B-Solutions FINAL REPORT by the EXPERT
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Erkende Vermeerderingsbedrijven Datum Lijst: 17/03/2017 Deze Lijst Is Gesorteerd Op Erkenningsnummer Deze Lijst Bevat 121 Bedrijven
Gespecialiseerde pluimveebedrijven - Erkende vermeerderingsbedrijven Datum lijst: 17/03/2017 Deze lijst is gesorteerd op erkenningsnummer Deze lijst bevat 121 bedrijven Nr. Naam bedrijf Adres maatschappelijke zetel BE1103 ANTHONISSEN D. Tilburgbaan 38 2960 BRECHT BE1105 BOLCKMANS JAN Blauwbossen 22 2322 MINDERHOUT BE1106 BORGHS W. BVBA Langenberg 7 2460 KASTERLEE BE1108 NOEYENS-BROECKX Molenzicht 2 2380 RAVELS BE1109 CLAES LEO Bruine Kolk 42 2490 BALEN BE1110 COOLS JOS Gebergte 5 2450 MEERHOUT BE1113 DE BRUYN JOS Keirschot 15 2310 RIJKEVORSEL BE1114 KENIS RENÉ Leiweg 24 2990 LOENHOUT BE1122 GROETELAERS PLUIMVEE BVBA Heesdijk 15 2382 POPPEL BE1123 TIMMERMANS BVBA Langvenstraat 45 2300 TURNHOUT BE1126 KLAASEN FRANK BVBA Koningsstraat 80 2381 Weelde BE1127 KLAASEN & C° NV Peelsestraat 33 2380 RAVELS BE1135 MEEUSSEN W. Heistraat 32 2990 WUUSTWEZEL BE1136 MERTENS DIRK & THOMAS Molenstraat 26 2990 WUUSTWEZEL BE1139 MICHIELSEN G. Hal 29 2322 MINDERHOUT BE1142 BEL-EGG BVBA Galgenbergstraat 25 3950 BOCHOLT BE1143 VAN AKEREN MARIA Meir 34 2381 WEELDE BE1144 MOONEN NV Nieuwstraat 21 2382 POPPEL BE1147 VAN HERCK NICOLE Heizijde 172/1 2300 TURNHOUT BE1149 SCHELLEKENS E. Linieweg 42 2380 RAVELS BE1153 FRANSEN RIA Pannenhoef 10A 2382 POPPEL BE1155 DE BIE RIA St. Lenaertseweg 120 2990 LOENHOUT BE1161 VAN LOOVEREN J. Vaalmoer 2 2321 MEER BE1164 VERMEIREN DANNY Henxbroekweg 2 2990 LOENHOUT BE1169 ALJO BVBA Zondereigen 93 2387 BAARLE-HERTOG BE1172 KOYEN A. Schrieken 4 2340 BEERSE BE1174 ROMBOUTS FRANCIS Steertheuvel 20 2990 WUUSTWEZEL BE1175 ROMBOUTS GUY Molenheide 61 2990 WUUSTWEZEL BE1177 ROMBOUTS JAN Molenstraat 8 2990 WUUSTWEZEL BE1178 BVBA VAN BYSTERVELDT Leemputten 10 2381 RAVELS-WEELDE BE1179 VAN EYCK JAN Roerdompstraat 1 2440 GEEL BE1180 WILLEM SPOORMANS NV Schotelven 111 2370 ARENDONK BE1181 DE WITTE JEF B.V.B.A Goudbergstraat 3 2380 RAVELS BE1183 WILLEM SPOORMANS NV Schotelven 111 2370 ARENDONK BE1184 WILLEM SPOORMANS NV Schotelven 111 2370 ARENDONK BE1185 KLAASEN EN C° NV Peelsestraat 33 2380 RAVELS BE1188 VAN LOOVEREN J. -
Kalmthout Essen Stabroek
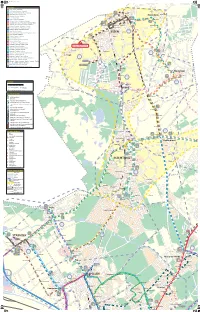
RF05_druk.pdf 1 8/21/2013 9:21:50 AM BUSLIJNEN RING 441 Essen - Wildert - Wuustwezel 442 Sint-Lenaarts - Wuustwezel - Kalmthout STEENPAAL Vaartstraat 444 Steenpaal 446 De Bijster 443 Sint-Job-in-’t-Goor - Maria-ter-Heide - Kalmthout 670 674 Kerkeneind HORENDONK Polikliniek 444 Wuustwezel - Maria-ter-Heide - Essen Mariaberg Horendonk Kerk WASBRUG GRENSSTRAAT Horendonk 445 Brasschaat - Gooreind - Kalmthout Hemelrijckweg Biblio- NIEUWSTR. SCHAM theek 444 446 447 446 Essen - Brecht - Malle 670 673 674 Over d'Aa Klooster- 679 KRAAIENBERG STATIONSSTR. Kleuterschool 447 Essen - Horendonk - Wuustwezel HEMELRIJKWEG straat Atheneum SCH Melkerijstraat 447 670 607 Sint-Job-in-’t-Goor - Sint-Antonius - Oostmalle A 444 446 674 673 679 MSE DIJK Eindhalte Gemeente- 640 Antwerpen - Brasschaat - Wuustwezel - Loenhout - Brecht Sint-Antoniusstraat huis KAPELSTRAAT 447 670 673 Essen STATIONSSTRAAT Sint-Jozef BOSDREEF 642 Antwerpen - Maria-ter-Heide via Brasschaat Miksebaan 679 OUDE BAAN Sint-Antonius- Molenstraat De Caernhoeve 648 Merksem - Brasschaat - Wuustwezel - Loenhout Station straat Spijker KER KRAAIENBERG SCHAN 649 Brasschaat - Wuustwezel - Hoogstraten scholen Domein Hemelrijk Sint-Antoniuskerk RINGELSHOEVE 650 Kapellen - Merksem - Antwerpen Luchtbal Schanker Kraaienberg Karrenmuseum ZONE 658 Putte - Kapellen - Merksem Dennenlaan N POSTBAAN IE 55 U VAARTKANT Oude Baan W NOORDENEIND 659 Ekeren Donk - Kapellen - Wuustwezel - Hoogstraten scholen ESSEN SPIJKER MO Sint-Michael E R 444 S Heemhuis E HEIKANTSTRAAT S VLEETWEG 444 446 T E 670 Essen - Kapellen -

Aalst Geel Lubbeek Stabroek Aalter Geraardsbergen Lummen STADEN
Aalst Geel Lubbeek Stabroek Aalter Geraardsbergen Lummen STADEN Aartselaar Grimbergen Maaseik Steenokkerzeel Alken Haacht Maldegem Temse Alveringem Hamme Mechelen Tervuren Anzegem Hamont-Achel Meerhout Tessenderlo Arendonk Harelbeke Meeuwen - Gruitrode Tielt-Winge As Hasselt Meise Tienen Assenede Heers Melle Tongeren Baarle-Hertog Heist-op-den-Berg Merchtem Tremelo Beerse Herent Merelbeke Veurne Beersel Herenthout Merksplas Vorselaar Bekkevoort Herk-de-Stad Meulebeke Vosselaar BERINGEN Herne Moerbeke Waarschoot Berlare Herzele Mol Waasmunster Bertem Hoegaarden Moorslede Wachtebeke BEVER Holsbeek Nazareth Wellen Beveren Hooglede Niel Wemmel Bierbeek Horebeke Nieuwerkerken Westerlo Bilzen Houthalen-Helchteren Nieuwpoort Wetteren Bocholt Houthulst Nijlen Wichelen Boechout Hove Ninove Wielsbeke Bonheiden Ieper Olen Willebroek Boom Ingelmunster Oosterzele Wingene Boortmeerbeek Izegem Opglabbeek Wommelgem Borgloon Kalmthout Oudenaarde Wortegem-Petegem Bornem Kapellen Oudenburg Wuustwezel Boutersem Kapelle-op-den-Bos Oud-Heverlee Zandhoven Brakel KASTERLEE Oud-Turnhout Zaventem Brecht knokke-heist Overijse Zedelgem Bree Koksijde Overpelt Zele BRUGGE Kontich Pittem Zelzate Buggenhout Kortenberg poperinge Zemst Damme Kortrijk Putte Zoersel De Pinte Kraainem Puurs Zonhoven Deinze Kruibeke Ranst Zottegem Dendermonde Kuurne Ravels Zulte Dessel Laakdal Riemst Zwalm Destelbergen Laarne Ronse ZWEVEGEM Diepenbeek Lanaken Ruiselede Zwijndrecht Diksmuide Landen Schelle Hoogstraten Dilbeek Langemark-Poelkapelle Schoten Genk Dilsen-Stokkem Lendelede Sint-Amands Kinrooi Drogenbos Lennik Sint-Gillis-Waas Neerpelt Duffel Liedekerke Sint-Laureins Herenthals Eeklo Lier Sint-Lievens-Houtem Balen Erpe-Mere Lille Sint-Martens-Latem Herselt Essen Linkebeek Sint-Niklaas Evergem Lint Sint-Pieters-Leeuw Galmaarden Lochristi Spiere-Helkijn. -

Gerechtelijk Arrondissement: Antwerpen Afdeling: Antwerpen
Gerechtelijk Arrondissement: Antwerpen LIJST VAN DE TAKELDIENSTEN DIE INGESTEMD HEBBEN MET DE VOORWAARDEN VERMELD IN DE OMZENDBRIEF NR 062 (20 JULI 2005) Afdeling: Antwerpen Laatste wijziging 26/03/2018 naam adres telefoon + fax Website / E-mail 1. NV Depannage 2000 Emiel Vloorsstraat 2 (03) 238 60 00 www.depannage2000.com 2660 Antwerpen (03) 248 18 05 [email protected] (Hoboken) 2. NV Depannage La France Tweemontstraat 310 (03) 325 19 15 www.depannagelafrance.be 2100 Antwerpen (03) 328 19 30 [email protected] (Deurne) 3. BVBA Internationale Takeldienst Viaene Kernenergiestraat 41 (03) 820 78 78 www.depannageviaene.com 2610 Wilrijk (03) 820 78 70 [email protected] 4. NV Autobedrijf Quirynen Turnhoutsebaan 433 (03) 309 14 24 [email protected] !! Alleen voor takelen en stalling 2970 Schilde (03) 309 14 45 bromfietsen en motorfietsen en het demonteren van opvoeronderdelen 5. BVBA Garage Delta Medelaar 116 (03) 384 10 08 www.garagedelta.be 2980 Zoersel (03) 384 10 09 [email protected] 6. Struyfs Gustaaf Grensstraat 41 (03) 484 50 39 [email protected] 2243 Zandhoven (03) 484 56 72 7. BVBA Luc Sanders Depannage Eikelstraat 34 (03) 666 64 65 www.lucsanders.be 2920 Kalmthout (03) 666 69 64 [email protected] 8. BVBA A.V.L. Van Laer Langestraat 56 (03) 484 31 06 [email protected] 2240 Zandhoven (03) 484 62 42 9. Autoschade Gunther Brocken BVBA Doornpark 102 – Zone C (03)296.70.65 [email protected] (ook takelen + 3.5t) 9120 Beveren-Waas 0475/56.50.20 [email protected] www.autoschadebrocken.be 10. -

Adressen Dagverzorgingscentra Conform Artikel 51 Provincie
Agentschap Zorg en Gezondheid Afdeling Woonzorg Koning Albert II-laan 35 bus 33, 1030 Brussel Tel. 02-553 35 09 Adressen dagverzorgingscentra conform artikel 51 Provincie Antwerpen AARTSELAAR Dossiernr.: 101.501.2 Erkenningsnr.: PE3295 NOAH Aartselaar Beheersinstantie Palmboomstraat 4 / 1 A2 2630 Aartselaar VZW Familiehulp tel. : 015 29 25 70 Koningsstraat 294 fax: 015 29 25 71 1210 Sint-Joost-ten-Node e-mail: [email protected] url: www.familiehulp.be Erkende capaciteit: 1 Einddatum: Onbepaalde duur Pagina 2 van 28 27-sep-2021 Agentschap Zorg en Gezondheid Afdeling Woonzorg Koning Albert II-laan 35 bus 33, 1030 Brussel Tel. 02-553 35 09 ARENDONK Dossiernr.: 110.502.2 Erkenningsnr.: PE2931 CADO Arendonk Beheersinstantie Vrijheid 100 2370 Arendonk VZW i-mens Thuishulp tel. : 0470 20 65 33 Sint-Jansstraat 30 fax: 02 515 03 08 1000 Brussel e-mail: [email protected] url: www.i-mens.be Erkende capaciteit: 1 Einddatum: Onbepaalde duur Pagina 3 van 28 27-sep-2021 Agentschap Zorg en Gezondheid Afdeling Woonzorg Koning Albert II-laan 35 bus 33, 1030 Brussel Tel. 02-553 35 09 BALEN Dossiernr.: 112.501.2 Erkenningsnr.: PE3122 CADO Balen Beheersinstantie Vaartstraat 165 2490 Balen VZW i-mens Thuishulp tel. : 0473 52 53 07 Sint-Jansstraat 30 fax: 014 40 98 99 1000 Brussel e-mail: [email protected] url: www.i-mens.be Erkende capaciteit: 1 Einddatum: Onbepaalde duur Pagina 4 van 28 27-sep-2021 Agentschap Zorg en Gezondheid Afdeling Woonzorg Koning Albert II-laan 35 bus 33, 1030 Brussel Tel. 02-553 35 09 BERLAAR Dossiernr.: 114.502.2 Erkenningsnr.: PE3007 NOAH Berlaar Beheersinstantie Pastorijstraat 2 2590 Berlaar VZW Familiehulp tel. -

(Pdf) Download
RESUME Tapiaco (pseudonym for Willi Smeuninx) Hasselt °03 08 1944. EDUCATION 1962 - '66: "Provinciaal Hoger Instituut voor Architectuur en Toegepaste Kunsten" (PHL University College for Architecture and Applied Arts) in Hasselt (speciality: graphic art, stained glass art and monumental art) directed by. H. Pauwels, R. Daniëls en J. Jans; 1968 - '72: "Koninklijke Academie voor Schone Kunsten" (The Royal Academy of Fine Arts) in Antwerp (free student painting art) directed by R. Meerbergen, J. Vaerten, F. De Bruyn, V. Dolphijn, W. Pas; 1969: “Akademie Vytvarnich Umeni in Prague” (Academy of Fine Arts) Specialization scholarship granted by the Flemish Ministry of Culture: painting art and lithography) directed by F. Jiroudek, Cepelak; 1979: "Vysoka Skola Umeleckoprumyslova" in Prague (Academy of Arts, Architecture and Design) (Research scholarship granted by the Flemish Ministry of Culture: glass art) directed by Libensky, Harcuba; 1979: Autodidact glass etching techniques. EXHIBITIONS Individual Exhibitions - 1964: August Cuppensbibliotheek (Library August Cuppens), Beringen (B) (Applied arts); - 1967: “Le Soutien aux Jeunes Peintres”(Support to Young Painters), Brussels (B); - 1968: Euro-Artes, Airport Deurne, Antwerp (B); - 1969: Klub 17-november University, Prague; - 1969: “Akademie Vutvarnich Umeni” (Academy of Fine Arts), Prague; - 1977: Gallery Hendrik De Braeckeleer, Antwerp (B); - 1977: Gallery Stijn, Hoboken (B); - 1977: Gallery Acantus, Hasselt (B); - 1984: Gallery Casino, Beringen (B) (Provincial Cultural Centre Limburg); - -

52 - the Enclaves and Counter-Enclaves of Baarle (B/NL) by Frank Jacobs December 12, 2006, 1:04 PM
52 - The Enclaves and Counter-enclaves of Baarle (B/NL) by Frank Jacobs December 12, 2006, 1:04 PM One of the unlikeliest complexes of enclaves and exclaves in the world is to be found on the Belgian-Dutch border, and is centred on Baarle. This town, while surrounded entirely by Dutch territory, consists of two separate administrative units, one of which is the Dutch commune of Baarle-Nassau, the other being the Belgian commune of Baarle-Hertog.For an exhaustive history, please visit this page of the Buffalo Ontology Site. That same story, more succinctly: here… The Belgian-Dutch border was established in the Maastricht Treaty of 1843, which mostly confirmed boundaries which were a few centuries old (as the separation of Belgium and the Netherlands has its origin in the religious wars of the 16th century). In the area around Baarle, it proved impossible to reach a definitive agreement. Instead, both governments opted to allocate nationality separately to each of the 5.732 parcels of land in the 50 km between border posts 214 and 215. These parcels ‘coagulated’ into a veritable archipelago of 20-odd Belgian exclaves in and around Baarle. In turn, some of these Belgian exclaves completely surround pieces of Dutch territory. Deliciously complicating this picture is a small enclave of Baarle-Nassau situated entirely within Belgium proper – and there’s even a Belgian parcel within a Dutch parcel within a Belgian enclave, which in turn is surrounded entirely by Dutch territory… Numerous attempts have been made throughout the centuries to (literally) rectify the situation, but they have obviously all failed – leaving the double entity of Baarle-Nassau/Baarle-Hertog with some absurd folklore. -

Beheerplan Bosreservaat Overheide
Beheerplan Bosreservaat Overheide AMINAL afdeling Bos & Groen 30 maart 2006 beheerplan 7304697 HASKONING BELGIUM BVBA Haskoning Belgium bvba Hanswijkdries 80 B-2800 Mechelen 015/40 56 56 Telefoon 015/40 56 57 Fax [email protected] E-mail www.royalhaskoning.com Internet Documenttitel Beheerplan Bosreservaat Overheide Verkorte documenttitel BHP/BRV Antwerpen/B&G/12/2003 Status beheerplan Datum 30 maart 2006 Projectnaam Projectnummer 7304697 Auteur(s) Opdrachtgever AMINAL afdeling Bos & Groen ir. Patrick Engels Referentie 7304697/R/GGE/Mech SAMENVATTING Het bosreservaat Overheide is ongeveer 30 ha groot en ligt in domeinbos. De Overheide ligt op de rechteroever van het riviertje de Aa, ten oosten van het dorp Weelde in de gemeente Ravels, in een grootschalig bos- en akkerlandschap, typisch voor de Noorderkempen. Enkel naar het zuiden sluit het boscomplex waartoe het bosreservaat behoort (ongeveer 200 ha) op een groot groengebied aan, domeinbos Ravels. In het westen, noorden en oosten is het omringd door sterk ontwaterd en bemest landbouwgebied. Centraal in het bosreservaat ligt een natuurlijke slenk op zandgrond, de Bogaert, waarlangs oppervlaktewater van het hogere landschap naar de Aa stroomt. Tot eind 19e eeuw werd die omringd door heide. Tussen 1870 en 1930 werden de drogere delen bebost: grotendeels met Grove den. Langsheen de Aa werden in een eikenbestand lijnaanplantingen van Zomereik opgenomen. Het zuidelijk deel van de slenk werd drooggelegd en in weiland omgezet, de rest werd bedijkt om er een vijver van te maken. De potentieel natuurlijke vegetatie in de bosbestanden van Overheide is een vochtige tot droge variant van eikenbos op arm en zuur zand (Betulo-Quercetum roboris en/of Fago-Quercetum). -

Rinus Van De Velde
RINUS VAN DE VELDE BIOGRAPHY 1983 Born in Leuven, Belgium Lives and works in Antwerp, Belgium EDUCATION 2010 Higher Institute of Fine Arts Flanders. Antwerp, Belgium 2006 Hogeschool Sint-Lukas. Antwerp, Belgium SELECTED SOLO EXHIBITIONS 2016 S.M.A.K. Ghent, Belgium (forthcoming) 2015 Tim Van Laere Gallery, Antwerp, Belgium (forthcoming) Paul Smith Showroom, London, UK Kunsthalle Sao Paulo, Brazil 2014 Galerie Zink Berlin, Germany Erasmus Gallery, University of Rotterdam, The Netherlands 2013 Tim Van Laere, Antwerp, Belgium CAC Malaga, Spain 2012 Patrick Painter Inc., Santa Monica, CA The Lost Bishop, Stedelijk Museum Schiedam, Netherlands Tegenboschvanvreden Gallery, Amsterdam, Netherlands 2011 Tim Van Laere Gallery, Antwerp, Belgium Moniquemeloche Gallery, Chicago, USA Artisanal House, New York, USA With Nothing but myself, Galerie Zink, Berlin, Germany 2010 Solo Project, Watou, Belgium Institut für zeitgenössische Kunst, Nürnberg, Germany Pocket Room, Antwerp, Belgium 2009 Art Basel Miami Beach, Art Positions, Miami, USA Gaining here is losing there, Be Part, Waregem, Belgium Interisland Terminal, Honolulu, Hawaii, USA Pocketroom, Antwerp, Belgium a rotating sculpture and the residues, Galerie Zink, Munich, Germany 2525 Michigan Ave., Unit B2, Santa Monica, CA USA 90404 T/ 310 264 5988 F/ 310 828 2532 www.patrickpainter.com 2008 William Crowder, 40 years of sculpture, S.M.A.K., Gent, Belgium okaal01, Antwerp, Belgium recent drawings, 1st Floor Gallery, Antwerp, Belgium 2007 Untitled Gallery, Antwerp, Belgium Gallery Boechout, Boechout, Belgium 2006 S&S Gallery, Antwerp, Belgium Bastart Gallery, Houthalen, Belgium 2005 existenzmaximum, Leuven, Belgium 2004 laureate art prize, Oud-Heverlee, Belgium SELECTED GROUP EXHIBITIONS 2015 Drawing Biennal 2015, Drawing Room, London, Great Britain The future = Beurssc50uwburg, Beursschouwbourg, Brussels, Belgium 2014 OPEN CORNER, CV Coleccion, Biblioteca Central de Cantabria, Santander, Spain HOGE HORIZON. -
Int Students Guide GENERAL.Pdf
Table of Content Welcome to Thomas More 5 Studying as an exchange student 30 1 Academic year and public holidays 30 University College 5 2 Public holidays 31 Thomas More - expect more 6 Words and phrases in Dutch 34 1 ASKING FOR HELP AND DIRECTIONS 34 Thomas More campuses 8 2 How to introduce yourself 34 3 WISH SOMEONE SOMETHING 35 Antwerp 8 4 SOLVING A MISUNDERSTANDING 35 Mechelen 9 5 EXPRESSIONS AND WORDS 36 Sint-Katelijne-Waver 10 Turnhout 11 Facilities 38 Vorselaar 12 1 International office 38 Geel 13 2 Student services (STIP) 38 Lier 14 3 Buddy programme 39 4 Network facilities 40 Belgium & Flanders 16 5 Student union 40 1 BELGIUM 16 6 Student card 41 2 Flanders 18 3 Higher education in Flanders 19 Practical information 22 1 Climate and clothing 22 2 Crime 22 3 Time 22 4 Using the phone 22 5 Mobile phone 22 6 Sockets 23 7 How to pay 23 8 Important phone numbers 23 9 Belgian cuisine 23 10 Transport 25 11 Health & insurance 28 12 Postal system in Belgium 28 Welcome to Thomas More University College Thomas More offers an exciting and diverse study environment where students can obtain international and intercultural competencies. We are happy to welcome you to in our university college. Our international office and student services (STIP) will ensure that your time at Thomas More is an unforgettable experience. It will be a pleasure for us to provide you with whatever assistance you need. We will not only provide practical assistance but also try to offer you a wide variety of fun and relaxing activities such as sight-seeing tours, sports and cultural activities. -

Gemeenten Roosendaal, Bergen Op Zoom, Halderberge, Etten-Leur, Moerdijk, Rucphen, Steenbergen, Woensdrecht En Zundert
persbericht Gemeenten Roosendaal, Bergen op Zoom, Halderberge, Etten-Leur, Moerdijk, Rucphen, Steenbergen, Woensdrecht en Zundert Datum: 1 maart 2018 Portefeuillehouder: Van Poppel Onderwerp: West Brabant West maakt grote stappen in goede Jeugdzorg ‘Handel alsof het je eigen kind is’ In december 2017 sloten de negen gemeenten Bergen op Zoom, Halderberge, Etten-Leur, Moerdijk, Roosendaal, Rucphen, Steenbergen, Woensdrecht en Zundert overeenkomsten met zeven zorgcombinaties jeugdzorg voor de hoog complexe zorg. Deze overeenkomsten zijn het resultaat van de nieuwe koers die de negen gemeenten sinds 2015 varen na de transitie in het sociaal domein. De zeven zorgcombinaties hebben slagvaardige ketens in de jeugdzorg gevormd die uitgaan van het belang van het kind. Geen aanbesteding In West Brabant West zijn grote stappen gemaakt in het resultaatgericht werken. In 2017 was de mogelijkheid om te kiezen voor de traditionele aanbesteding vanuit de gemeenten. Dat deden zij niet. Elke zorgaanbieder met passend aanbod kan nu opdrachten krijgen. Een groot aantal zorgaanbieders hebben zorgcombinaties gevormd waarmee zij een volledig aanbod kunnen bieden voor de hoog complexe zorg aan onze jeugd. Lef De wijze waarop de zorgaanbieders de samenwerking hebben gezocht met elkaar is vernieuwend en getuigt van lef. Zij zijn koploper in Nederland. Medewerkers op de werkvloer krijgen de ruimte voor het leveren van maatwerk aan cliënten. Dit alles kan alleen als alle partijen op elkaar durven vertrouwen. Deze nieuwe wijze van samenwerking roept natuurlijk in de praktijk vragen op waar antwoorden op gevonden moeten worden. Ook die oplossingen vinden zij samen; aan de overlegtafels. De vraag van het kind Het zorgstelsel in Bergen op Zoom, Halderberge, Etten-Leur, Moerdijk, Roosendaal, Rucphen, Steenbergen, Woensdrecht en Zundert is gericht op de vraag van de cliënt en niet op het aanbod van de zorgaanbieders. -

Study Visit in Antwerp – Local Context and Cultural Policies
Study visit in Antwerp – Local context and cultural policies 1. About the city Antwerp Number of inhabitants 516 000 Area in Km² 204,5 km2 Annual budget of the city 1 480 000 000 euro Annual budget for culture Total amount of 87 800 000 euro for buildings/equipment/overhead, exploitation/operation, staff. Divided into: • 35 200 000 euro: local cultural policies: libraries, cultural centra, • 16 000 000 euro: art policies: subsidies of opera, ballet, theatres, filharmonie,… • 36 600 000 euro: musea and cultural heritage The local/regional context Belgium, officially the Kingdom of Belgium is a small, densely populated country which covers an area of 30,528 square kilometres and has a population of about 11 million people. Belgium is a federal constitutional monarchy with a parliamentary system of governance. It is divided into three regions and three communities, that exist next to each other. Its two largest regions are the Dutch-speaking region of Flanders in the north and the French-speaking southern region of Wallonia. The Brussels-Capital Region, officially bilingual, is a mostly French-speaking enclave within the Flemish Region. A German-speaking Community exists in eastern Wallonia. Belgium's linguistic diversity and related political conflicts are reflected in its political history and complex system of government Antwerp is the most populous city in Flanders. Antwerp is on the River Scheldt, linked to the North Sea by the Westerschelde estuary. The Port of Antwerp is one of the biggest in the world, ranking second in Europe and within the top 20 globally. 1 Antwerp has long been an important city in the Low Countries, both economically and culturally, especially before the Spanish Fury (1576) in the Dutch Revolt.