Innovations in Medical Education
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Count Me In; Resource Manual on Disabilities. INSTITUTION PACER Center, Inc., Minneapolis, KN
ED 341 218 EC 300 893 AUTHOR Milota, Cathy; And Others TITLE Count Me In; Resource Manual on Disabilities. INSTITUTION PACER Center, Inc., Minneapolis, KN. PUB DATE 91 NOTE 121p. AVAILABLE FROMPACER Center, 4826 Chicago Ave. S., Minneapolis, MN 55417-1055 ($15.00). PUB TYPE Guides - Non-Classrcom Use (055) EDRS PRICE ,MF01 Plus Postage. PC Not Available from EDRS. DESCRIPTORS Assisive Devices (for Disabled); Autism; *Disabilities; *Educational Legislation; Educational Resources; Elementary Secondary Education; EMotional Disturbances; *Federal Legislation; Hearing Impairments; *Intervention; Learning Disabilities; Mental Retardation; Multiple Disabilities; Physical Disabilities; Preschool Education; Simulation; Special Health Problems; Speech Handicaps; *Symptoms (Individual Disorders); Visual Impairments IDENTIFIERS Americans with Disabilities Act 1990; Education for All Handicapped Children Act; Education of the Handicapped Act Amendments 1986; Impairment Severity; Individuals with Disabilities Education Act; Rehabilitation Act 1973 (Section 504) ABSTRACT This resource guide presents general information about disabilities and summaries of relevant federal laws. A question-and-answer format is used to highlight key features of the Education for All Handicapped Children Act (Public Law 94-142, reauthorized in 1990 as the Individuals with Disabilities Education Act); Section 504 of the Rehabilitation Act of 1973; Public Law 99-457; and the Americans with Disabilities Act. Then individual sections provide information on vision impairments, hearing impairments, speech impairments, physical disabilities, mental retardation, learning disabilities, multiple disabilities, emotional disorders, autism, and other health impairments. Information provided typically includes the nature of the impairment, severity factors, associated problems, aids and appliances, therapeutic or remediation approaches, simulation activities, and resources (books for both children and adults as well as organizations). -

2010 Annual Report
University of Southern California 2010 A NEW DAY FOR USC FINANCIAL REPORT University of Southern California > University Park, UGB 205 Los Angeles, CA 90089-8006 10_USCFRcover_final.R2.indd 1 12/17/10 4:48:40 AM USC celebrates a new president and a long-awaited gathering place for students 1 A New Day for USC 3 A Great Place to Be 6 2010 Academic Year Highlights 12 Report of Independent Auditors 13 2010 Financial Summary 32 Budget 2010-2011 For information and additional 40 Board of Trustees copies of this report please contact: 41 Officers, Executives and Academic Deans University of Southern California 42 Role and Mission of the University University Park, UGB 205 Los Angeles, CA 90089-8006 email: [email protected] UNIVERSITY OF SOUTHERN CALIFORNIA FINANCIAL REPORT telephone: (213) 821-1900 > www.usc.edu 10_USCFRcover_final.R3.indd 2 12/17/10 4:48:03 PM A New Day for USC The summer of 2010 brought two historic changes to USC: the long- awaited opening of the Ronald Tutor Campus Center and the beginning of C. L. Max Nikias’s tenure as the eleventh president of the university. Nikias, who had been the university’s chief academic officer since 2005, presided over the grand opening of the Tutor Campus Center as one of his first ceremonial duties as president. He invoked the words of Winston Churchill, who said “We shape our buildings, and afterward our buildings shape us,” adding: “This building reflects our Trojan values. It gives voice to our greatest aspirations.” Throughout his career at USC, Nikias has paid particular attention to creating a dynamic, well-rounded intellectual environment for students. -

2019 Annual Report Our Conservation Supporters
2019 ANNUAL REPORT TO THE OUR CONSERVATION SUPPORTERS Partnerships with a Purpose Every piece of wetland or associated upland habitat A special thanks to our conserved by Ducks Unlimited Canada (DUC) is the result of partnerships. These partnerships are the government partners: foundation of DUC’s conservation leadership and the The governments listed below The State of Idaho reason why we so clearly envision a future for wetland have provided instrumental The State of Indiana conservation in North America. support in Canada over the The State of Kansas Today, this continent-wide network of conservation past year. staff, volunteers and supporters ensures that Ducks The Government of Canada The State of Kentucky Unlimited Canada, Ducks Unlimited, Inc., and The Government of Alberta The State of Louisiana Ducks Unlimited Mexico play leadership roles in The State of Maine international programs like the North American The Government of British Waterfowl Management Plan (NAWMP). Established Columbia The State of Maryland in 1986, NAWMP is a partnership of federal, provincial, The Government of Manitoba The State of Massachusetts state and municipal governments, nongovernmental The Government of The State of Michigan organizations, private companies and many individuals, New Brunswick all working towards achieving better wetland habitat The State of Minnesota for the benefit of waterfowl, other wetland associated The Government of The State of Mississippi wildlife and people. DUC is proud to be closely Newfoundland and Labrador The State of Missouri associated with NAWMP, one of the most successful The Government of the conservation initiatives in the world. Northwest Territories The State of Nebraska The State of Nevada The North American Wetlands Conservation Act The Government of (NAWCA), enacted by the U.S. -

First Prize ! (Story on Page 14) Page 2 INCO 'T'riangle JULY, 1960
VOLUME 20 COPPER CLIFF, ONTARIO, JULY, 1960 NUMBER 4 First Prize ! (story on Page 14) Page 2 INCO 'T'RIANGLE JULY, 1960 Frood Operations Make An Impressive View from the Air Published for all employees of The International Nickel Company of Canada, Limited. D. M. Dunbar, Editor Editorial Office Copper Cliff, Ont. Authorized as second class mail, Post Office Department , Ottawa, Inco, Nickel, and Numismatics By R. F. Boudignon Pay Office, Copper Cliff Numismatics is the science of coins, tokens, medals, paper money and objects closely related to these in form or purpose. I find it a most enjoyable hobby. To assist the numismatist in the study of coins, their origins and technique, their history, mythology and art, the international Nickel Company of Canada, Limited and its predecessors have published a number of most interesting and valuable books and pamphlets. Several weeks ago, through the library of the American Numis- matic Association I had the opportunity of reading a number of these, now out of print and most certainly collector's items in them- selves. In 1930 there appeared a very elaborate volume of some 125 In this fine aerial picture by the noted Canadian industrial photographer, George pages, entitled "Nickel Coins." It Hunter, are seen the Frood surface plant and open pit, part of the Frood-Stobie mine is a gem of the art of printing and publishing. Privately printed for operations. The first of the two long buildings at right centre is the hoistroom, and the International Nickel Company, in the second are the mine offices and changehouse. -

Letter from USC Radio
Map of Classical KUSC Coverage KUSC’s Classical Public Radio can be heard in 7 counties, from as far north as San Luis Obispo and as far south as the Mexican border. With 39,000 watts of power, Classical KUSC boasts the 10th most powerful signal in Southern California. KUSC transmits its programming from five transmitters - KUSC-91.5 fm in Los Angeles and Santa Clarita; 88.5 KPSC in Palm Springs; 91.1 KDSC in Thousand Oaks; 93.7 KDB in Santa Barbara and 99.7 in Morro Bay/San Luis Obispo. KUSC Mission To make classical music and the arts a more important part of more people’s lives. KUSC accomplishes this by presenting high quality classical music programming, and by producing and presenting programming that features the arts and culture of Southern California. KUSC supports the goal of the University of Southern California to position USC as a vibrant cultural enterprise in downtown Los Angeles. Page 1 Classical KUSC Table of Contents 1 Map of Classical KUSC Coverage / KUSC Mission 2 Classical KUSC Table of Contents 3-4 Letter from USC Radio President, Brenda Barnes 5 USC Radio Vice President / KUSC Programming Team 6 KUSC Programming On Air-Announcers 7-10 Programming Highlights 2013-14 11 KUSC Online and Tour with the Los Angeles Philharmonic 12 KUSC Interactive 13 KUSC Underwriting 14 KUSC Engineering 15 KUSC Administration 16 USC Radio Board of Councilors 17 Tours with KUSC 18 KUSC Development 19 Leadership Circle 20 Legacy Society 21 KUSC Supports the Arts 22 KUSC Revenue and Expenses Page 2 Letter From USC Radio hen I came to USC Radio almost 17 and covered the arts in the community for W years ago the Coachella Valley was decades. -

Morgan, Sylvia (2017) Constructing Identities, Reclaiming Subjectivities, Reconstructing Selves: an Interpretative Study of Transgender Practices in Scotland
Morgan, Sylvia (2017) Constructing identities, reclaiming subjectivities, reconstructing selves: an interpretative study of transgender practices in Scotland. PhD thesis. http://theses.gla.ac.uk/8073/ Copyright and moral rights for this work are retained by the author A copy can be downloaded for personal non-commercial research or study, without prior permission or charge This work cannot be reproduced or quoted extensively from without first obtaining permission in writing from the author The content must not be changed in any way or sold commercially in any format or medium without the formal permission of the author When referring to this work, full bibliographic details including the author, title, awarding institution and date of the thesis must be given Glasgow Theses Service http://theses.gla.ac.uk/ [email protected] Constructing identities, reclaiming subjectivities, reconstructing selves: an interpretative study of transgender practices in Scotland A thesis submitted in fulfilment of the requirements for the degree of Doctor of Philosophy By Sylvia Morgan (M.Litt, M.Ed) School of Social and Political Sciences, The College Social Sciences University of Glasgow, Scotland January 2017 Author’s Declaration I declare that the original work presented in this thesis is the work of the author Sylvia Morgan. I have been responsible for all aspects of the study unless where explicit reference is made to the contribution of others. This work has not been submitted for any other course or qualification on a previous occasion to University of Glasgow or any other institution. Sylvia Morgan Signed: ……………………………………………… Date:……………………………………………….. ABSTRACT This thesis provides a sociologically informed understanding of the intersubjective meanings of historical and emergent transgender identities and practices in Scotland. -

This Is Not a Book, As Books Are Always Written by the Scholars
1 Glimpses In Reality Rajinder Bibra 2 About the book This is the story of the little self, whom the author, especially chosen as the central character in his latest book in English, because he is an ideal ‘product’ of the modern Indian society, which is influenced by the western ‘values’ based on material culture. In his last two books the author has explained the progress and the process of the journey, in the realms of the wisdom; the l.s. has been enlightened to. The present book is an attempt on the part of the author, to pen down the penultimate fruits of the inward-journey of the little self, leading to ‘Self-realization’. In the process the l.s. went through the same time tested Sadhna (spiritual practice for the realization of the Self) methodology of concentration, contemplation and meditation. As a result of these churning, the author ‘produced’ three biographical books: “Quest in Reality”, “Prasanthi Thoughts”, and “Glimpses in Reality”. Therefore, the author is merely a medium through whom the l.s. expressed his inner pouring, and as such the real credit for the ‘creation’ of these books goes to him. These books are not the works of fiction or the borrowed excerpts from the scriptures, but only the ‘expressions’ of the little self’s ‘experiences,’ which the author has put them in book shape. During the course of his inner-journey, the l.s. realized, there was nothing supernatural or mythical about the existence of ‘Supreme-Reality/Intelligence’. It is a biological reality, which is easily provable and within the reach of all, whether they are theists or atheists. -

Telephone Directory
SCampus 2011-12 Exploring Los Angeles Telephone Directory Need to find the contact information for your department chair? In a hurry to locate the Student Affairs Office? The SCampus Telephone Directory is an easy way to find out who to contact and where to go for virtually anything on campus. A Unless otherwise noted, all phone Transcripts 740-7445 Undergraduate Success Program 740-0776 numbers are in the 213 area code. Asst. Registrar, James Feigert Dir., Abi Ingleton REG Lobby, MC 0912, 821-3758 (FAX) STU 301, MC 0896, 821-5479 (FAX) [email protected] [email protected]; [email protected] A www.usc.edu/transcripts www.usc.edu/cas Tuition Exchange 740-6963 Access Program Academic Counseling Services Tuition Exchange Liaison, USCard Office 740-8709 Academic Review Department 740-7741 Robert Morley PSD 102, PSX, HSC-SRH Lobby, Asst. Registrar, Kenny Eng JHH 104, MC 0912, 821-3759 (FAX) MC 1623, 740-7253 (FAX) TRO 101, MC 0912, 821-0249 (FAX) www.tuitionexchange.org [email protected] [email protected] Verification, Degree or www.usc.edu/uscard www.usc.edu/academicreview Enrollment 740-9230 Asst. Registrar, James Feigert Accounting, Leventhal School of Academic Culture Assembly REG Lobby, MC 0912, 821-3758 (FAX) Dean, William W. Holder 740-4838 Program Board 740-5656 [email protected] ACC 101A, MC 0441, 740-2153 (FAX) TCC 224, MC 3107, 740-2524 (FAX) www.usc.edu/verification [email protected] [email protected] marshall.usc.edu/lsoa www.academicculture.com Academic Recognition Programs Academic Affairs 740-4850 Trustee and Presidential Scholars; Academic Integrity Assoc. -
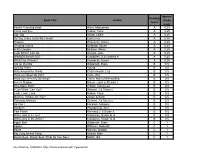
Book Title Author Reading Level Approx. Grade Level
Approx. Reading Book Title Author Grade Level Level Anno's Counting Book Anno, Mitsumasa A 0.25 Count and See Hoban, Tana A 0.25 Dig, Dig Wood, Leslie A 0.25 Do You Want To Be My Friend? Carle, Eric A 0.25 Flowers Hoenecke, Karen A 0.25 Growing Colors McMillan, Bruce A 0.25 In My Garden McLean, Moria A 0.25 Look What I Can Do Aruego, Jose A 0.25 What Do Insects Do? Canizares, S.& Chanko,P A 0.25 What Has Wheels? Hoenecke, Karen A 0.25 Cat on the Mat Wildsmith, Brain B 0.5 Getting There Young B 0.5 Hats Around the World Charlesworth, Liza B 0.5 Have you Seen My Cat? Carle, Eric B 0.5 Have you seen my Duckling? Tafuri, Nancy/Greenwillow B 0.5 Here's Skipper Salem, Llynn & Stewart,J B 0.5 How Many Fish? Cohen, Caron Lee B 0.5 I Can Write, Can You? Stewart, J & Salem,L B 0.5 Look, Look, Look Hoban, Tana B 0.5 Mommy, Where are You? Ziefert & Boon B 0.5 Runaway Monkey Stewart, J & Salem,L B 0.5 So Can I Facklam, Margery B 0.5 Sunburn Prokopchak, Ann B 0.5 Two Points Kennedy,J. & Eaton,A B 0.5 Who Lives in a Tree? Canizares, Susan et al B 0.5 Who Lives in the Arctic? Canizares, Susan et al B 0.5 Apple Bird Wildsmith, Brain C 1 Apples Williams, Deborah C 1 Bears Kalman, Bobbie C 1 Big Long Animal Song Artwell, Mike C 1 Brown Bear, Brown Bear What Do You See? Martin, Bill C 1 Found online, 7/20/2012, http://home.comcast.net/~ngiansante/ Approx. -

Sponsored Project Activity
SPONSORED PROJECT ACTIVITY - ACTIVE AWARDS AS OF 07/05/2011 Principal & Co-Inv TOT PROJ TOT PROJ Total Account Name(s) Department Name Title Sponsor Start End Amount -------------------- -------------------- ------------------------- ------------------------- -------- -------- ---------------- ADAMS, GREGOR B Broad-CIRM Center CIRM Bridges to Stem Cell California State 01/05/11 09/24/11 $4,000.00 Internship - CSU Channel University Channel Islands Islands ADER, MARILYN Physiology and Bioph Islet Transplant Program Islet Sheet Medical LLC 02/15/11 12/31/11 $89,329.00 ysics AKBARI, OMID Molecular Microbiolo Study the Role of 6b11mAb NKT Therapeutics, Inc. 07/01/09 12/31/11 $246,041.00 gy & Immunology in Preventing iNKT Cell Dependent Airway Hyperactivity in Va24-JaQ TCR Transgenic Mice AKBARI, OMID Molecular Microbiolo Role of NKT Cells in National Institute of 09/20/07 08/31/12 $1,217,390.20 gy & Immunology Airway Hyperreactivity Allergy and Infectious and Tolerance Diseases ALBER, FRANK UWE Computational Biolog Comprehensive Data Pew Charitable Trusts 07/01/09 06/30/14 $240,000.00 y Integration Towards A 3D Structure Of The Genome ALBER, FRANK UWE Computational Biolog Alfred P.Sloan Research Alfred P. Foundation 09/16/09 09/15/11 $50,000.00 y Fellowship for Dr. Frank Alber in Computational and Evolutionary Molecular Biology ALBER, FRANK UWE Biological Sciences New Tools for Exploring Rockefeller University 08/15/10 07/31/14 $0.00 The Dynamic Interactome CHEN, LIN ALBER, FRANK UWE Computational Biolog New Tools for Exploring Rockefeller University 08/15/10 07/31/14 $110,022.00 y The Dynamic Interactome CHEN, LIN ALBERTSON, DAVID C. -

The Foreign Service Journal, September 1956
SEPTEMBER, 1956 Throughout the world ^ more people buy Seagram’s VO. than any other imported whisky. Seagrams m CANADIAN WHISKY RARE OLD DELICATE CANADIAN WHISt SPECIALLY MATURED IN OAK CASKS DISTILLED. AGED AND BOTTLED UNDER THE SUPERVISION OF THE CANADIAN GOVERNMENT JOSEPH E. SEAGRAM £r- SONS. LIMITED WATERLOO • ONTARIO ■ CANADA PRODUCE OF CANADA Honoured the Wi wee **£'{*' * VV *H ,> For Business . For Pleasure rni* si Wnrlrl nf YOU CAN COUNT ON AMERICAN EXPRESS Here are the world-wide, world-wise services offered by American Express . 343 offices in 36 nations always ready to serve you completely, expertly, whatever your needs for business or pleasure. TRAVELERS CHEQUES MONEY ORDERS The best-known, most widely Pay bills and transmit funds accepted cheques in the world! with convenient, economical American Express Travelers American Express Money Cheques are 100% safe—immediate Orders... available through¬ refund if lost or stolen. You can out the U. S. at neighborhood buy them at BANKS, Railway stores, Railway Express and Express and Western Union offices. Western Union offices. TRAVEL SERVICES OTHER FINANCIAL SERVICES The trained and experienced staff of American Express Swift... convenient and dependable, will provide air or steamship other world-wide American Express tickets.. .hotel reservations... financial services include: foreign uniformed interpreters, and remittances, mail and cable transfer plan independent trips or of funds, and the purchase and escorted tours. sale of foreign currency. SHIPPING SERVICES f&RICAiV American Express offers complete facilities to handle personal and household effects shipments, also the entire operation of import or export forwarding, including customs clearances and marine insurance. Offices in Principal Cities of the World Now in our Second Century of Service Headquarters: 65 Broadway, New York 6, N. -

Nuhmafricanus 2
WORKS ISSUED BY tbe IFahlu* t !ocietp . 0 THE HISTORY AND DESCRIPTION OF AFRICA OF LEO AFRICANUS. VOL. II. No XCIII. THE HISTORY AND DESCRIPTION OF AFRICA AND OF THE NOTABLE THINGS THEREIN CONTAINED, WRITTEN BY AL-HASSAN IBN-MOHAMMED AL-WEZAZ AL-FASI, A MOOR, BAPTISED AS GIOVANNI LEONE, BUT BETTER KNOWN AS LEO AFRICANUS. DONE INTO ENGLISH IN THE YEAR 16oo, BY JOHN PORY, 2lnb nob) Ebiteb, bitb an *utroburtion anb $otro, BY DR. ROBERT BROWN. IN THREE VOLUMES.-VOL. II. LONDON: PRINTED FOR THE HAKLUYT SOCIETY, 4, LINCOLN'S INN FIELDS, W.C. LONDON: PRINTED AT THE BEDFORD PRESS, 20 AND 21, BEDFORDBURV, W.C. COUNCIL OF THE HAKLUYT SOCIETY. SIR CLEMENTS R. MARKHAM, K.C.B., F.R.S., Pres. R.G.S., PRESIDENT. THE RIGHT HON. THE LORD STANLEY OF ALDERLEY, VICE- PRESIDENT. SIR A. WOLLASTON FRANKS, K.C.B., F.R.S., VICE- PRESIDENT. C. RAYMOND BEAZLEY, ESQ., M.A. MILLER CHRISTY, ESQ. COLONEL G. EARL CHURCH. THE RIGHT HON. GEORGE N. CURZON, M.P. ALBERT GRAY, ESQ. THE RIGHT HON. LORD HAWKESBURY. EDWARD HEAWOOD, ESQ., M.A. ADMIRAL SIR ANTHONY H. HOSKINS, K.C.B. REAR-ADMIRAL ALBERT H. MARKHAM. A. P. MAUDSLAY, ESQ. E. DELMAR MORGAN, ESQ. CAPTAIN NATHAN, R.E. ADMIRAL SIR E. OMMANNEY, C.B., F.R.S. CUTHBERT E. PEEK, ESQ. E. G. RAVENSTEIN, ESQ. CouTrs TROTTER, ESQ. REAR-ADMIRAL W_ J. L. WHARTON, C.B., R.N. WILLIAM FOSTER, ESQ., Honorary Secretary. CONTENTS. VOLUME II. THE SECOND BOOK Notes to Book II THE THIRD BOOK Notes to Book III THE FOURTH BOOK Notes to Book IV PAGE 225 325 IOHN LEO HIS SECOND BOOKE OF the Historie of Africa, and of the memorable t/ings contained therein.