Surveillance and Early Detection and Response Systems in Latvia
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Baltic Republics
FINNISH DEFENCE STUDIES THE BALTIC REPUBLICS A Strategic Survey Erkki Nordberg National Defence College Helsinki 1994 Finnish Defence Studies is published under the auspices of the National Defence College, and the contributions reflect the fields of research and teaching of the College. Finnish Defence Studies will occasionally feature documentation on Finnish Security Policy. Views expressed are those of the authors and do not necessarily imply endorsement by the National Defence College. Editor: Kalevi Ruhala Editorial Assistant: Matti Hongisto Editorial Board: Chairman Prof. Mikko Viitasalo, National Defence College Dr. Pauli Järvenpää, Ministry of Defence Col. Antti Numminen, General Headquarters Dr., Lt.Col. (ret.) Pekka Visuri, Finnish Institute of International Affairs Dr. Matti Vuorio, Scientific Committee for National Defence Published by NATIONAL DEFENCE COLLEGE P.O. Box 266 FIN - 00171 Helsinki FINLAND FINNISH DEFENCE STUDIES 6 THE BALTIC REPUBLICS A Strategic Survey Erkki Nordberg National Defence College Helsinki 1992 ISBN 951-25-0709-9 ISSN 0788-5571 © Copyright 1994: National Defence College All rights reserved Painatuskeskus Oy Pasilan pikapaino Helsinki 1994 Preface Until the end of the First World War, the Baltic region was understood as a geographical area comprising the coastal strip of the Baltic Sea from the Gulf of Danzig to the Gulf of Finland. In the years between the two World Wars the concept became more political in nature: after Estonia, Latvia and Lithuania obtained their independence in 1918 the region gradually became understood as the geographical entity made up of these three republics. Although the Baltic region is geographically fairly homogeneous, each of the newly restored republics possesses unique geographical and strategic features. -
Health Systems in Transition
61575 Latvia HiT_2_WEB.pdf 1 03/03/2020 09:55 Vol. 21 No. 4 2019 Vol. Health Systems in Transition Vol. 21 No. 4 2019 Health Systems in Transition: in Transition: Health Systems C M Y CM MY CY CMY K Latvia Latvia Health system review Daiga Behmane Alina Dudele Anita Villerusa Janis Misins The Observatory is a partnership, hosted by WHO/Europe, which includes other international organizations (the European Commission, the World Bank); national and regional governments (Austria, Belgium, Finland, Kristine Klavina Ireland, Norway, Slovenia, Spain, Sweden, Switzerland, the United Kingdom and the Veneto Region of Italy); other health system organizations (the French National Union of Health Insurance Funds (UNCAM), the Dzintars Mozgis Health Foundation); and academia (the London School of Economics and Political Science (LSE) and the Giada Scarpetti London School of Hygiene & Tropical Medicine (LSHTM)). The Observatory has a secretariat in Brussels and it has hubs in London at LSE and LSHTM) and at the Berlin University of Technology. HiTs are in-depth profiles of health systems and policies, produced using a standardized approach that allows comparison across countries. They provide facts, figures and analysis and highlight reform initiatives in progress. Print ISSN 1817-6119 Web ISSN 1817-6127 61575 Latvia HiT_2_WEB.pdf 2 03/03/2020 09:55 Giada Scarpetti (Editor), and Ewout van Ginneken (Series editor) were responsible for this HiT Editorial Board Series editors Reinhard Busse, Berlin University of Technology, Germany Josep Figueras, European -
All Latvia Cemetery List-Final-By First Name#2
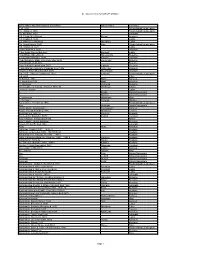
All Latvia Cemetery List by First Name Given Name and Grave Marker Information Family Name Cemetery ? d. 1904 Friedrichstadt/Jaunjelgava ? b. Itshak d. 1863 Friedrichstadt/Jaunjelgava ? b. Abraham 1900 Jekabpils ? B. Chaim Meir Potash Potash Kraslava ? B. Eliazar d. 5632 Ludza ? B. Haim Zev Shuvakov Shuvakov Ludza ? b. Itshak Katz d. 1850 Katz Friedrichstadt/Jaunjelgava ? B. Shalom d. 5634 Ludza ? bar Abraham d. 5662 Varaklani ? Bar David Shmuel Bombart Bombart Ludza ? bar Efraim Shmethovits Shmethovits Rezekne ? Bar Haim Kafman d. 5680 Kafman Varaklani ? bar Menahem Mane Zomerman died 5693 Zomerman Rezekne ? bar Menahem Mendel Rezekne ? bar Yehuda Lapinski died 5677 Lapinski Rezekne ? Bat Abraham Telts wife of Lipman Liver 1906 Telts Liver Kraslava ? bat ben Tzion Shvarbrand d. 5674 Shvarbrand Varaklani ? d. 1875 Pinchus Judelson d. 1923 Judelson Friedrichstadt/Jaunjelgava ? d. 5608 Pilten ?? Bloch d. 1931 Bloch Karsava ?? Nagli died 5679 Nagli Rezekne ?? Vechman Vechman Rezekne ??? daughter of Yehuda Hirshman 7870-30 Hirshman Saldus ?meret b. Eliazar Ludza A. Broido Dvinsk/Daugavpils A. Blostein Dvinsk/Daugavpils A. Hirschman Hirschman Rīga A. Perlman Perlman Windau Aaron Zev b. Yehiskiel d. 1910 Friedrichstadt/Jaunjelgava Aba Ostrinsky Dvinsk/Daugavpils Aba b. Moshe Skorobogat? Skorobogat? Karsava Aba b. Yehuda Hirshberg 1916 Hirshberg Tukums Aba Koblentz 1891-30 Koblentz Krustpils Aba Leib bar Ziskind d. 5678 Ziskind Varaklani Aba Yehuda b. Shrago died 1880 Riebini Aba Yehuda Leib bar Abraham Rezekne Abarihel?? bar Eli died 1866 Jekabpils Abay Abay Kraslava Abba bar Jehuda 1925? 1890-22 Krustpils Abba bar Jehuda died 1925 film#1890-23 Krustpils Abba Haim ben Yehuda Leib 1885 1886-1 Krustpils Abba Jehuda bar Mordehaj Hakohen 1899? 1890-9 hacohen Krustpils Abba Ravdin 1889-32 Ravdin Krustpils Abe bar Josef Kaitzner 1960 1883-1 Kaitzner Krustpils Abe bat Feivish Shpungin d. -

Madona, Varakļāni, MADONA Cesvaines, Ērgļu, Lubānas, Madonas, Varakļānu Novads
Cesvaine, Ērgļi, Lubāna, Madona, Varakļāni, MADONA Cesvaines, Ērgļu, Lubānas, Madonas, Varakļānu novads UZŅĒMUMI KARTES PAŠVALDĪBAS ETENS ETENS Ļ TNIECISKAIS BI TNIECISKAIS Ē P - VI Ī Mājaslapu izstrāde INFORMAT SEO risinājumi Mārketinga koncepti Sociālo tīklu profilu izveide nelieliem uzņēmumiem 2020/21 www.latvijastalrunis.lv 67770577 AKTUĀLAIS UN NOZĪMĪGAIS PORTĀLĀ ZIŅAS AFIŠA KATALOGS KARTE GALERIJAS SLUDINĀJUMI PAŠVALDĪBA Kur zvanīt steidzamos gadījumos?? 2 - 3 Uzziņas un pakalpojumi Pašvaldību informācija 4 - 15 Kartes, ielu saraksti, informācija 16 - 17 Uzņēmējdarbības vide 18 - 19 Alfabētiskais 20 - 28 nozaru saraksts Nozaru daļa 29 - 57 Firmu saraksts pēc to darbības sfēras Advokāti - Bankas 29 - 33 Būvuzraudzība… - Celtniecības… 34 - 35 Ceļu… - Daiļamatniecība 35 - 35 Dzīvnieku… - Ekonomikas… 37 - 37 Ēdināšanas… - Iepakojums… 37 - 39 Izglītība… - Jaunrades… 39 - 40 Juvelierizstrādājumi… - Kafija… 40 - 40 Ķīmiskā… - Labiekārtošana… 42 - 42 Lopkopība - Maize… 43 - 44 Mūzikas - Namu… 46 - 46 Notāri - Parfimērijas… 47 - 47 Putnkopība - Radio… 52 - 53 Rūpniecības… - Sabiedriskais… 53 - 53 Somas… - Tabakas… 54 - 54 Tūrisms… - Ugunsdzēsība… 55 - 55 Ūdensapgāde… - Valsts… 55 - 55 Viesnīcas… - Žalūzijas… 56 - 57 Firmas alfabētiskā secībā Mājaslapu izstrāde A - J 58 - 61 www.latvijastalrunis.lv Firmas alfabētiskā secībā 67770577 K - Z 61 - 68 Uzziņas un pakalpojumi KUR ZVANĪT STEIDZAMOS GADĪJUMOS? UGUNSDZĒSĪBA UN GLĀBŠANA 01, 112 POLICIJA 02, 110, 112 MEDICĪNISKĀ PALĪDZĪBA 03, 112, 113 Medicīniskā palīdzība Avārijas dienesti Madonas slimnīca -

Best Baltic Basketball League
BBBL – BEST BALTIC BASKETBALL LEAGUE BBBL is an international basketball tournament for boys & girls aged U10 to U16 (years of birth 2011-2005) BBBL is the biggest and fastest growing regular Youth basketball tournament in Europe • the tournament was founded in 2012 • since season 2019/2020 we have started also girls tournament and renamed league to BEST BALTIC BASKETBALL LEAGUE • season of 2019/2020, BBBL participates 306 teams from 13 countries ABOUT BBBL season 2019/2010 BBBL teams, season 2019/2020, by age groups 60 50 306 teams 40 13 countries 30 20 4300 players 10 0 boys boys boys boys boys boys boys girls U11 girls U12 girls U13 girls U14 U10 U11 U12 U13 U14 U15 U16 BBBL teams by countries, season 2019/2020 MOL UK DEN SWE POL GEO UKR BLR FIN LTU RUS EST LV 0 20 40 60 80 100 120 BBBL STAGE MAP STAGE LOCATIONS LATVIA – Riga, Ozolnieki, Valmiera, Cēsis, Sigulda, Madona, Tukums, Talsi, Ventspils ESTONIA – Tartu, Tallin, Kaarikuu, Viimsi, Saaremaa LITHUANIA – Vilnius, Mazeikiai, Siauliai BELARUS – Minsk RUSSIA – Moscow, Tula FINLAND - Nokia FINAL STAGES : Riga, Valmiera, Cesis, Jelgava, Tartu BBBL TOURNAMENT KEY & FUNNY FACTS season 2019/2020 till covid-19 lockdown • 1851 games / almost all live on YouTube channel • 4300 players / 13 countries • 132 stages / 25 different locations • some teams travel very far away to play in BBBL tournament Krasnoyarsk 5`070 km London 2`317 km number of teams per seasons Tbilisi 2`874 km 350 Odesa 1`519 km 300 250 • besides players and coaches BBBL 200 tournament attracts a lot of other guests 150 /sometimes team brings 40+ person delegation for the bbbl stage/ 100 50 0 2013 2014 2015 2016 2017 2018 2019 2020 BBBL TOURNAMENT KEY & FUNNY FACTS • BBBL it`s not just a games, it`s a basketball festival full of joy & positive emotions only youth basketball - Skills challenges tournament where every - 3-point shot contests game is provided with full - Coach challenges FIBA standard live statistics - Coach meetings etc. -

The Saeima (Parliament) Election
/pub/public/30067.html Legislation / The Saeima Election Law Unofficial translation Modified by amendments adopted till 14 July 2014 As in force on 19 July 2014 The Saeima has adopted and the President of State has proclaimed the following law: The Saeima Election Law Chapter I GENERAL PROVISIONS 1. Citizens of Latvia who have reached the age of 18 by election day have the right to vote. (As amended by the 6 February 2014 Law) 2.(Deleted by the 6 February 2014 Law). 3. A person has the right to vote in any constituency. 4. Any citizen of Latvia who has reached the age of 21 before election day may be elected to the Saeima unless one or more of the restrictions specified in Article 5 of this Law apply. 5. Persons are not to be included in the lists of candidates and are not eligible to be elected to the Saeima if they: 1) have been placed under statutory trusteeship by the court; 2) are serving a court sentence in a penitentiary; 3) have been convicted of an intentionally committed criminal offence except in cases when persons have been rehabilitated or their conviction has been expunged or vacated; 4) have committed a criminal offence set forth in the Criminal Law in a state of mental incapacity or a state of diminished mental capacity or who, after committing a criminal offence, have developed a mental disorder and thus are incapable of taking or controlling a conscious action and as a result have been subjected to compulsory medical measures, or whose cases have been dismissed without applying such compulsory medical measures; 5) belong -

Gradients of Latvian Magnetic Anomalies
Scientific Journal of Riga Technical University Sustainable Spatial Development 2011 __________________________________________________________________________________________________ Volume 2 Gradients of Latvian Magnetic Anomalies Vladimir Vertennikov, Riga Technical University Abstract. This article discusses one of the most important and vertical gradients. It is possible to determine those geophysical factors, which produces an impact on the gradients by calculations or measurements using special demographic processes and reflects the nature of variability in instruments – magnetic gradiometers. Instrumented gradient the anomalous magnetic field intensity in space. The article characterises the horizontal magnetic gradients, which vary measurements are predominantly utilised in local areas during within the wide range: from 10 to 2400 nT/km. It distinguishes prospecting and exploration for minerals. In regional magnetic scale and magnetic gradient areas. The article gives an investigations, to which concrete operations associated with ecodemographic evaluation of the territory of Latvia by the investigating the impact of geophysical factors on gradience of the anomalous magnetic field. demographic processes belong, horizontal gradients are the main factor; they are determined by calculations. Keywords: horizontal magnetic gradient, magnetic scale, magnetic gradient area, ecodemographic evaluation of territory by magnetic gradience. CHARACTERISATION OF HORIZONTAL MAGNETIC GRADIENTS The magnetic field is represented in the Latvian territory by a complex set of anomalies with different signs, intensity, size The gradient is an important parameter of anomalous and morphology. The transitions from one anomaly to another magnetic field. The discussion deals with the spatial intensity are expressed through changes in the field intensity and are variations. The thing is that the intensity of the anomalous either gradual, occurring step-by-step, or abrupt. -
CYCLING from KLAIPĖDA to RIGA (LITHUANIA – LATVIA) 8 Days / 7 Nights, Self-Guided (Code: SG3)
BALTIC BIKE TRAVEL Self-guided cycling tours 2021 CYCLING FROM KLAIPĖDA TO RIGA (LITHUANIA – LATVIA) 8 days / 7 nights, self-guided (code: SG3) A cycle tour through some of the most beautiful areas of Lithuania before crossing into Latvia to explore its hidden treasures. The journey begins by cycling along a famous Lithuanian route along the Baltic coast. The route continues through beautiful countryside in Latvia with its constantly changing landscape, small villages & old towns to end in the former Hanseatic port of Riga. Cycling grade: We rate this trip as moderate level. Cycle routes mainly on roads with little traffic and cycle paths, a few stretches in Latvia are on main roads with more car traffic, especially on weekends (from the Lithuanian border to Liepaja, and some stretches near Pavilosta and Tukums). Routes range from 30 to 78 km (19-49 miles) each day. Bicycle route is flat. CYCLING ITINERARY (cycling ~366 km / 229 miles, by train ~1 hour) Day 1. Klaipėda Individual arrival in Klaipėda and transfer to your hotel (not included). Hotel check-in. OVERNIGHT at central 3* Klaipėda hotel. Day 2. Klaipėda-Karklė-Palanga (appr. 30 km) Collect rental cycles at your hotel (if pre-ordered). Cycle on asphalt cycle path signposted as the Lithuanian Seaside Cycle Route through the Seaside Regional Park to Palanga resort, famous for its Botanical Park and Amber Museum. Arrive in Palanga, Hotel check-in. OVERNIGHT at central 4* Palanga hotel Day 3. Palanga-Nica-Liepaja (appr. 78 km) Cycle on picturesque cycle path along the Baltic Sea Coast to Šventoji where you’ll cross the river over a cable bridge. -

(UN/LOCODE) for Latvia
United Nations Code for Trade and Transport Locations (UN/LOCODE) for Latvia N.B. To check the official, current database of UN/LOCODEs see: https://www.unece.org/cefact/locode/service/location.html UN/LOCODE Location Name State Functionality Status Coordinatesi LV 6LV Alsunga 006 Road terminal; Recognised location 5659N 02134E LV AGL Aglona 001 Road terminal; Recognised location 5608N 02701E LV AIN Ainazi 054 Port; Code adopted by IATA or ECLAC 5752N 02422E LV AIZ Aizkraukle 002 Port; Rail terminal; Road terminal; Recognised location 5636N 02513E LV AKI Akniste JKB Road terminal; Multimodal function, ICD etc.; Recognised location 5610N 02545E LV ALJ Aloja 005 Road terminal; Recognised location 5746N 02452E LV AMT Amata 008 Road terminal; Recognised location 5712N 02509E LV APE Aizpute 003 Road terminal; Recognised location 5643N 02136E LV APP Ape 007 Road terminal; Recognised location 5732N 02640E LV ARX Avoti RIX Road terminal; Recognised location 5658N 02350E LV ASE Aluksne 002 Rail terminal; Road terminal; Recognised location 5725N 02703E LV AUC Auce 010 Rail terminal; Road terminal; Recognised location 5628N 02254E LV B8R Balozi 052 Road terminal; Recognised location 5652N 02407E LV B9G Baldone 013 Port; Road terminal; Recognised location 5644N 02423E LV BAB Babite 079 Road terminal; Recognised location 5657N 02357E LV BAL Balvi 015 Rail terminal; Road terminal; Recognised location 5708N 02715W LV BAU Bauska 016 Rail terminal; Road terminal; Recognised location 5624N 02411E LV BLN Baltinava 014 Road terminal; Recognised location -

Chapter 3 Chapter 3 Potential Analysis of Regional Development
CHAPTER 3 CHAPTER 3 POTENTIAL ANALYSIS OF REGIONAL DEVELOPMENT 3.1 National and Regional Policy on Socioeconomic Development 3.1.1 Review of Development Policy Latvia aims at ensuring equal working, income, social, and cultural opportunities for all inhabitants of the state, as mentioned in the following legislation, development strategies and policies. However, the former course of development after independence in 1991 has resulted in differences in living environment and opportunities of economic activity in different regions of Latvia. In many areas including LWC, insufficient economic development and activity, high unemployment rate, low income, unequal conditions for social and cultural life have been found. (1) Law on Spatial Development Planning of Latvia The Law on Spatial Development Planning of Latvia was adopted in October 1998. According to this new law, development and land use planning in Latvia is to be carried out, as such: - Local governments of districts, state cities, towns, and townships should prepare spatial development plans of their administrative areas, - Spatial development plans of higher level should be observed when producing spatial development plans of lower levels, and - Land use plans of regional and local municipal levels should be prepared in accordance with the relevant spatial development plans. Development and land use plans for LWC, therefore, has to observe and coordinate with the directions and strategies mentioned in the existing national, regional, district, and township level plans. (2) National development strategies The long-term goal of development strategy for Latvia is to become a socially harmonized country with a dynamic, open and equal opportunity as well as its own national identity. -

Latvia Country Report
m o c 50 km . s p m a o m c 50 km - 30 mi . d s p © a m - 30 mi d © Valmiera Ventspils Cē sis Talsi Gulbene Sigulda Jū rmala Kuldī ga Tukums Riga Salaspils Madona Olaine Ogre Saldus Dobele Jelgava Liepā ja Jē kabpils Rē zekne Bauska Krā slava Republic of Latvia Daugavpils Country Report Table of contents: Executive Summary ............................................................................................................................................. 2 Latvia’s transition to a Western-style political and economic model since regaining its independence in 1991 culminated in its 2004 accession to the EU and NATO. Overcoming an initial dependence on Russia, and various crises in the 1990s, Latvia has shown impressive economic growth since 2000. Read more. History ................................................................................................................................................................ 2 Latvia lies between its fellow Baltic states of Estonia and Lithuania, with Belarus and Russia to the east. The USSR annexed the country in 1940 and the Nazis occupied it during World War II. Up to 95% of the country’s Jewish population perished in the Holocaust. Read more. Domestic Situation .............................................................................................................................................. 4 Latvia is a stable parliamentary democracy ranked as “free” by Freedom House. Its constitution guarantees basic civil liberties that the government recognizes in practice. The -

A Social Assessment of Poverty in Latvia
LISTENING TO THE POOR: A SOCIAL ASSESSMENT OF POVERTY IN LATVIA Report on research findings (March – June 1998) Institute of Philosophy and Sociology Riga, 1998 TABLE OF CONTENTS TALKING TO THE POOR:............................................................................................................ I A SOCIAL ASSESSMENT OF POVERTY IN LATVIA .............................................................. I TABLE OF CONTENTS................................................................................................................ II ACKNOWLEDGEMENTS.......................................................................................................... VI EXECUTIVE SUMMARY ......................................................................................................... VII OBJECTIVES OF THE STUDY ................................................................................................ VII METHODOLOGY ................................................................................................................. VII FINDINGS .......................................................................................................................... VIII CHAPTER 1: OBJECTIVES AND METHODS............................................................................1 AN ECONOMY IN TRANSITION................................................................................................1 OBJECTIVES OF THE STUDY ...................................................................................................2 METHODOLOGY