Raynaud's Phenomenon and Erythromelalgia
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Inline-Supplementary-Material-1.Pdf
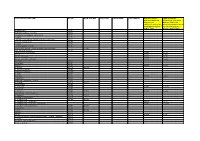
Appendix 1: STOPP/START criteria version 2 applied to the TRUST dataset Physiological system Criteria Criteria included Number (%) (The relevant () criteria for each participant were applied to the dataset and recorded in of Microsoft Office Excel ® (2013)) criteria included out of total criteria STOPP criteria Indication of medication A1. Any drug prescribed without an evidence-based clinical indication. X 1/3 (33.3) A2. Any drug prescribed beyond the recommended duration, where treatment duration is X well defined. A3. Any duplicate drug class prescription e.g. two concurrent NSAIDs, SSRIs, loop diuretics, ACE inhibitors, anticoagulants (optimisation of monotherapy within a single drug class should be observed prior to considering a new agent). Cardiovascular system B1. Digoxin for heart failure with preserved systolic ventricular function (no clear evidence X 7/13 (53.8) of benefit). B2. Verapamil or diltiazem with NYHA Class III or IV heart failure (may worsen heart failure). B3. Beta-blocker in combination with verapamil or diltiazem (risk of heart block). B4. Beta blocker with symptomatic bradycardia (< 50/min), type II heart block or complete heart block (risk of profound hypotension, asystole). B5. Amiodarone as first-line antiarrhythmic therapy in supraventricular tachyarrhythmias X (higher risk of side-effects than beta-blockers, digoxin, verapamil or diltiazem). B6. Loop diuretic as first-line treatment for hypertension (safer, more effective alternatives available). B7. Loop diuretic for dependent ankle oedema without clinical, biochemical evidence or radiological evidence of heart failure, liver failure, nephrotic syndrome or renal failure (leg elevation and /or compression hosiery usually more appropriate). B8. Thiazide diuretic with current significant hypokalaemia (i.e. -

Raynaud's Phenomenon and the Possible Use of Foods
JFS R: Concise Reviews/Hypotheses in Food Science Raynaud’s Phenomenon and the Possible Use of Foods CHRIS I. WRIGHT, CHRISTINE I. KRONER, AND RICHARD DRAIJER R: Concise Reviews in Food Science ABSTRACT: In this article we focus on the possible use of foods to alleviate Raynaud’s phenomenon (RP). RP is evoked, predominately, by cold and results in a potent vascular constriction of the microvascular blood vessels in the hands, thus leading to reduced hand blood flow and the elevation of pain sensation. To alleviate RP by diet, food components need to be able to promote hand skin blood flow, which may be achieved using fish oil, garlic, ginkgo biloba, L-carnitine, or inositol nicotinate, or to increase hand skin temperature, using evening primrose oil, ginkgo biloba, or inositol nicotinate. Although there are a number of studies documenting such improvements with these ingredients, they often are poorly designed. Hence, there is a need for more controlled studies to substantiate their use, but also to test alternative foods or target new ones. Therefore, we also discuss some alternate food options and briefly outline clinical drugs for the treatment of RP, as their mechanisms of action may also be possible targets for food. It is the intention of this article to address the research needs of this field and to provide a better understanding of alternative options for those with RP. Keywords: Raynaud’s, vascular constriction, dietary intervention, nutraceutical, functional foods Introduction Mahoney 1999; Generini and others 2003; Herrick 2003); however, lit- here are a growing number of studies focusing on the con- tle work has been published on the use of foods as a complementary Tceivable health benefits of foods, botanicals, and supplements treatment for RP patients or as a safeguard for those at high or future (Boelsma and others 2001; Green and others 2003). -

Poisons and Narcotic Drugs (Amendment) Ordinance 1988
AUSTRALIAN CAPITAL TERRITORY Poisons and Narcotic Drugs (Amendment) Ordinance 1988 No. 96 of 1988 I, THE GOVERNOR-GENERAL of the Commonwealth of Australia, acting with the advice of the Federal Executive Council, hereby make the following Ordinance under the Seat of Government (Administration) Act 1910. Dated 15 December 1988 N. M. STEPHEN Governor-General By His Excellency’s Command, CLYDE HOLDING Minister of State for the Arts and Territories An Ordinance to amend the Poisons and Narcotic Drugs Ordinance 1978 Short title 1. This Ordinance may be cited as the Poisons and Narcotic Drugs (Amendment) Ordinance 1988.1 Commencement 2. This Ordinance commences on such date as is fixed by the Minister by notice in the Gazette. Principal Ordinance 3. In this Ordinance, “Principal Ordinance” means the Poisons and Narcotic Drugs Ordinance 1978.2 (Ord. 79/88)—Cat. No. Authorised by the ACT Parliamentary Counsel—also accessible at www.legislation.act.gov.au 2 Poisons and Narcotic Drugs (Amendment) No. 96, 1988 Substances to which Division applies 4. Section 27B of the Principal Ordinance is amended by adding at the end the following paragraphs: “; (f) follicle stimulating hormone; (g) luteinising hormone; (h) thalidomide.”. Grant of authorisation 5. Section 27E of the Principal Ordinance is amended— (a) by omitting from paragraph (1) (a) “or cyclofenil” and substituting “, cyclofenil, follicle stimulating hormone or luteinising hormone”; (b) by omitting from paragraph (1) (b) “and”; and (c) by adding at the end of subsection (1) the following word and paragraph: “; and (d) in the case of an application that relates to thalidomide— the applicant is a specialist physician with no less than 5 years’ experience in the treatment of erythema nodosum leprosum.”. -
List of Union Reference Dates A
Active substance name (INN) EU DLP BfArM / BAH DLP yearly PSUR 6-month-PSUR yearly PSUR bis DLP (List of Union PSUR Submission Reference Dates and Frequency (List of Union Frequency of Reference Dates and submission of Periodic Frequency of submission of Safety Update Reports, Periodic Safety Update 30 Nov. 2012) Reports, 30 Nov. -

)&F1y3x PHARMACEUTICAL APPENDIX to THE
)&f1y3X PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE )&f1y3X PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 3 Table 1. This table enumerates products described by International Non-proprietary Names (INN) which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service (CAS) registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. Product CAS No. Product CAS No. ABAMECTIN 65195-55-3 ACTODIGIN 36983-69-4 ABANOQUIL 90402-40-7 ADAFENOXATE 82168-26-1 ABCIXIMAB 143653-53-6 ADAMEXINE 54785-02-3 ABECARNIL 111841-85-1 ADAPALENE 106685-40-9 ABITESARTAN 137882-98-5 ADAPROLOL 101479-70-3 ABLUKAST 96566-25-5 ADATANSERIN 127266-56-2 ABUNIDAZOLE 91017-58-2 ADEFOVIR 106941-25-7 ACADESINE 2627-69-2 ADELMIDROL 1675-66-7 ACAMPROSATE 77337-76-9 ADEMETIONINE 17176-17-9 ACAPRAZINE 55485-20-6 ADENOSINE PHOSPHATE 61-19-8 ACARBOSE 56180-94-0 ADIBENDAN 100510-33-6 ACEBROCHOL 514-50-1 ADICILLIN 525-94-0 ACEBURIC ACID 26976-72-7 ADIMOLOL 78459-19-5 ACEBUTOLOL 37517-30-9 ADINAZOLAM 37115-32-5 ACECAINIDE 32795-44-1 ADIPHENINE 64-95-9 ACECARBROMAL 77-66-7 ADIPIODONE 606-17-7 ACECLIDINE 827-61-2 ADITEREN 56066-19-4 ACECLOFENAC 89796-99-6 ADITOPRIM 56066-63-8 ACEDAPSONE 77-46-3 ADOSOPINE 88124-26-9 ACEDIASULFONE SODIUM 127-60-6 ADOZELESIN 110314-48-2 ACEDOBEN 556-08-1 ADRAFINIL 63547-13-7 ACEFLURANOL 80595-73-9 ADRENALONE -

Pharmacy and Poisons (Third and Fourth Schedule Amendment) Order 2017
Q UO N T FA R U T A F E BERMUDA PHARMACY AND POISONS (THIRD AND FOURTH SCHEDULE AMENDMENT) ORDER 2017 BR 111 / 2017 The Minister responsible for health, in exercise of the power conferred by section 48A(1) of the Pharmacy and Poisons Act 1979, makes the following Order: Citation 1 This Order may be cited as the Pharmacy and Poisons (Third and Fourth Schedule Amendment) Order 2017. Repeals and replaces the Third and Fourth Schedule of the Pharmacy and Poisons Act 1979 2 The Third and Fourth Schedules to the Pharmacy and Poisons Act 1979 are repealed and replaced with— “THIRD SCHEDULE (Sections 25(6); 27(1))) DRUGS OBTAINABLE ONLY ON PRESCRIPTION EXCEPT WHERE SPECIFIED IN THE FOURTH SCHEDULE (PART I AND PART II) Note: The following annotations used in this Schedule have the following meanings: md (maximum dose) i.e. the maximum quantity of the substance contained in the amount of a medicinal product which is recommended to be taken or administered at any one time. 1 PHARMACY AND POISONS (THIRD AND FOURTH SCHEDULE AMENDMENT) ORDER 2017 mdd (maximum daily dose) i.e. the maximum quantity of the substance that is contained in the amount of a medicinal product which is recommended to be taken or administered in any period of 24 hours. mg milligram ms (maximum strength) i.e. either or, if so specified, both of the following: (a) the maximum quantity of the substance by weight or volume that is contained in the dosage unit of a medicinal product; or (b) the maximum percentage of the substance contained in a medicinal product calculated in terms of w/w, w/v, v/w, or v/v, as appropriate. -

Medicines Regulations 1984 (SR 1984/143)
Reprint as at 1 April 2020 Medicines Regulations 1984 (SR 1984/143) David Beattie, Governor-General Order in Council At the Government House at Wellington this 5th day of June 1984 Present: His Excellency the Governor-General in Council Pursuant to section 105 of the Medicines Act 1981, and, in the case of Part 3 of the regulations, to section 62 of that Act, His Excellency the Governor-General, acting on the advice of the Minister of Health tendered after consultation with the organisations and bodies that appeared to the Minister to be representatives of persons likely to be substantially affected, and by and with the advice and consent of the Executive Coun- cil, hereby makes the following regulations. Contents Page 1 Title and commencement 5 2 Interpretation 5 Part 1 Classification of medicines 3 Classification of medicines 9 Note Changes authorised by subpart 2 of Part 2 of the Legislation Act 2012 have been made in this official reprint. Note 4 at the end of this reprint provides a list of the amendments incorporated. These regulations are administered by the Ministry of Health. 1 Reprinted as at Medicines Regulations 1984 1 April 2020 Part 2 Standards 4 Standards for medicines, related products, medical devices, 10 cosmetics, and surgical dressings 4A Standard for CBD products 10 5 Pharmacist may dilute medicine in particular case 11 6 Colouring substances [Revoked] 11 Part 3 Advertisements 7 Advertisements not to claim official approval 11 8 Advertisements for medicines 11 9 Advertisements for related products 13 10 Advertisements -

Arterial Manifestations in Young People
Arterial Manifestations in Young People Ann Marie Kupinski, PhD RVT RDMS FSVU North Country Vascular Diagnostics, Inc, & Albany Medical College, Albany, NY Objectives Describe arterial pathology encountered in young people Discuss criteria used to diagnose nonatherosclerotic disease entities Present cases which illustrate ultrasound findings of arterial disease in young people Arterial Disease in Young People • Approx. 90% of PAD and extracranial arterial disease is due to atherosclerosis • Nonatherosclerotic diseases can include: • Inflammatory diseases • Non-inflammatory diseases (FMD) • Congenital abnormalities • Acquired diseases • Injuries Testing Options • Ultrasound – Useful with large vessel disease – Giant Cell, Takayasu’s, Radiation arteritis – Injury/Trauma • Physiologic testing (PVR, PPG, pressures) – Useful with small vessel disease Buerger’s Disease (Thromboangiitis obliterans) Vasospastic Disease Fibromuscular dysplasia FMD Noninflammatory Nonatherosclerotic Young individuals (mean onset 48 yrs) Women (3:1) Affects small to medium- sized arteries Intima, media or adventitia FMD Distribution Renal 60-75% Cerebrovascular 25-30% Visceral 9% Extremity Arteries 5% Has also been observed in coronary arteries, pulmonary arteries and the aorta 28% of patients have at least two vascular beds involved Intimal fibroplasia Smooth focal stenosis with a concentric band Long smooth tubular stenosis Poloskey, et al. Circulation 2012;125 Medial fibroplasia Alternating areas of thinned media and thickened fibromuscular -

Marrakesh Agreement Establishing the World Trade Organization
No. 31874 Multilateral Marrakesh Agreement establishing the World Trade Organ ization (with final act, annexes and protocol). Concluded at Marrakesh on 15 April 1994 Authentic texts: English, French and Spanish. Registered by the Director-General of the World Trade Organization, acting on behalf of the Parties, on 1 June 1995. Multilat ral Accord de Marrakech instituant l©Organisation mondiale du commerce (avec acte final, annexes et protocole). Conclu Marrakech le 15 avril 1994 Textes authentiques : anglais, français et espagnol. Enregistré par le Directeur général de l'Organisation mondiale du com merce, agissant au nom des Parties, le 1er juin 1995. Vol. 1867, 1-31874 4_________United Nations — Treaty Series • Nations Unies — Recueil des Traités 1995 Table of contents Table des matières Indice [Volume 1867] FINAL ACT EMBODYING THE RESULTS OF THE URUGUAY ROUND OF MULTILATERAL TRADE NEGOTIATIONS ACTE FINAL REPRENANT LES RESULTATS DES NEGOCIATIONS COMMERCIALES MULTILATERALES DU CYCLE D©URUGUAY ACTA FINAL EN QUE SE INCORPOR N LOS RESULTADOS DE LA RONDA URUGUAY DE NEGOCIACIONES COMERCIALES MULTILATERALES SIGNATURES - SIGNATURES - FIRMAS MINISTERIAL DECISIONS, DECLARATIONS AND UNDERSTANDING DECISIONS, DECLARATIONS ET MEMORANDUM D©ACCORD MINISTERIELS DECISIONES, DECLARACIONES Y ENTEND MIENTO MINISTERIALES MARRAKESH AGREEMENT ESTABLISHING THE WORLD TRADE ORGANIZATION ACCORD DE MARRAKECH INSTITUANT L©ORGANISATION MONDIALE DU COMMERCE ACUERDO DE MARRAKECH POR EL QUE SE ESTABLECE LA ORGANIZACI N MUND1AL DEL COMERCIO ANNEX 1 ANNEXE 1 ANEXO 1 ANNEX -

Australian Statistics on Medicines 1997 Commonwealth Department of Health and Family Services
Australian Statistics on Medicines 1997 Commonwealth Department of Health and Family Services Australian Statistics on Medicines 1997 i © Commonwealth of Australia 1998 ISBN 0 642 36772 8 This work is copyright. Apart from any use as permitted under the Copyright Act 1968, no part may be repoduced by any process without written permission from AusInfo. Requests and enquiries concerning reproduction and rights should be directed to the Manager, Legislative Services, AusInfo, GPO Box 1920, Canberra, ACT 2601. Publication approval number 2446 ii FOREWORD The Australian Statistics on Medicines (ASM) is an annual publication produced by the Drug Utilisation Sub-Committee (DUSC) of the Pharmaceutical Benefits Advisory Committee. Comprehensive drug utilisation data are required for a number of purposes including pharmacosurveillance and the targeting and evaluation of quality use of medicines initiatives. It is also needed by regulatory and financing authorities and by the Pharmaceutical Industry. A major aim of the ASM has been to put comprehensive and valid statistics on the Australian use of medicines in the public domain to allow access by all interested parties. Publication of the Australian data facilitates international comparisons of drug utilisation profiles, and encourages international collaboration on drug utilisation research particularly in relation to enhancing the quality use of medicines and health outcomes. The data available in the ASM represent estimates of the aggregate community use (non public hospital) of prescription medicines in Australia. In 1997 the estimated number of prescriptions dispensed through community pharmacies was 179 million prescriptions, a level of increase over 1996 of only 0.4% which was less than the increase in population (1.2%). -
Layne14cv14.Pdf
IN THE UNITED STATES DISTRICT COURT FOR THE WESTERN DISTRICT OF VIRGINIA Harrisonburg Division CARLA R. LAYNE, ) Plaintiff, ) ) Civil Action No. 5:14cv00014 v. ) ) By: Joel C. Hoppe CAROLYN W. COLVIN, ) United States Magistrate Judge Acting Commissioner, ) Social Security Administration, ) Defendant. ) REPORT AND RECOMMENDATION Plaintiff Carla R. Layne asks this Court to review the Commissioner of Social Security’s (“Commissioner”) final decision denying her applications for disability insurance benefits (“DIB”) and supplemental security income (“SSI”) under Titles II and XVI of the Social Security Act, 42 U.S.C. §§ 401–422, 1381–1383f. This Court has authority to decide Layne’s case under 42 U.S.C. §§ 405(g) and 1383(c)(3), and her case is before me by referral under 28 U.S.C. § 636(b)(1)(B). Having considered the administrative record, the parties’ briefs and oral arguments, and the applicable law, I find that substantial evidence supports the Commissioner’s final decision that Layne is not disabled. I. Standard of Review The Social Security Act authorizes this Court to review the Commissioner’s final decision that a person is not entitled to disability benefits. See 42 U.S.C. § 405(g); Hines v. Barnhart, 453 F.3d 559, 561 (4th Cir. 2006). The Court’s role, however, is limited—it may not “reweigh conflicting evidence, make credibility determinations, or substitute [its] judgment” for that of agency officials. Hancock v. Astrue, 667 F.3d 470, 472 (4th Cir. 2012). Instead, the Court asks only whether the Administrative Law Judge (“ALJ”) applied the correct legal standards and 1 whether substantial evidence supports the ALJ’s factual findings. -

ESVM Guidelines – the Diagnosis and Management of Raynaud's Phenomenon
413 Review ESVM guidelines – the diagnosis and management of Raynaud’s phenomenon Writing group Jill Belch1, Anita Carlizza2, Patrick H. Carpentier3, Joel Constans4, Faisel Khan1, and Jean-Claude Wautrecht5 1 University of Dundee School of Medicine, Dundee, United Kingdom 2 Azienda Ospedaliera S.Giovanni-Addolorata, Rome, Italy 3 Grenoble University Hospital, Grenoble, France 4 Hopital St Andre, Bordeaux, France 5 Cliniques universitaires de Bruxelles, Brussels, Belgium ESVM board authors Adriana Visona6, Christian Heiss7, Marianne Brodeman8, Zsolt Pécsvárady9, Karel Roztocil10, Mary-Paula Colgan11, Dragan Vasic12, Anders Gottsäter13, Beatrice Amann-Vesti14, Ali Chraim15, Pavel Poredoš16, Dan-Mircea Olinic17, Juraj Madaric18, and Sigrid Nikol19 6 Angiology Unit, Azienda ULSS 2, Marca Trevigiana, Treviso, Italy 7 Department of Cardiology, Pulmonology and Vascular Medicine, Düsseldorf, Germany 8 Division of Angiology, Medical University, Graz, Austria 9 Head of 2nd Dept. of Internal Medicine, Vascular Center, Flor Ferenc Teaching Hospital, Kistarcsa, Hungary 10 Institute of Clinical and Experimental Medicine, Prague, Czech Republic 11 St. James’s Hospital and Trinity College, Dublin, Ireland 12 Clinical Centre of Serbia, Belgrade, Serbia 13 Department of Vascular Diseases, Skåne University Hospital, Sweden 14 Clinic for Angiology, University Hospital Zurich, Switzerland 15 Department of Vascular Surgery, Cedrus Vein and Vascular Clinic, Lviv Hospital, Lviv, Ukraine 16 University Medical Centre Ljubljana, Slovenia 17 Medical Clinic no. 1,