Description Ileostomy/Enterostomy an Ileostomy Is an Opening In
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Etditaxmurnats. ~THE JOURNAL of the BRITISH MEDICAL ASSOCIATION
THE ritishJ eTdiTaXMurnaTS. ~THE JOURNAL OF THE BRITISH MEDICAL ASSOCIATION. EDITED BY NORMAN GERALD HORNER, M.A., M.D. VOLUME 1, 1932 JANUARY TO JUNE I PRINTED AND PUBLISHED AT THE OFFICE OF THE BRITISH MEDICAL ASSOCIATION, TAVISTOCK SQUARE, LONDON, W.C.1. [Thu Bama-- J"A.-JUNE, I932j 1MXUDAL JOURNAL KEY TO DATES AND PAGES THE following table, giving a key to the dates of issue and the page numbers of the BRITISH MEDICAL JOURNAL and SUPPLEMENT in the first volume for 1932, may prove convenient to readers in search of a reference. Serial Date of Journal Supplement No. Issue. Pages. Pages. 3704 Jan. 2nd 1- 44 1- 8 3705 9th 45- 84 9- 12 3706 16th 85- 128 13- 20 3707 23rd 129- 176 21- 28 3708 30th 177- 222 29- 36 3709 Feb. 6th 223- 268 37- 48 3710 ,, 13th 269- 316 49- 60 3711 ,, 20th 317- 362 61- 68 3712 ,, 27th 363- 410 .69- 76 3713 March 5th 411- 456 ......77- 84 3714 12th 457- 506 ......85- 92 3715 19th 507- 550 93 - 104 3716 26th 551- 598 .105- 112 3717 April 2nd 599i.- 642 .113- 120 3718 9th 643- 692 .121 - 132 3719 ,, 16th 693- 738 .133- 144 3720 23rd 739- 784 .145- 160 3721 30th 785- 826 .161 - 208 3722 May 7th 827- 872 .209- 232 *3723 ,, 14th 873- 918 3724 21st 919- 968 .233 - 252 3725 , 28th 969- 1016 .253 - 264 3726 June 4th 1017 - 1062 .265 - 280 3727 11th 1063 - 1110 .281 - 288 3728 , 18th 1111 - 1156 .289- 312 3729 Pt 25th 1157 - 1200 .313- 348 * This No. -

An Interesting Case of Bishop-Koop Stoma Prolapse
Mirza, Bishop-koop stoma prolapse I M A G E S OPEN ACCESS An Interesting Case of Bishop-Koop Stoma Prolapse Bilal Mirza A 4-month-old male baby presented with enterostomy prolapse. Past medical history revealed two operations elsewhere during third week of life. The first operation was performed for pneumoperitoneum due to necrotizing enterocolitis (NEC) of distal jejunum. The involved portion of small intestine was resected and a primary end-to-end jejuno-ileal anastomosis performed. The patient had to be re-explored due to anastomotic disruption and then an end-to-side jejuno-ileal anastomosis with Bishop-Koop ileostomy fashioned [Image 1]. The patient remained well for three months and passed stool per rectally and occasionally from stoma. The patient on arrival was vitally stable with normal labs. The general physical and systemic examinations were unremarkable besides a prolapsed enterostomy. Patient was anesthetized. The prolapse was inverted Y shaped, Image 1: A line diagram illustrating end-to-side jejuno-ileal anastomosis with Bishop-Koop ileostomy. with the first limb the original Bishop Koop prolapse of ileal mucosa; whereas the second limb was the prolapsed The basic purpose of a Bishop-Koop enterostomy, in mucosa of jejunum through end-to-side jejuno-ileal patients of meconium ileus, is to provide a vent for and anastomosis. The mucosal anastomotic line was visible irrigation of the distal bowel having thick inspissated at the proximal part of that limb [Image 2]. Initially the meconium. In other pediatric surgical conditions, it is jejunal mucosa was returned back to the main stump being used as a safety guard for intestinal anastomosis followed by reduction of ileal mucosa. -

Culture Advantage Anatomy and Medical Terminology For
1 Culture Advantage Anatomy and Medical Terminology for Interpreters GASTROINTESTINAL SYSTEM Marlene V. Obermeyer, MA, RN [email protected] ©Culture Advantage http://www.cultureadvantage.org 2 Digestive System Case Study for PowerPoint Presentation Carlos is a 13-year old boy who is brought to the Emergency Department by his parents. Through an interpreter, the physician finds out that Carlos has started complaining of right lower quadrant pain about 16 hours ago. He was unable to eat supper, was nauseated and vomited several times. He is now feeling feverish and has pain all over his abdomen. An IV is started in his arm and he is given IV fluids and antibiotics. He is given medication for pain and given an antiemetic for nausea. He is also examined and interviewed by the physician. The physician obtains blood work that indicates Carlos has an acute infection. A CT scan of the abdomen indicates Carlos has appendicitis. A surgeon is contacted and Carlos is scheduled for emergency appendectomy. The interpreter is asked to translate the surgery consent form that states Carlos is going to have a "laparoscopic appendectomy, possible open laparotomy" and the parents are asked to sign the consent form. By the end of this section, you will learn the meaning of the following words: Acute IV (IV fluid, IV antibiotics) Antiemetic CT scan Appendicitis Appendectomy Laparoscopic appendectomy Open laparotomy ©Culture Advantage http://www.cultureadvantage.org 3 GASTROINTESTINAL SYSTEM TERMINOLOGY Terminology Meaning Terminology Meaning absorption The movement of Alimentary Alimen – nourishment. Refers food from the to the gastrointestinal or small intestine digestive tract into the cells of the body. -
Public Use Data File Documentation
Public Use Data File Documentation Part III - Medical Coding Manual and Short Index National Health Interview Survey, 1995 From the CENTERSFOR DISEASECONTROL AND PREVENTION/NationalCenter for Health Statistics U.S. DEPARTMENTOF HEALTHAND HUMAN SERVICES Centers for Disease Control and Prevention National Center for Health Statistics CDCCENTERS FOR DlSEASE CONTROL AND PREVENTlON Public Use Data File Documentation Part Ill - Medical Coding Manual and Short Index National Health Interview Survey, 1995 U.S. DEPARTMENT OF HEALTHAND HUMAN SERVICES Centers for Disease Control and Prevention National Center for Health Statistics Hyattsville, Maryland October 1997 TABLE OF CONTENTS Page SECTION I. INTRODUCTION AND ORIENTATION GUIDES A. Brief Description of the Health Interview Survey ............. .............. 1 B. Importance of the Medical Coding ...................... .............. 1 C. Codes Used (described briefly) ......................... .............. 2 D. Appendix III ...................................... .............. 2 E, The Short Index .................................... .............. 2 F. Abbreviations and References ......................... .............. 3 G. Training Preliminary to Coding ......................... .............. 4 SECTION II. CLASSES OF CHRONIC AND ACUTE CONDITIONS A. General Rules ................................................... 6 B. When to Assign “1” (Chronic) ........................................ 6 C. Selected Conditions Coded ” 1” Regardless of Onset ......................... 7 D. When to Assign -

Blade-Directed Totally Laparoscopic Feeding Jejunostomy – How to Do It
ISSN: 2574-1241 Volume 5- Issue 4: 2018 DOI: 10.26717/BJSTR.2018.07.001457 Chun Yi Tsai. Biomed J Sci & Tech Res Research Article Open Access Blade-Directed Totally Laparoscopic Feeding Jejunostomy – How to do it Chun Chih Lai, Chun Yi Tsai* and Chun Nan Yeh Department of General Surgery, Chang Gung Memorial Hospital, Taiwan Received: July 20, 2018; Published: July 23, 2018 *Corresponding author: Chun Yi Tsai, Assistant professor, Department of General Surgery, Chang Gung Memorial Hospital, Linkou branch, Taiwan,Chang Gung University, No.5, Fu Shing Street, Kweishan District, Taoyuan City, 333, Taiwan. Abstract Jejunostomy is the recommended route for enteral nutrition in certain patients. Various methods and equipment had been proposed to complete the operation laparoscopically. The method we proposed is based on the triangular rule of trocar orientation with typically available tube and equipment. It minimized the wounds to one 11mm trocar for the laparoscope plus two 5mm trocars for intracorporeal suturing, by creating the jejunostoma with straightforward surgical blade penetration. Sixty-nine patients underwent the operation as either a solitary procedure or a part of the operation based on preoperative indications. The majority of the patients received feeding within 3 day after operation (84%) without major new tubes. The method we proposed could be done with readily available equipment and minimized wounds and did not yield major complications. complications. Fifteen patients experienced tube dislodgement or occlusion during the follow up but did not encounter difficulty while exchanging Keywords: Laparoscopic Feeding Jejunostomy; Minimally Invasive Surgery; Enteral Nutrition Introduction of the patient, and the assistant stood at the right caudal side. -

Gastrointestinal Stomas and Fistulas: What Is Lost and What to Do? Rajesh K Pande1, Arpit Gupta2
INVITED REVIEW Gastrointestinal Stomas and Fistulas: What is Lost and What to Do? Rajesh K Pande1, Arpit Gupta2 ABSTRACT Abnormal connections between gastrointestinal tract (GIT) and skin are called enterocutaneous fistulas (ECFs). Presence of ECF is associated with significant morbidity and mortality. A stoma refers to a surgically created opening in the abdomen to divert feces or urine to the outside of the body, to compensate for partial or complete loss of bowel function. Gastrointestinal (GI) stomas and postoperative ECFs present a unique challenge to the intensivist due to development of malnutrition, dehydration, and sepsis leading to high morbidity and mortality. This review focuses on the basic concepts about the type of fistula and stomas, their indications and complications, and management. Principles of clinical management include replacement of fluid and electrolyte losses, control of sepsis along with reducing fistula output, prevention of malnutrition and psychological support, and skin care. Keywords: Enteral nutrition, Enterocutaneous fistula, Parenteral nutrition, Sepsis, Surgical stomas. Indian Journal of Critical Care Medicine (2020): 10.5005/jp-journals-10071-23620 INTRODUCTION 1,2Department of Critical Care, BLK Center for Critical Care, BLK Abnormal connections between gastrointestinal tract (GIT) and Superspeciality Hospital, New Delhi, India skin are called enterocutaneous fistulas (ECFs). Presence of ECF is Corresponding Author: Rajesh K Pande, Department of Critical Care, associated with significant morbidity and mortality. Seventy-five to BLK Center for Critical Care, BLK Superspeciality Hospital, New Delhi, eighty-five percent of ECFs are surgical in origin due to gut injury India, Phone: +91 9810536268, e-mail: [email protected] or significant manipulation and adhenolysis during surgery, or How to cite this article: Pande RK, Gupta A. -

Icd-9-Cm (2010)
ICD-9-CM (2010) PROCEDURE CODE LONG DESCRIPTION SHORT DESCRIPTION 0001 Therapeutic ultrasound of vessels of head and neck Ther ult head & neck ves 0002 Therapeutic ultrasound of heart Ther ultrasound of heart 0003 Therapeutic ultrasound of peripheral vascular vessels Ther ult peripheral ves 0009 Other therapeutic ultrasound Other therapeutic ultsnd 0010 Implantation of chemotherapeutic agent Implant chemothera agent 0011 Infusion of drotrecogin alfa (activated) Infus drotrecogin alfa 0012 Administration of inhaled nitric oxide Adm inhal nitric oxide 0013 Injection or infusion of nesiritide Inject/infus nesiritide 0014 Injection or infusion of oxazolidinone class of antibiotics Injection oxazolidinone 0015 High-dose infusion interleukin-2 [IL-2] High-dose infusion IL-2 0016 Pressurized treatment of venous bypass graft [conduit] with pharmaceutical substance Pressurized treat graft 0017 Infusion of vasopressor agent Infusion of vasopressor 0018 Infusion of immunosuppressive antibody therapy Infus immunosup antibody 0019 Disruption of blood brain barrier via infusion [BBBD] BBBD via infusion 0021 Intravascular imaging of extracranial cerebral vessels IVUS extracran cereb ves 0022 Intravascular imaging of intrathoracic vessels IVUS intrathoracic ves 0023 Intravascular imaging of peripheral vessels IVUS peripheral vessels 0024 Intravascular imaging of coronary vessels IVUS coronary vessels 0025 Intravascular imaging of renal vessels IVUS renal vessels 0028 Intravascular imaging, other specified vessel(s) Intravascul imaging NEC 0029 Intravascular -

What Is an Enteral Feeding Tube?
Your Feeding Tubes Feeding Your What Is an Enteral Feeding Tube? Enteral refers to within the digestive system or intestine. Enteral feeding tubes allow liquid food to enter your stomach or intestine through a tube. The soft, flexible tube enters a surgically created opening in the abdominal wall called an ostomy. An enterostomy tube in the stomach is called a gastrostomy. A tube in the small intestine is called a jejunostomy. The site on the abdomen where the tube is inserted is called a stoma. The location of the stoma depends on your specific operation and the shape of your abdomen. Most stomas: f Lie flat against your body f Are round in shape f Are red and moist (similar to the inside of your mouth) f Have no feeling Gastrostomy feeding tube Stoma tract Surgical Patient Education 112830_BODY.indd 1 8/21/15 9:25 AM 3 Who Needs an Enteral Feeding Tube? Cancer, trauma, nervous system and digestive system disorders, and congenital birth defects can cause difficulty in feeding. Some people also have difficulty swallowing, which increases the chance that they will breathe in food (aspirate). People who have difficulties feeding can benefit from a feeding tube. Your doctor will explain to you the specific reasons why you or your family member need a feeding tube. For some, a feeding tube is a new way of life, but for others, the tube is temporary and used until the problem can be treated or repaired. Low-profile feeding tube American College of Surgeons • Division of Education 112830_BODY.indd 2 8/21/15 9:25 AM 2 Your Feeding Tubes Feeding Your Understanding Your Digestive System When food enters your oral cavity (mouth), the lips and tongue move it toward the back of the throat. -

FY 2009 Final Addenda ICD-9-CM Volume 3, Procedures Effective October 1, 2008
FY 2009 Final Addenda ICD-9-CM Volume 3, Procedures Effective October 1, 2008 Tabular 00.3 Computer assisted surgery [CAS] Add inclusion term That without the use of robotic(s) technology Add exclusion term Excludes: robotic assisted procedures (17.41-17.49) New code 00.49 SuperSaturated oxygen therapy Aqueous oxygen (AO) therapy SSO2 SuperOxygenation infusion therapy Code also any: injection or infusion of thrombolytic agent (99.10) insertion of coronary artery stent(s) (36.06-36.07) intracoronary artery thrombolytic infusion (36.04) number of vascular stents inserted (00.45-00.48) number of vessels treated (00.40-00.43) open chest coronary artery angioplasty (36.03) other removal of coronary obstruction (36.09) percutaneous transluminal coronary angioplasty [PTCA] (00.66) procedure on vessel bifurcation (00.44) Excludes: other oxygen enrichment (93.96) other perfusion (39.97) New Code 00.58 Insertion of intra-aneurysm sac pressure monitoring device (intraoperative) Insertion of pressure sensor during endovascular repair of abdominal or thoracic aortic aneurysm(s) New code 00.59 Intravascular pressure measurement of coronary arteries Includes: fractional flow reserve (FFR) Code also any synchronous diagnostic or therapeutic procedures Excludes: intravascular pressure measurement of intrathoracic arteries (00.67) 00.66 Percutaneous transluminal coronary angioplasty [PTCA] or coronary atherectomy Add code also note Code also any: SuperSaturated oxygen therapy (00.49) 1 New code 00.67 Intravascular pressure measurement of intrathoracic -

Cecal Volvulus: a Review and Analysis of the Literature and Presentation Of
Cecal volvulus: A review and analysis of the Intestinal obstruction literature and presentation of three cases VIVIAN M. BARSKY, D.O. WARREN H. SWENSON, D.O., FACOS ANTHONY A. MINISSALE, n.o. Philadelphia, Pennsylvania contributes to the rotation of the cecum up- Three women were admitted to the hospital ward and to the left to form a closed loop. Ab- with signs and symptoms of cecal volvulus. normal mobility of the cecum has been re- They all were more than 40 years of age and ported in from 11 to 22 percent of several had adhesions from prior surgery. Two series of cadavers. Hendrick reported that in cases were the acute obstructive type of approximately 22 percent of the male and 28 volvulus in which the rotation involved the percent of the female cadavers studied, the cecum and ascending colon were sufficiently adhesions. In one case the length of the mobile to permit volvulus of 180 degrees. Ab- mesentery and its laxity caused intermittent normal fixation of the ascending colon by a bouts of cecal rotation. Detorsion of the transverse band (Jacksons membrane) or ad- involved bowel segment was done in each hesions from previous surgery may provide instance. The viability of the bowel was the fixed point about which the cecum may ro- assessed and when it was questionable, tate. Chronic distention of the cecum with gas right hemicolectomy was done with an or feces has been found to be a factor. At times, opening made between the ileum and the distal obstruction, such as that due to tumors, transverse colon. -

EFFERENT LOOP of JEJUNUM THROUGH a GASTRO-ENTEROSTOMY STOMA with a THEORY AS to the AETIOLOGY by MORTIMER BURDMAN, F.R.C.S
Postgrad Med J: first published as 10.1136/pgmj.30.342.200 on 1 April 1954. Downloaded from 2O0 REPORT OF A CASE OF THRICE OCCURRING RETROGRADE INTUSSUSCEPTION OF THE EFFERENT LOOP OF JEJUNUM THROUGH A GASTRO-ENTEROSTOMY STOMA WITH A THEORY AS TO THE AETIOLOGY By MORTIMER BURDMAN, F.R.C.S. Whittington Hospital In the past 35 years there have been over 40 modic, each attack being accompanied by retch- cases reported of retrograde intussusceptiqn of the ing. He was admitted to hospital five hours after efferent loop of the jejunum into the stomach the onset of acute symptoms. through a gastro-enterostomy stoma.. On examination the patient was seen to be a Although these cases have been recorded, there thin man with three vertical scars in the middle seems to be little in the way of explanation of the of his upper abdomen. There was divarication of mechanism of Some retrograde intussusception. the recti, due to atrophy of the musculatureby copyright. suggestions as to aetiology have been put forward resulting from his four previous operations. The by different authors, but these have not success- upper abdomen was tender and mildly guarded. fully stood up to the criticisms of the proposers The lower abdomen was soft, and not tender to themselves. palpation. No masses were palpable. Rectal An effort has been made to consider the prob- examination revealed no tenderness or other abnor- lem in the light of physiological principles in an mality. Temperature was normal, pulse rate 55 per attempt to understand the mechanism of retro- minute, of good quality. -
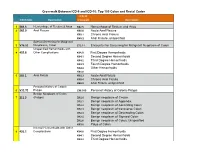
ICD-10 Coding
Crosswalk Between ICD-9 and ICD-10: Top 100 Colon and Rectal Codes ICD-10 ICD-9 Code Description Crosswalk Description 1 569.3 Hemorrhage of Rectum & Anus K62.5 Hemorrhage of Rectum and Anus 2 565.0 Anal Fissure K60.0 Acute Anal Fissure K60.1 Chronic Anal Fissure K60.2 Anal Fissure, unspecified Special Screening for Malignant 3 V76.51 Neoplasms, Colon Z12.11 Encounter for Screening for Malignant Neoplasm of Colon Unspecified Hemorrhoids with 4 455.8 Other Complications K64.0 First Degree Hemorrhoids K64.1 Second Degree Hemorrhoids K64.2 Third Degree Hemorrhoids K64.3 Fourth Degree Hemorrhoids K64.4 Other Hemorrhoids K64.8 5 565.1 Anal Fistula K60.3 Acute Anal Fistula K60.4 Chronic Anal Fistula K60.5 Anal Fistula, unspecified Personal History of Colonic 6 V12.72 Polyps Z86.010 Personal History of Colonic Polyps Benign Neoplasm of Colon 7 211.3 (Polyps) D12.0 Benign neoplasm of Cecum D12.1 Benign neoplasm of Appendix D12.2 Benign neoplasm of Ascending Colon D12.3 Benign neoplasm of transverse Colon D12.4 Benign neoplasm of Descending Colon D12.5 Benign neoplasm of Sigmoid Colon D12.6 Benign neoplasm of Colon, Unspecified K63.5 Polyp of Colon Internal Hemorrhoids with Other 8 455.2 Complications K64.0 First Degree Hemorrhoids K64.1 Second Degree Hemorrhoids K64.2 Third Degree Hemorrhoids Crosswalk Between ICD-9 and ICD-10: Top 100 Colon and Rectal Codes K64.3 Fourth Degree Hemorrhoids K64.8 Other Hemorrhoids 9 569.42 Anal or Rectal Pain K62.89 Other Specified Diseases of Anus and Rectum 10 698.0 Pruritus Ani L29.0 Pruritus Ani Internal Hemorrhoids