Medicationsmedications
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

What's the Best First Line Anticonvulsant?
What’s the best first line anticonvulsant? Stephen Hanson, DVM, MS, Dip. ACVIM (Neurology) Recurring seizure activity is a relatively common problem in canine patients. Nowadays, there are several good options for medical treatment, which makes the choice of which drug to use a little more complicated. All anticonvulsant drugs have advantages and disadvantages, so the selection of a first-line drug should be tailored for the individual patient and client. Phenobarbital: This has been the standard first choice drug for decades. The nice thing about Phenobarbital is that it works fairly well, controlling seizures in about 70% of dogs with epilepsy. Also, it is inexpensive and readily available. The biggest down-sides are its induction of hepatic metabolism and the need for frequent upward dose adjustments, as well as its potential to cause hepatotoxicity. The potential for liver disease increases with time, so a 2 year old dog placed on this medication is more likely to develop hepatotoxicity in his life-time than a 10 year old dog. Phenobarbital can also cause sedation and ataxia. While this is usually mild/transient, it can be a real problem in dogs with other pre- existing signs of intracranial disease. Polyuria, polydipsia and polyphagia are other common side effects. These signs vary widely in severity between patients. Pros: cheap, available at any corner pharmacy, works well Cons: higher doses required with time, possible serious liver side-effects Good first-line choice for middle-aged to older dogs without any pre-existing liver issues Poor choice for dogs with liver disease, dogs with other intracranial signs Questionable choice for young epileptic dogs Potassium/sodium bromide: This was the most commonly-used add on anticonvulsant drug for a long time. -

22 Psychiatric Medications for Monitoring in Primary Care
22 Psychiatric Medications for Monitoring in Primary Care Medication Warnings, Precautions, and Adverse Events Comments Class: SSRI Fluvoxamine Boxed Warnings: Suicidality Used much less than SSRIs in the group of eight Indications: Warnings and Precautions: Similar to other SSRIs medications for prescribing, probably because it has no Adult: OCD Adverse Events: Similar to other SSRIs FDA indication for MDD or any anxiety disorder. Still Child/Adolescent: OCD (10-17 years) somewhat popular as a medication for OCD. Uses: Anxiety, OCD Monitoring: Same as other SSRIs Citalopram Boxed Warning: Suicidality. Escitalopram, one of the SSRIs in the group of Indications: Warnings and Precautions: Similar to other SSRIs medications for prescribing, is an active metabolite of Adult: MDD Adverse Events: Similar to other SSRIs citalopram. Escitalopram reportedly has fewer AEs and Child/Adolescent: None less interaction with hepatic metabolic enzymes than Uses: Anxiety, MDD, OCD citalopram but is otherwise essentially identical. Citalopram offers no advantage other than price, as Monitoring: Same as other SSRIs escitalopram is branded until 2012. Paroxetine Boxed Warnings: Suicidality. Paroxetine used much less than the SSRIs for Indications: Warnings and Precautions: Similar to other SSRIs prescribing, probably because of its nonlinear kinetics. Adult: MDD, OCD, Panic Disorder, Generalized Anxiety Adverse Events: Similar to other SSRIs A study of children and adolescents showed doubling Disorder, Social Anxiety Disorder, Posttraumatic Stress Disorder the dose of paroxetine from 10 mg/day to 20 mg/day Child/Adolescent: None resulted in a 7-fold increase in blood levels (Findling et Uses: Anxiety, MDD, OCD al, 1999). Thus, once metabolic enzymes are saturated, paroxetine levels can increase dramatically with dose Monitoring: Same as other SSRIs increases and decrease dramatically with dose decreases, sometimes leading to adverse events. -

Drugs That Can Cause Delirium (Anticholinergic / Toxic Metabolites)
Drugs that can Cause Delirium (anticholinergic / toxic metabolites) Deliriants (drugs causing delirium) Prescription drugs . Central acting agents – Sedative hypnotics (e.g., benzodiazepines) – Anticonvulsants (e.g., barbiturates) – Antiparkinsonian agents (e.g., benztropine, trihexyphenidyl) . Analgesics – Narcotics (NB. meperidine*) – Non-steroidal anti-inflammatory drugs* . Antihistamines (first generation, e.g., hydroxyzine) . Gastrointestinal agents – Antispasmodics – H2-blockers* . Antinauseants – Scopolamine – Dimenhydrinate . Antibiotics – Fluoroquinolones* . Psychotropic medications – Tricyclic antidepressants – Lithium* . Cardiac medications – Antiarrhythmics – Digitalis* – Antihypertensives (b-blockers, methyldopa) . Miscellaneous – Skeletal muscle relaxants – Steroids Over the counter medications and complementary/alternative medications . Antihistamines (NB. first generation) – diphenhydramine, chlorpheniramine). Antinauseants – dimenhydrinate, scopolamine . Liquid medications containing alcohol . Mandrake . Henbane . Jimson weed . Atropa belladonna extract * Requires adjustment in renal impairment. From: K Alagiakrishnan, C A Wiens. (2004). An approach to drug induced delirium in the elderly. Postgrad Med J, 80, 388–393. Delirium in the Older Person: A Medical Emergency. Island Health www.viha.ca/mhas/resources/delirium/ Drugs that can cause delirium. Reviewed: 8-2014 Some commonly used medications with moderate to high anticholinergic properties and alternative suggestions Type of medication Alternatives with less deliriogenic -

Chapter 25 Mechanisms of Action of Antiepileptic Drugs
Chapter 25 Mechanisms of action of antiepileptic drugs GRAEME J. SILLS Department of Molecular and Clinical Pharmacology, University of Liverpool _________________________________________________________________________ Introduction The serendipitous discovery of the anticonvulsant properties of phenobarbital in 1912 marked the foundation of the modern pharmacotherapy of epilepsy. The subsequent 70 years saw the introduction of phenytoin, ethosuximide, carbamazepine, sodium valproate and a range of benzodiazepines. Collectively, these compounds have come to be regarded as the ‘established’ antiepileptic drugs (AEDs). A concerted period of development of drugs for epilepsy throughout the 1980s and 1990s has resulted (to date) in 16 new agents being licensed as add-on treatment for difficult-to-control adult and/or paediatric epilepsy, with some becoming available as monotherapy for newly diagnosed patients. Together, these have become known as the ‘modern’ AEDs. Throughout this period of unprecedented drug development, there have also been considerable advances in our understanding of how antiepileptic agents exert their effects at the cellular level. AEDs are neither preventive nor curative and are employed solely as a means of controlling symptoms (i.e. suppression of seizures). Recurrent seizure activity is the manifestation of an intermittent and excessive hyperexcitability of the nervous system and, while the pharmacological minutiae of currently marketed AEDs remain to be completely unravelled, these agents essentially redress the balance between neuronal excitation and inhibition. Three major classes of mechanism are recognised: modulation of voltage-gated ion channels; enhancement of gamma-aminobutyric acid (GABA)-mediated inhibitory neurotransmission; and attenuation of glutamate-mediated excitatory neurotransmission. The principal pharmacological targets of currently available AEDs are highlighted in Table 1 and discussed further below. -

Headshop Highs & Lows
HeadshopHeadshop HighsHighs && LowsLows AA PresentationPresentation byby DrDr DesDes CorriganCorrigan HeadshopsHeadshops A.K.A.A.K.A. ““SmartSmart ShopsShops””,, ““HempHemp ShopsShops””,, ““HemporiaHemporia”” oror ““GrowshopsGrowshops”” RetailRetail oror OnlineOnline OutletsOutlets sellingselling PsychoactivePsychoactive Plants,Plants, ‘‘LegalLegal’’ && ““HerbalHerbal”” HighsHighs asas wellwell asas DrugDrug ParaphernaliaParaphernalia includingincluding CannabisCannabis growinggrowing equipment.equipment. Headshops supply Cannabis Paraphernalia HeadshopsHeadshops && SkunkSkunk--typetype (( HighHigh Strength)Strength) CannabisCannabis 1.1. SaleSale ofof SkunkSkunk--typetype seedsseeds 2.2. AdviceAdvice onon SinsemillaSinsemilla TechniqueTechnique 3.3. SaleSale ofof HydroponicsHydroponics && IntenseIntense LightingLighting .. CannabisCannabis PotencyPotency expressedexpressed asas %% THCTHC ContentContent ¾¾ IrelandIreland ¾¾ HerbHerb 6%6% HashHash 4%4% ¾¾ UKUK ¾¾ HerbHerb** 1212--18%18% HashHash 3.4%3.4% ¾¾ NetherlandsNetherlands ¾¾ HerbHerb** 20%20% HashHash 37%37% * Skunk-type SkunkSkunk--TypeType CannabisCannabis && PsychosisPsychosis ¾¾ComparedCompared toto HashHash smokingsmoking controlscontrols ¾¾ SkunkSkunk useuse -- 77 xx riskrisk ¾¾ DailyDaily SkunkSkunk useuse -- 1212 xx riskrisk ¾¾ DiDi FortiForti etet alal .. Br.Br. J.J. PsychiatryPsychiatry 20092009 CannabinoidsCannabinoids ¾¾ PhytoCannabinoidsPhytoCannabinoids-- onlyonly inin CannabisCannabis plantsplants ¾¾ EndocannabinoidsEndocannabinoids –– naturallynaturally occurringoccurring -

DEMAND REDUCTION a Glossary of Terms
UNITED NATIONS PUBLICATION Sales No. E.00.XI.9 ISBN: 92-1-148129-5 ACKNOWLEDGEMENTS This document was prepared by the: United Nations International Drug Control Programme (UNDCP), Vienna, Austria, in consultation with the Commonwealth of Health and Aged Care, Australia, and the informal international reference group. ii Contents Page Foreword . xi Demand reduction: A glossary of terms . 1 Abstinence . 1 Abuse . 1 Abuse liability . 2 Action research . 2 Addiction, addict . 2 Administration (method of) . 3 Adverse drug reaction . 4 Advice services . 4 Advocacy . 4 Agonist . 4 AIDS . 5 Al-Anon . 5 Alcohol . 5 Alcoholics Anonymous (AA) . 6 Alternatives to drug use . 6 Amfetamine . 6 Amotivational syndrome . 6 Amphetamine . 6 Amyl nitrate . 8 Analgesic . 8 iii Page Antagonist . 8 Anti-anxiety drug . 8 Antidepressant . 8 Backloading . 9 Bad trip . 9 Barbiturate . 9 Benzodiazepine . 10 Blood-borne virus . 10 Brief intervention . 11 Buprenorphine . 11 Caffeine . 12 Cannabis . 12 Chasing . 13 Cocaine . 13 Coca leaves . 14 Coca paste . 14 Cold turkey . 14 Community empowerment . 15 Co-morbidity . 15 Comprehensive Multidisciplinary Outline of Future Activities in Drug Abuse Control (CMO) . 15 Controlled substance . 15 Counselling and psychotherapy . 16 Court diversion . 16 Crash . 16 Cross-dependence . 17 Cross-tolerance . 17 Custody diversion . 17 Dance drug . 18 Decriminalization or depenalization . 18 Demand . 18 iv Page Demand reduction . 19 Dependence, dependence syndrome . 19 Dependence liability . 20 Depressant . 20 Designer drug . 20 Detoxification . 20 Diacetylmorphine/Diamorphine . 21 Diuretic . 21 Drug . 21 Drug abuse . 22 Drug abuse-related harm . 22 Drug abuse-related problem . 22 Drug policy . 23 Drug seeking . 23 Drug substitution . 23 Drug testing . 24 Drug use . -

The Psychoactive Effects of Psychiatric Medication: the Elephant in the Room
Journal of Psychoactive Drugs, 45 (5), 409–415, 2013 Published with license by Taylor & Francis ISSN: 0279-1072 print / 2159-9777 online DOI: 10.1080/02791072.2013.845328 The Psychoactive Effects of Psychiatric Medication: The Elephant in the Room Joanna Moncrieff, M.B.B.S.a; David Cohenb & Sally Porterc Abstract —The psychoactive effects of psychiatric medications have been obscured by the presump- tion that these medications have disease-specific actions. Exploiting the parallels with the psychoactive effects and uses of recreational substances helps to highlight the psychoactive properties of psychi- atric medications and their impact on people with psychiatric problems. We discuss how psychoactive effects produced by different drugs prescribed in psychiatric practice might modify various disturb- ing and distressing symptoms, and we also consider the costs of these psychoactive effects on the mental well-being of the user. We examine the issue of dependence, and the need for support for peo- ple wishing to withdraw from psychiatric medication. We consider how the reality of psychoactive effects undermines the idea that psychiatric drugs work by targeting underlying disease processes, since psychoactive effects can themselves directly modify mental and behavioral symptoms and thus affect the results of placebo-controlled trials. These effects and their impact also raise questions about the validity and importance of modern diagnosis systems. Extensive research is needed to clarify the range of acute and longer-term mental, behavioral, and physical effects induced by psychiatric drugs, both during and after consumption and withdrawal, to enable users and prescribers to exploit their psychoactive effects judiciously in a safe and more informed manner. -

Guidance on the Use of Mood Stabilizers for the Treatment of Bipolar Affective Disorder Version 2
Guidance on the use of mood stabilizers for the treatment of bipolar affective disorder Version 2 RATIFYING COMMITTEE DRUGS AND THERAPEUTICS GROUP DATE RATIFIED July 2015 REPLACES Version 1 dated July 2013 NEXT REVIEW DATE July 2017 POLICY AUTHORS Jules Haste, Lead Pharmacist, Brighton and Hove Members of the Pharmacy Team (contributors are listed overleaf) If you require this document in an alternative format, i.e. easy read, large text, audio or Braille please contact the pharmacy team on 01243 623349 Page 1 of 49 Contributors Jed Hewitt, Chief Pharmacist - Governance & Professional Practice James Atkinson, Pharmacist Team Leader Mental Health and Community Services Miguel Gomez, Lead Pharmacist, Worthing. Hilary Garforth, Lead Pharmacist, Chichester. Pauline Daw, Lead Pharmacist (CRHTs & AOT), East Sussex. Iftekhar Khan, Lead Pharmacist (S&F Service), East Sussex. Graham Brown, Lead Pharmacist CAMHS & EIS. Gus Fernandez, Specialist Pharmacist MI and MH Lisa Stanton, Specialist Pharmacist Early Intervention Services & Learning Disabilities. Nana Tomova, Specialist Pharmacist, Crawley. Page 2 of 49 Section Title Page Number Introduction and Key Points 4 1. General principles in the treatment of acute mania 6 2. General principles in the treatment of bipolar depression 8 3. General principles in long term treatment 10 4. Rapid cycling 13 5. Physical health 13 6. Treatment in special situations 6.1 Pregnancy 15 6.2 Breast-feeding 17 6.3 Older adults 19 6.4 Children and adolescents 22 6.5 Learning disabilities 29 6.6 Cardiac dysfunction 30 6.7 Renal dysfunction 34 6.8 Hepatic dysfunction 37 6.9 Epilepsy 41 7. The risk of switching to mania with antidepressants 43 8. -

Homicide and Associated Steroid Acute Psychosis: a Case Report
Hindawi Publishing Corporation Case Reports in Medicine Volume 2011, Article ID 564521, 4 pages doi:10.1155/2011/564521 Case Report Homicide and Associated Steroid Acute Psychosis: A Case Report G. Airagnes,1, 2 C. Rouge-Maillart,1, 3 J.-B. Garre,2, 3 and B. Gohier2 1 Service de M´edecine L´egale, CHU d’Angers, 49933 Angers Cedex 09, France 2 D´epartement de Psychiatrie et de Psychologie m´edicale, CHU d’Angers, 49933 Angers Cedex 09, France 3 IFR 132, Universit´e d’Angers, 49035 Angers, France Correspondence should be addressed to G. Airagnes, [email protected] Received 22 June 2011; Revised 26 August 2011; Accepted 26 September 2011 Academic Editor: Massimo Gallerani Copyright © 2011 G. Airagnes et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. We report the case of an old man treated with methylprednisolone for chronic lymphoid leukemia. After two months of treatment, he declared an acute steroid psychosis and beat his wife to death. Steroids were stopped and the psychotic symptoms subsided, but his condition declined very quickly. The clinical course was complicated by a major depressive disorder with suicidal ideas, due to the steroid stoppage, the leukemia progressed, and by a sudden onset of a fatal pulmonary embolism. This clinical case highlights the importance of early detection of steroid psychosis and proposes, should treatment not be stopped, a strategy of dose reduction combined with a mood stabilizer or antipsychotic treatment. -
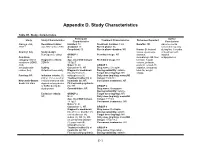
Appendix D. Study Characteristics
Appendix D. Study Characteristics Table D1. Study characteristics Participant Author Study Study Characteristics Treatment Characteristics Outcomes Reported Characteristics Conclusions Alacqua et al., Recruitment dates: Enrolled: 73 Treatment duration: 3 mo Benefits: NR Adverse events 2008 96 Jan 2002 to Dec 2003 Analyzed: 73 Run-in phase: No occurred frequently Completed: 50 Run-in phase duration: NR Harms: Behavioral during first 3 months Country: Italy Study design: issues, dyskinesia, of treatment with Retrospective cohort GROUP 1 Permitted drugs: NR dystonia, atypical Condition N: 2 dermatologic AE, liver antipsychotics. category: Mixed Diagnostic criteria: Age, mean±SD (range): Prohibited drugs: NR function, hepatic conditions (ADHD, DSM-IV 15.5±0.7 volume, prolactin, ASD, Males %: 50 GROUP 1 prolactin-related AE, schizophrenia- Setting: Caucasian %: NR Drug name: Clozapine sedation, sleepness, related, tics) Outpatient/community Diagnostic breakdown Dosing variability: variable total AE, weight (n): psychosis (1), Target dose (mg/day): NR change Funding: NR Inclusion criteria: (1) schizophrenia (1) Daily dose (mg/day), mean±SD ≤18 yr, (2) received an Treatment naïve (n): all (range): 150±70.1 Newcastle-Ottawa incident treatment with Inpatients (n): NR Concurrent treatments: NR Scale: 6/8 stars atypical antipsychotics First episode psychosis or SSRIs during the (n): NR GROUP 2 study period Comorbidities: NR Drug name: Olanzapine Dosing variability: variable Exclusion criteria: GROUP 2 Target dose (mg/day): NR NR N: 24 Daily dose -

Neurosteroid Metabolism in the Human Brain
European Journal of Endocrinology (2001) 145 669±679 ISSN 0804-4643 REVIEW Neurosteroid metabolism in the human brain Birgit Stoffel-Wagner Department of Clinical Biochemistry, University of Bonn, 53127 Bonn, Germany (Correspondence should be addressed to Birgit Stoffel-Wagner, Institut fuÈr Klinische Biochemie, Universitaet Bonn, Sigmund-Freud-Strasse 25, D-53127 Bonn, Germany; Email: [email protected]) Abstract This review summarizes the current knowledge of the biosynthesis of neurosteroids in the human brain, the enzymes mediating these reactions, their localization and the putative effects of neurosteroids. Molecular biological and biochemical studies have now ®rmly established the presence of the steroidogenic enzymes cytochrome P450 cholesterol side-chain cleavage (P450SCC), aromatase, 5a-reductase, 3a-hydroxysteroid dehydrogenase and 17b-hydroxysteroid dehydrogenase in human brain. The functions attributed to speci®c neurosteroids include modulation of g-aminobutyric acid A (GABAA), N-methyl-d-aspartate (NMDA), nicotinic, muscarinic, serotonin (5-HT3), kainate, glycine and sigma receptors, neuroprotection and induction of neurite outgrowth, dendritic spines and synaptogenesis. The ®rst clinical investigations in humans produced evidence for an involvement of neuroactive steroids in conditions such as fatigue during pregnancy, premenstrual syndrome, post partum depression, catamenial epilepsy, depressive disorders and dementia disorders. Better knowledge of the biochemical pathways of neurosteroidogenesis and -

Mechanism of Action of Antidepressants and Mood Stabilizers
79 MECHANISM OF ACTION OF ANTIDEPRESSANTS AND MOOD STABILIZERS ROBERT H. LENOX ALAN FRAZER Bipolar disorder (BPD), the province of mood stabilizers, the more recent understanding that antidepressants share has long been considered a recurrent disorder. For more this property in UPD have focused research on long-term than 50 years, lithium, the prototypal mood stabilizer, has events, such as alterations in gene expression and neuroplas- been known to be effective not only in acute mania but ticity, that may play a significant role in stabilizing the clini- also in the prophylaxis of recurrent episodes of mania and cal course of an illness. In our view, behavioral improvement depression. By contrast, the preponderance of past research and stabilization stem from the acute pharmacologic effects in depression has focused on the major depressive episode of antidepressants and mood stabilizers; thus, both the acute and its acute treatment. It is only relatively recently that and longer-term pharmacologic effects of both classes of investigators have begun to address the recurrent nature of drugs are emphasized in this chapter. unipolar disorder (UPD) and the prophylactic use of long- term antidepressant treatment. Thus, it is timely that we address in a single chapter the most promising research rele- vant to the pharmacodynamics of both mood stabilizers and MOOD STABILIZERS antidepressants. As we have outlined in Fig. 79.1, it is possible to charac- The term mood stabilizer within the clinical setting is com- terize both the course and treatment of bipolar and unipolar monly used to refer to a class of drugs that treat BPD.