Costa Rica) angestrebter akademischer Grad Magistra der Naturwissenschaften (Mag. rer.nat) Verfasserin / Verfasser: Stefanie Csekits Matrikel-Nummer: 9100989 Studienrichtung /Studienzweig Biologie / Botanik (lt. Studienblatt): Betreuerin / Betreuer: Prof. Michael Kiehn Wien, im Oktober 2008 1 2 Inhalt Inhalt Abstract 1.Einleitung 1.1 Motivation 1.2 Allgemeine Information 1.2.1 Die Geschichte der Bestäubungsbiologie 1.2.2 Blütenmerkmale der Rubiaceen 1.2.3 Blütenbiologie Neotropischer Rubiaceen 1.2.4 Bestäubungssyndrome und Bestäuber 1.2.4.1 Bestäubungssyndrome 2.Studiengebiet, Material und Methoden 2.1 Studiengebiet 2.1.1 Geographie 2.1.2 Klima 2.1.3 Vegetation 2.1.4 Esquinas Regenwald 2.2 Feldarbeit 2.2.1 Bestimmung von Pflanzen 2.2.2 Bestimmung von Insekten und Vögeln 2.3.Morphologische Untersuchungen 2.3.1 Infloreszenzen und Blütenvermessungen 2.4 Phänologische Untersuchungen 2.4.1 Blühperioden 2.4.2 Lebensdauer von Einzelblüten 2.5 Belohnung für Blütenbesucher 2.5.1 Duft 2.5.2 Nektar 2.5.2.1 Nektarmenge 2.5.2.1 Nektar Zuckerkonzentration 2.6 Blütenbesucher 2.7 Reproduktionssystem 2.7.1 Bagging-Experimente 2.7.2 Narbenempfängnisbereitschaft 2.7.3 Pollen/Samenanlagen Rate 3. Ergebnisse 3.1 Diverse Blütenbiologische Untersuchungen 3.1.1 Bestäubungssyndrome der Rubiaceae in der Golfo Dulce Region 3.1.2 Heterostyle Arten 3.1.3 Lebensdauer von Einzelblüten 3.2 Isertia haenkeana 3.2.1Morphologie 3.2.1.1 Vegetativer Bau 3.2.1.2 Reproduktive Pflanzenteile 3.2.1.2.1 Infloreszenzen 3.2.1.2.2 Gelbblühende Form von Isertia haenkeana 3 3.2.1.2.3 Blüte 3.2.1.2.4 Pleiomerie 3.2.1.2.4.1 Sonderfall fusionierte Blüte 3.2.2 Phänologie 3.2.2.1 Entwicklung innerhalb der Population 3.2.2.2 Entwicklung der Blüte 3.2.2.2.1 Zeitliche Abläufe während der Anthese 3.2.2.2.2 Der legitime Blütenbesuch 3.2.2.3 Früchte und Samen 3.2.2.3.1 Infukteszenen 3.2.2.3.2 Früchte 3.2.2.3.3. -

Rediscovery of Arrabidaea Chica (Bignoniaceae) and Entada Polystachya Var
Phytotaxa 125 (1): 53–58 (2013) ISSN 1179-3155 (print edition) www.mapress.com/phytotaxa/ Article PHYTOTAXA Copyright © 2013 Magnolia Press ISSN 1179-3163 (online edition) http://dx.doi.org/10.11646/phytotaxa.125.1.8 Rediscovery of Arrabidaea chica (Bignoniaceae) and Entada polystachya var. polyphylla (Fabaceae) in Puerto Rico MARCOS A. CARABALLO-ORTIZ Herbarium, Botanical Garden of the University of Puerto Rico, 1187 Calle Flamboyán, San Juan, Puerto Rico 00926, USA. Current address: Pennsylvania State University, Department of Biology, 208 Mueller Laboratory, University Park, Pennsylvania 16802, USA. E-mail: [email protected]; [email protected] Abstract In this contribution the rediscovery of the lianas Arrabidaea chica (Bignoniaceae) and Entada polystachya var. polyphylla (Fabaceae-Mimosoideae) in Puerto Rico is reported. These species were first collected during the 1880s and subsequently considered extirpated. Their current status in Puerto Rico is discussed, and recommendations for their conservation are offered. Introduction During the decade of 1880, the German botanist Paul Ernst Emil Sintenis and the Puerto Rican naturalist Agustín Stahl collected several plant species and made significant contributions to the knowledge of the flora of Puerto Rico (Urban 1903–1911, Stahl 1883–1888). During their explorations throughout the island, Sintenis and Stahl collected several species new to science and new records for Puerto Rico, some of which are still known only from their collections (Acevedo-Rodríguez 2007, 2013). Examples of these are Arrabidaea chica (Bonpl. in Humboldt & Bonpland 1807: 107, pl. 31) Verlot (1868: 154) (Bignoniaceae) and Entada polystachya (Linnaeus 1753: 520) Candolle (1825: 425) var. polyphylla (Bentham 1840: 133) Barneby (1996: 175) [synonym: Entadopsis polyphylla (Benth.) Britton (in Britton & Rose 1928: 191)] (Fabaceae-Mimosoideae), both collected in 1885 and 1886. -

Of the FLORIDA STATE MUSEUM Biological Sciences
of the FLORIDA STATE MUSEUM Biological Sciences Volume 32 1987 Number 1 FLORISTIC STUDY OF MORNE LA VISITE AND PIC MACAYA NATIONAL PARKS, HAITI Walter S. Judd THREE NEW ANGIOSPERMS FROM PARC NATIONAL PIC MACAYA, MASSIF DE LA HOTTE, HAITI Walter S. Judd and James D. Skean, Jr. S A./4 UNIVERSITY OF FLORIDA GAINESVILLE Numbers of the BULLETIN OF THE FLORIDA STATE MUSEUM, BIOLOGICAL SCIENCES, are published at irregular intervals. Volumes contain about 300 pages and are not necessarily completed in any one calendar year. OLIVER L. AuSTIN, JR., Editor S. DAVID WEBB, Associate Editor RHODA J. BRYANL Managing Editor Consultants for this issue: JOHN H. BEAMAN JAMES L. LUTEYN Communications concerning purchase or exchange of the publications and all manuscripts should be addressed to: Managing Editor, Bulletin; Florida State Museum; University of Florida; Gainesville FL 32611; U.S.A. This public document was promulgated at an annual cost of $6240.00 or $6.240 per copy. It makes available to libraries, scholars, and all interested persons the results of researches in the natural sciences, emphasizing the circum-Caribbean region. ISSN: 0071-6154 CODEN: BF 5BA5 Publication date: December 23, 1987 Price: $6.40 FLORISTIC STUDY OF MORNE LA VISITE AND PIC MACAYA NATIONAL PARKS, HAITIl Walter S. Judd2 ABSTRACT A floristic and vegetational survey of two recently established national parks in the poorly known mountains of southern Haiti, i.e. Parc National Pic Macaya (in the Massif de La Hotte) and Parc National Morne La Visite (in the Massif de La Selle), clearly documents the rich and highly endemic nature of the tracheophyte (especially angiosperm) flora of the parks, and confirms EL Ekman's early reports of the region's flora. -

Structure and Composition of Moist Coastal Forests in Dorado, Puerto Rico
r Un~tedStates f@ji Department of Agriculture Structure and Composition of Forest Serv~ce Moist Coastal Forests in Southern Forest Experiment Station Dorado, Puerto Rico New Orleans. Louisiana Research Paper Julio C. Figueroa, Luis Totti, Ariel E. Lugo, and Roy 0.Woodbury SO-202 February 1984 An Institute of Tropical Forestry Publication SUMMARY A survey of forest structure, species composition, and change in forest areas over a 44 year period was conducted on 39.5 ha of forest lands in Dorado, Puerto Rico, where H. A. Gleason and M. T. Cook had studied forest conditions in 1926. A total of 51 tree species were found in the study area. Six forest types were identified on white sands and poorly drained clay soil. The most complex forest was the 19.7 m tall old secondary forest with 32 tree species, 1,880 stemslha, a basal area of 41.6 mVha, and a complexity index of 493. Abandoned palm groves (5 tree species), a disturbed open forest with 9 tree species and dominated by Hymenaea courban'l, a Clusia-Zyzygium forest (11 tree species), and a young secondary forest with 19 tree species (also dominated by H. courbaril) were all undergoing succession towards the old secondary forest. This forest is considered to be the climax on white sands. In flooded soils, Pterocarpus officinalis and six other tree species form a climax swamp forest that has not changed in composition for the last 54 years. In terms of forest area, however, Pterocarpus and old secondary forests have been reduced by 30 percent and 79 percent, respectively. -

Research Article
s z Available online at http://www.journalcra.com INTERNATIONAL JOURNAL OF CURRENT RESEARCH International Journal of Current Research Vol. 9, Issue, 02, pp.46960-46976, February, 2017 ISSN: 0975-833X RESEARCH ARTICLE CONTRIBUTION TO THE KNOWLEDGE OF THE SPECIFIC ASPECTS OF THE LESSER ANTILLES FLORA: THE VEGETATION INVERSIONS (THE CASE OF MARTINIQUE’S LOWER PLANT LEVEL) *Philippe JOSEPH Professor of Ecology, Botany and Biogeography, University of the frenchWest Indies (Martinique)-UMR ESPACE DEV -BIORECA ARTICLE INFO ABSTRACT Article History: The main physical factors influencing the diversity of phytocenoses are the climate and geomorphology. The latter’s various aspects can modify, for example, the spatiotemporal structure of Received 18th November, 2016 Received in revised form the temperature, rainfall, humidity and evaporation. These changes result in a set of biotopes whose 20th December, 2016 varied biocenotic responses correspond to a dense floristic mosaic. Among these responses, due to Accepted 25th January, 2017 their small size, the vegetation inversions represent specific cases. To demonstrate this phenomenon, Published online 28th February, 2017 we used 73 stations of Martinique’s lower level influenced by the dry sub-humid bioclimate and occupying each of the specific topographic facies. Using indicators and a multifactorial treatment Key words: (AFC), the data from the floristic inventories revealed the existence of a station whose flora is composed of mesophilous (evergreen tropical seasonal) species typical of the wet or even wet sub- Lesser Antilles, Martinique, Topography, humid bioclimate. Bioclimates, Phytocenoses. Copyright©2017, Philippe JOSEPH. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. -

Universidade Federal De Juiz De Fora Instituto De Ciências Biológicas Programa De Pós-Graduação Em Ciências Biológicas
UNIVERSIDADE FEDERAL DE JUIZ DE FORA INSTITUTO DE CIÊNCIAS BIOLÓGICAS PROGRAMA DE PÓS-GRADUAÇÃO EM CIÊNCIAS BIOLÓGICAS Rodrigo Luiz Fabri ESTUDO FITOQUÍMICO DE Mitracarpus frigidus (Willd. ex Reem Schult.) K. Schum. BIOMONITORADO PELA ATIVIDADE ANTIMICROBIANA E A AVALIAÇÃO DAS ATIVIDADES CITOTÓXICA, ANTIOXIDANTE E LEISHMANICIDA. Juiz de Fora, 2008. RODRIGO LUIZ FABRI ESTUDO FITOQUÍMICO DE Mitracarpus frigidus (Willd. ex Reem Schult.) K. Schum. BIOMONITORADO PELA ATIVIDADE ANTIMICROBIANA E A AVALIAÇÃO DAS ATIVIDADES CITOTÓXICA, ANTIOXIDANTE E LEISHMANICIDA. Dissertação de Mestrado do Curso de Pós-graduação em Ciências Biológicas, para obtenção do Título de Mestre em Ciências Biológicas na área de Genética e Biotecnologia. Orientadora: Dra. Elita Scio Fontes Juiz de Fora, 2008. FABRI, R.L. Estudo fitoquímico de Mitracarpus frigidus (Willd. ex Reem Schult.) K. Schum. biomonitorado pela atividade antimicrobiana e a avaliação das atividades citotóxica, antioxidante e leishmanicida. Juiz de Fora (MG), 2007. 140 f. Dissertação de Mestrado (Curso de Pós- Graduação em Ciências Biológicas) – Instituto de Ciências Biológicas, Universidade Federal de Juiz de Fora). Esta dissertação intitulada: “ESTUDO FITOQUÍMICO DE Mitracarpus frigidus (Willd. ex Reem Schult.) K. Schum. BIOMONITORADO PELA ATIVIDADE ANTIMICROBIANA E AVALIAÇÃO DAS ATIVIDADES CITOTÓXICA, LEISHMANICIDA E ANTIOXIDANTE”. Apresentada por RODRIGO LUIZ FABRI Foi avaliada pela banca examinadora composta pelos seguintes membros: Prof. Dr. Adilson David da Silva (Departamento de Química/UFJF) Prof. Dra. Luciana Moreira Chedier (Universidade Presidente Antônio Carlos/JF) Fevereiro, 2008. Dedico este trabalho a meus pais, ao meu irmão Rafael, a minha noiva Angélica e todos meus familiares.. AGRADECIMENTOS A Deus por permitir a realização de mais um sonho. À minha orientadora Doutora Elita Scio Fontes, muito obrigado pela oportunidade. -

Survey of Rubiaceae in the Golfo Dulce Area, Costa Rica
ZOBODAT - www.zobodat.at Zoologisch-Botanische Datenbank/Zoological-Botanical Database Digitale Literatur/Digital Literature Zeitschrift/Journal: Stapfia Jahr/Year: 2008 Band/Volume: 0088 Autor(en)/Author(s): Will Sabine, Kiehn Michael Artikel/Article: Survey of Rubiaceae in the Golfo Dulce area, Costa Rica: new species, combinations and name changes since 2001 111-120 © Biologiezentrum Linz/Austria; download unter www.biologiezentrum.at Survey of Rubiaceae in the Golfo Dulce area, Costa Rica: new species, combinations and name changes since 2001 Investigaciones en Rubiaceae en el área de Golfo Dulce, Costa Rica: nuevas especies, combinaciones y cambios de nombre desde 2001 S abine W ILL &Michael K IEHN Abstract: Since the publication of the last Rubiaceae treatment of the Golfo Dulce area in southern Costa Rica (WILL et al. 2001a), several new taxa have been described and changes in generic and species level within the family have been made. The new species, combinations and name changes are presented here and a new checklist of the Rubiaceae for the region is provided. Key words: Costa Rica, Golfo Dulce, Rubiaceae, checklist. Resumen: Desde la última publicación de Rubiaceas del área del Golfo Dulce en la zona Sur de Costa Rica (WILL et al. 2001a), nuevos taxa han sido descritos y también se han realizado cambios a nivel génerico y específico dentro de la familia. En esta re- visión se presentan las nuevas especies, combinaciones y cambios de nombre, así como la lista actualizada de las Rubiaceas de la región. Palabras clave: Costa Rica, Golfo Dulce, Rubiaceae, lista actualizada. Introduction green forests and wet rainforests, up to dry forests and desert environments. -
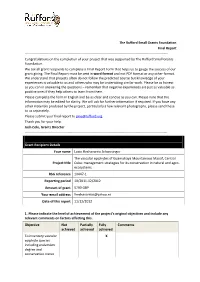
The Rufford Small Grants Foundation Final Report ------Congratulations on the Completion of Your Project That Was Supported by the Rufford Small Grants Foundation
The Rufford Small Grants Foundation Final Report ------------------------------------------------------------------------------------------------------------------------------- Congratulations on the completion of your project that was supported by The Rufford Small Grants Foundation. We ask all grant recipients to complete a Final Report Form that helps us to gauge the success of our grant giving. The Final Report must be sent in word format and not PDF format or any other format. We understand that projects often do not follow the predicted course but knowledge of your experiences is valuable to us and others who may be undertaking similar work. Please be as honest as you can in answering the questions – remember that negative experiences are just as valuable as positive ones if they help others to learn from them. Please complete the form in English and be as clear and concise as you can. Please note that the information may be edited for clarity. We will ask for further information if required. If you have any other materials produced by the project, particularly a few relevant photographs, please send these to us separately. Please submit your final report to [email protected]. Thank you for your help. Josh Cole, Grants Director ------------------------------------------------------------------------------------------------------------------------------ Grant Recipient Details Your name Lucia Hechavarria Schwesinger The vascular epiphytes of Guamuhaya Mountainous Massif, Central Project title Cuba: management strategies for its conservation in natural and agro- ecosystems. RSG reference 10447-1 Reporting period 10/2011-12/2012 Amount of grant 5790 GBP Your email address [email protected] Date of this report 11/12/2012 1. Please indicate the level of achievement of the project’s original objectives and include any relevant comments on factors affecting this. -

Search Results Help:Searching
Search results Help:Searching "is derived from the greek word" • Chrysovirus viruses which infect fungi, in particular Penicillium. Their name is derived from the Greek word chrysos which means yellow-green. There are currently nine species 3 KB (227 words) - 17:21, 26 June 2015 • Nanoviridae Diseases associated with this family include: stunting. Their name is derived from the Greek word 'nano (dwarf) because of their small genome and their stunting 5 KB (388 words) - 05:39, 1 July 2015 • Paizo Publishing community. The CEO of Paizo is Lisa Stevens. The company's name is derived from the Greek word παίζω paizō, which means 'I play' or 'to play'. Paizo formerly 6 KB (575 words) - 05:38, 20 July 2014 • Eidophor projector used to create theater-sized images. The name Eidophor is derived from the Greek word-roots ‘eido’ and ‘phor’ meaning 'image' and 'bearer' (carrier) 6 KB (695 words) - 22:59, 28 June 2015 • Somatic cell types of somatic cells in the human body. The word "somatic" is derived from the Greek word sōma, meaning "body". As multicellularity evolved many times 5 KB (710 words) - 05:01, 28 May 2015 • Dendron, Limpopo health committee. Laid out on the farm Duitsland. The name is derived from the Greek word for ‘tree’ and refers to the abundance of indigenous trees in 1 KB (75 words) - 11:12, 24 December 2013 • Ampelopsis of climbing shrubs, in the grape family Vitaceae. The name is derived from the Greek word ampelos, which means "vine". The genus was named in 1803. 6 KB (391 words) - 21:22, 26 June 2015 • Giga- (short-form) billion (109 or 1000000000).