Acquired Bilateral Vocal Cord Paralysis, 166 Acquired Subglottic Stenosis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Lung Pathology: Embryologic Abnormalities
Chapter2C Lung Pathology: Embryologic Abnormalities Content and Objectives Pulmonary Sequestration 2C-3 Chest X-ray Findings in Arteriovenous Malformation of the Great Vein of Galen 2C-7 Situs Inversus Totalis 2C-10 Congenital Cystic Adenomatoid Malformation of the Lung 2C-14 VATER Association 2C-20 Extralobar Sequestration with Congenital Diaphragmatic Hernia: A Complicated Case Study 2C-24 Congenital Chylothorax: A Case Study 2C-37 Continuing Nursing Education Test CNE-1 Objectives: 1. Explain how the diagnosis of pulmonary sequestration is made. 2. Discuss the types of imaging studies used to diagnose AVM of the great vein of Galen. 3. Describe how imaging studies are used to treat AVM. 4. Explain how situs inversus totalis is diagnosed. 5. Discuss the differential diagnosis of congenital cystic adenomatoid malformation. (continued) Neonatal Radiology Basics Lung Pathology: Embryologic Abnormalities 2C-1 6. Describe the diagnosis work-up for VATER association. 7. Explain the three classifications of pulmonary sequestration. 8. Discuss the diagnostic procedures for congenital chylothorax. 2C-2 Lung Pathology: Embryologic Abnormalities Neonatal Radiology Basics Chapter2C Lung Pathology: Embryologic Abnormalities EDITOR Carol Trotter, PhD, RN, NNP-BC Pulmonary Sequestration pulmonary sequestrations is cited as the 1902 theory of Eppinger and Schauenstein.4 The two postulated an accessory he clinician frequently cares for infants who present foregut tracheobronchia budding distal to the normal buds, Twith respiratory distress and/or abnormal chest x-ray with caudal migration giving rise to the sequestered tissue. The findings of undetermined etiology. One of the essential com- type of sequestration, intralobar or extralobar, would depend ponents in the process of patient evaluation is consideration on the timing of the accessory foregut budding (Figure 2C-1). -

Vocal Cord Dysfunction: a Review Neha M
Dunn et al. Asthma Research and Practice (2015) 1:9 DOI 10.1186/s40733-015-0009-z REVIEW Open Access Vocal cord dysfunction: a review Neha M. Dunn1*, Rohit K. Katial2 and Flavia C. L. Hoyte2 Abstract Vocal cord dysfunction (VCD) is a term that refers to inappropriate adduction of the vocal cords during inhalation and sometimes exhalation. It is a functional disorder that serves as an important mimicker of asthma. Vocal cord dysfunction can be difficult to treat as the condition is often underappreciated and misdiagnosed in clinical practice. Recognition of vocal cord dysfunction in patients with asthma-type symptoms is essential since missing this diagnosis can be a barrier to adequately treating patients with uncontrolled respiratory symptoms. Although symptoms often mimic asthma, the two conditions have certain distinct clinical features and demonstrate specific findings on diagnostic studies, which can serve to differentiate the two conditions. Moreover, management of vocal cord dysfunction should be directed at minimizing known triggers and initiating speech therapy, thereby minimizing use of unnecessary asthma medications. This review article describes key clinical features, important physical exam findings and commonly reported triggers in patients with vocal cord dysfunction. Additionally, this article discusses useful diagnostic studies to identify patients with vocal cord dysfunction and current management options for such patients. Keywords: Vocal cord dysfunction, Paradoxical vocal fold movement, Vocal cord, Asthma-comorbidity Introduction medical literature 70 years later, in 1974, by Patterson Vocal cord dysfunction (VCD) is a term that refers to in- and colleagues in a 33 year old woman with 15 hospitali- appropriate adduction of the vocal cords during inhalation zations for what they termed “Munchausen’s stridor” [6]. -

Posterior Glottic Stenosis in Adults
Original Articles Posterior Glottic Stenosis in Adults Michael Wolf MD, Adi Primov-Fever MD, Yoav P. Talmi MD FACS and Jona Kronenberg MD Department of Otorhinolaryngology & Head Neck Surgery, Sheba Medical Center, Tel Hashomer, Israel Affiliated to Sackler Faculty of Medicine, Tel Aviv University, Ramat Aviv, Israel Key words: larynx, vocal cords, stenosis, fixation, laryngoplasty Abstract entiation between vocal cord paralysis and fixation [3,4], although Background: Posterior glottic stenosis is a complication of some patients survived complex central nervous system and prolonged intubation, manifesting as airway stenosis that may mimic peripheral organ injuries, long courses of mechanical ventilation, bilateral vocal cord paralysis. It presents a variety of features that oral or nasal intubation, and nasogastric tubing. These may result mandate specific surgical interventions. in combined pathologies of both paralysis and fixation, or they Objectives: To summarize our experience with PSG and its working diagnosis. may mask the alleged simplicity of making a diagnosis based Methods: We conducted a retrospective review of a cohort of solely on clinical grounds. The extent of scarring dictates the adult patients with PGS operated at the Sheba Medical Center extent of surgical intervention. While endoscopic lysis of the scar between 1994 and 2006. is appropriate for grade 1, complex laryngoplasty procedures are Results: Ten patients were diagnosed with PGS, 6 of whom mandated for grades 2 to 4 [3]. also had stenosis at other sites of -

Extralobar Pulmonary Sequestration Infected with Mycobacterium Gordonae
Brief Communications Extralobar pulmonary sequestration infected with Mycobacterium gordonae Yukio Umeda, MD, PhD,a Yukihiro Matsuno, MD, PhD,a Matsuhisa Imaizumi, MD, PhD,a Yoshio Mori, MD, PhD,a Hitoshi Iwata, MD, PhD,b and Hiroshi Takiya, MD, PhD,a Gifu, Japan Pulmonary sequestration is a malformation composed of lung was found except around the left lower pulmonary dysplastic lung tissue without normal communication with vein. We diagnosed it as extralobar sequestration and the tracheobronchial tree and with an anomalous systemic planned a simple excision of the sequestrated lung. We di- arterial supply.1 Few cases of pulmonary sequestration in- vided the aberrant artery and drainage vein and excised the fected with tuberculous or nontuberculous mycobacterium sequestrated lung using a linear stapler. The postoperative have been reported.2-4 However, all of those reports were course was uneventful. of intralobar pulmonary sequestrations. In the present article, Histopathologic study revealed destruction of alveolar we describe the first case of extralobar sequestration infected and reconstruction of respiratory epithelium within its own with Mycobacterium gordonae. pleura. The alveolar spaces were filled by mucoid or mono- nuclear cells. Caseating epithelioid granulomas and Lan- ghans’ giant cells were also observed (Figure 2). The CLINICAL SUMMARY diagnosis was of an extralobar pulmonary sequestration in- In August of 2005, a 72-year-old woman was referred to fected with Mycobacterium. M. gordonae was identified the Gifu Prefectural General Medical Center for abnormal from the culture of preoperatively collected sputum and sur- shadow on chest x-ray. Contrast media-enhanced com- gical specimen by the DNA–DNA hybridization method. -

Recurrent Pneumonia (Recurrent Lower Respiratory Tract Infections)
Recurrent Pneumonia (Recurrent lower respiratory tract infections) Guideline developed by Gulnur Com, MD, and Jeanne Velasco, MD in collaboration with the ANGELS team. Last reviewed by Jeanne Velasco, MD, on May 15, 2017. Key Points A single episode of uncomplicated pneumonia in an otherwise healthy child does not require investigation. Recurrent pneumonia is not an uncommon presenting symptom in general pediatric practice and one of the most common reasons for referral to pediatric pulmonologists. Recurrent pneumonia is usually defined as ≥2 episodes of pneumonia in a year or ≥3 in life.1 Many children with recurrent pneumonia do not need a full diagnostic work up, either because pneumonia episodes are not frequent or severe enough or because eventually children become asymptomatic. Evaluation of children with recurrent pneumonias begins by taking a careful history, an examination while the child is sick, and confirmation that the child is truly experiencing recurrent pneumonia. The majority of recurrent pneumonia causes in children have predictable risk factors (e.g., psychomotor retardation with feeding problems). Extensive investigations may not identify an underlying cause in up to 30% of children with recurrent pneumonia.1 The initial step in evaluating a child with recurrent respiratory symptoms includes distinguishing between recurrent wheezing versus recurrent infections. Studies show that asthma is being over diagnosed in children with recurrent respiratory symptoms. Patients with atypical asthma that does not respond to therapy should be investigated further. The evaluation of children with recurrent pneumonia should not be focused only on the respiratory tract. 1 Investigation for other organ system involvement may help for ultimate diagnosis (e.g., cystic fibrosis). -

The Importance of Inspiratory Maneuver for Benign Laryngeal Lesions
THIEME Original Research 513 The Importance of Inspiratory Maneuver for Benign Laryngeal Lesions Marília Batista Costa1 Taynara Oliveira Ledo1 Mariana Delgado Fernandes1 Romualdo Suzano Louzeiro Tiago1 1 Otorhinolaryngology Department, Hospital do Servidor Publico Address for correspondence Marília Batista Costa, MD, Estadual de Sao Paulo, Sao Paulo, SP, Brazil Otorrinolaringologia, Hospital do Servidor Publico Estadual de São Paulo, Rua Pedro de Toledo, 1800, Vila Clementino, São Paulo, SP, Int Arch Otorhinolaryngol 2020;24(4):e513–e517. 04029-000, Brazil (e-mail: [email protected]). Abstract Introduction Inspiratory maneuver corresponds to a simple method used during videolaryngoscopy to increase characterizations of laryngeal findings, through the movement of the vocal fold cover and exposure of the ligament, facilitating its evaluation. Objective To evaluate the increase in diagnosis of benign laryngeal lesions from the usage of inspiratory maneuvers during videolaryngoscopy in patients with or without vocal complaints. Methods A cross-sectional study performed from March 1 to July 1, 2018, in the Laryngology sector of a tertiary hospital. The age of the patients varied from 18 to 60 years old. They were divided into two groups, symptomatic and asymptomatic vocals, and evaluated through videolaryngoscopy together with inspiratory maneu- vers. The exams were recorded and later evaluated by three trained laryngologists who determined the laryngeal lesions before and after the inspiratory maneuver. Results Therewere60patientsinthissample,41ofwhichwerevocalsymptomatic and 19 asymptomatic. The majority was female and the main complaint was about dysphonia. Before the inspiratory maneuver, the most observed lesions in both groups were chronic laryngitis, followed by vascular dysgenesis. After the inspiratory maneu- Keywords ver, sulcus vocalis was the most frequent additional finding. -

Benign Thyroid Disease and Vocal Cord Palsy
Annals of the Royal College ofSurgeons of England (1993) vol. 75, 241-244 Benign thyroid disease and vocal cord palsy Julian M Rowe-Jones MB FRCS Susanna E J Leighton MB FRCS Registrar in Otolaryngology Senior Registrar in Otolaryngology R Paul Rosswick MS FRCS Consultant General Surgeon St George's Hospital and Medical School, London Key words: Multinodular goitre; Thyroid adenoma; Graves' disease; Hashimoto's thyroiditis; Vocal cord palsy The case notes of 2453 consecutive patients admitted for intrinsic laryngeal muscles including cricothyroid, there- thyroid surgery and with successful preoperative laryngo- by suggesting vagal or concurrent superior and recur- scopy were examined retrospectively. Of the 2408 patients rent laryngeal nerve involvement (1). who had not had previous operations on the gland, 2321 proved to have benign pathology. A total of 29 patients had a preoperative vocal cord palsy of which 22 were associated Materials and methods with benign disease. Return of cord movement after surgery occurred in 89% of the patients with a benign goitre. We advocate routine preoperative laryngoscopy to detect vocal The case records of 2453 consecutive patients undergoing cord paresis. Such a finding with a goitre does not necessar- thyroid surgery between 1947 and 1992, who had had ily indicate malignancy. The recurrent laryngeal nerve successful preoperative laryngoscopy, were analysed should therefore be identified at surgery and preserved to retrospectively. Laryngoscopy had been performed allow for recovery of vocal cord movement. indirectly using a mirror, or in the last 11 years with a flexible, fibreoptic nasendoscope when mirror examin- ation had been unsuccessful. The patients all had their vocal cord assessments performed by a registrar, senior Goitre with hoarseness is usually considered a portent of registrar or consultant. -

Adult Outcome of Congenital Lower Respiratory Tract Malformations M S Zach, E Eber
500 Arch Dis Child: first published as 10.1136/adc.87.6.500 on 1 December 2002. Downloaded from PAEDIATRIC ORIGINS OF ADULT LUNG DISEASES Series editors: P Sly, S Stick Adult outcome of congenital lower respiratory tract malformations M S Zach, E Eber ............................................................................................................................. Arch Dis Child 2002;87:500–505 ongenital malformations of the lower respiratory tract relevant studies have shown absence of the normal peristaltic are usually diagnosed and managed in the newborn wave, atonia, and pooling of oesophageal contents.89 Cperiod, in infancy, or in childhood. To what extent The clinical course in the first years after repair of TOF is should the adult pulmonologist be experienced in this often characterised by a high incidence of chronic respiratory predominantly paediatric field? symptoms.910 The most typical of these is a brassy, seal-like There are three ways in which an adult physician may be cough that stems from the residual tracheomalacia. While this confronted with this spectrum of disorders. The most frequent “TOF cough” is both impressive and harmless per se, recurrent type of encounter will be a former paediatric patient, now bronchitis and pneumonitis are also frequently observed.711In reaching adulthood, with the history of a surgically treated rare cases, however, tracheomalacia can be severe enough to respiratory malformation; in some of these patients the early cause life threatening apnoeic spells.712 These respiratory loss of lung tissue raises questions of residual damage and symptoms tend to decrease in both frequency and severity compensatory growth. Secondly, there is an increasing with age, and most patients have few or no respiratory number of children in whom paediatric pulmonologists treat complaints by the time they reach adulthood.13 14 respiratory malformations expectantly; these patients eventu- The entire spectrum of residual respiratory morbidity after ally become adults with their malformation still in place. -

Idiopathic Subglottic Stenosis: a Review
1111 Editorial Section of Interventional Pulmonology Idiopathic subglottic stenosis: a review Carlos Aravena1,2, Francisco A. Almeida1, Sanjay Mukhopadhyay3, Subha Ghosh4, Robert R. Lorenz5, Sudish C. Murthy6, Atul C. Mehta1 1Department of Pulmonary Medicine, Respiratory Institute, Cleveland Clinic, Cleveland, OH, USA; 2Department of Respiratory Diseases, Faculty of Medicine, Pontificia Universidad Católica de Chile, Santiago, Chile; 3Department of Pathology, Robert J. Tomsich Pathology and Laboratory Medicine Institute, 4Department of Diagnostic Radiology, 5Head and Neck Institute, 6Department of Thoracic and Cardiovascular Surgery, Heart and Vascular Institute, Cleveland Clinic, Cleveland, OH, USA Contributions: (I) Conception and design: C Aravena, AC Mehta; (II) Administrative support: All authors; (III) Provision of study materials or patients: All authors; (IV) Collection and assembly of data: C Aravena, AC Mehta; (V) Data analysis and interpretation: All authors; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors. Correspondence to: Atul C. Mehta, MD, FCCP. Lerner College of Medicine, Department of Pulmonary Medicine, Respiratory Institute, Cleveland Clinic, 9500 Euclid Ave, A-90, Cleveland, OH 44195, USA. Email: [email protected]. Abstract: Idiopathic subglottic stenosis (iSGS) is a fibrotic disease of unclear etiology that produces obstruction of the central airway in the anatomic region under the glottis. The diagnosis of this entity is difficult, usually delayed and confounded with other common respiratory diseases. No apparent etiology is identified even after a comprehensive workup that includes a complete history, physical examination, pulmonary function testing, auto-antibodies, imaging studies, and endoscopic procedures. This approach, however, helps to exclude other conditions such as granulomatosis with polyangiitis (GPA). It is also helpful to characterize the lesion and outline management strategies. -
Paediatric Airway Problems
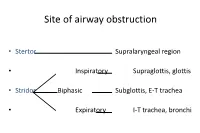
Site of airway obstruction • Stertor Supralaryngeal region • Inspiratory Supraglottis, glottis • Stridor Biphasic Subglottis, E-T trachea • Expiratory I-T trachea, bronchi Investigation of Stridor • History • Examination • Radiological investigations • Endoscopy History • Neonatal intubation • Stridor / stertor • Voice / cry • Cough / cyanotic attacks • Feeding difficulties • Failure to thrive Examination • Pallor, cyanosis • Tracheal tug, sternal recession, intercostal / subcostal recession • Pectus excavatum, Harrison’s sulci • Stridor / stertor • Voice / cry • Cough Site of Airway Obstruction Stridor Voice Cough Supralaryngeal Stertor Muffled - region Supraglottis, Inspiratory Hoarse Barking glottis Subglottis, E-T Biphasic Normal Brassy trachea I-T trachea, Expiratory Normal + bronchi Site of Airway Obstruction • Pharyngeal (stertor): - worse when asleep • Laryngeal, tracheal or bronchial (stridor): - worse when awake, especially if stressed Radiological investigations • Soft-tissue lateral neck X-ray • PA chest X-ray • Cincinnati (high-kv filter) view • ? Barium swallow • ? Bronchogram Endoscopy • The definitive investigation for a child with stridor Endoscopy • Awake flexible fibreoptic laryngoscopy • Suitable for infants using simple restraint • Screening investigation for laryngomalacia • May be helpful in assessing vocal cord palsy • But only gives a view of the supraglottis • Does not exclude coexisting lower airway pathology Endoscopy • Microlaryngoscopy + Bronchoscopy • “The Gold Standard” Total airway endoscopies at GOS 9,341 -

A Cause of Acute Stridor T Jaiganesh, a Bentley
666 CASE REPORTS Emerg Med J: first published as 10.1136/emj.2003.009886 on 19 August 2005. Downloaded from Hereditary motor and sensor neuropathy: a cause of acute stridor T Jaiganesh, A Bentley ............................................................................................................................... Emerg Med J 2005;22:666–667. doi: 10.1136/emj.2003.009886 We present an acute stridor secondary to bilateral vocal cord Table 1 Clinical presentation of HMSN related to the paresis in a patient with demyelinating form (type I) of genetic defects hereditary motor and sensory neuropathy (HMSN). Management problems are discussed and HMSN reviewed. Age of Chromo- onset (in Early Tendon Type some years) symptoms reflexes HMSN 1: dominant; demyelinating 1 A 17 5–10 Distal Absent 48 year old female attended the emergency department weakness with complaints of cough, breathing difficulty, and 1 B 1 5–10 Distal Absent Aflu-like symptoms for one day. She suffers from weakness hereditary motor and sensory neuropathy (HMSN) Type Ia, 1 C Unknown 10–15 Distal Reduced weakness which had been detected by isolating DNA from a blood 1D 10 10–15 Distal Absent sample for the presence of duplication on Chromosome 17. weakness She had been treated for asthma for two years and had X X 10–15 Distal Absent a history of nocturnal choking episodes. Examination weakness HMSN 2: dominant; revealed inspiratory stridor with indrawing of neck axonal muscles. The ear, nose, and throat (ENT) surgeons, con- 2 A 1 10 Distal Absent sultant anaesthetist, and intensivist were contacted. ENT weakness examination through a fibre optic flexible laryngoscope 2 B 3 10–20 Distal Absent weakness revealed smooth white paramedian position of the vocal Sensory loss cords, which were not swollen. -

Transient Bilateral Vocal Cord Paralysis After Endotracheal Intubation with Double-Lumen Tube -A Case Report
Korean J Anesthesiol 2010 December 59(Suppl): S9-S12 Case Report DOI: 10.4097/kjae.2010.59.S.S9 Transient bilateral vocal cord paralysis after endotracheal intubation with double-lumen tube -A case report- Dae Myoung Jeong1, Gunn Hee Kim2, Jie Ae Kim1, and Sangmin Maria Lee1 Department of Anesthesiology and Pain Medicine, 1Samsung Medical Center, Sungkyunkwan University School of Medicine, 2National Medical Center, Seoul, Korea Vocal cord paralysis is one of the most serious anesthetic complications related to endotracheal intubation. The practitioner should take extreme care, as bilateral vocal cord paralysis can obstruct the airway and lead to disastrous respiratory problems. There have been many papers on bilateral vocal cord paralysis after neck surgery, but reports on such a condition after lung surgery are very rare. We report a case of bilateral vocal cord paralysis detected after removal of a double-lumen endotracheal tube in a 67-year-old patient who underwent wedge resection by video- assisted thoracoscopic surgery. We also note that he recovered spontaneously without complications within a day. (Korean J Anesthesiol 2010; 59: S9-S12) Key Words: Bilateral vocal cord paralysis, Double-lumen endotracheal tube, Postoperative stridor. Bilateral vocal cord paralysis is widely known to be a com- Case Report plication of general anesthesia [1,2]. There have been few reports, however, of bilateral vocal cord paralysis related to a A 67-year-old man, 164.5 cm in height and 64.7 kg in weight, double-lumen endotracheal tube (DLT) [3]. was admitted to the hospital for investigation of abnormal We encountered a patient with bilateral vocal cord paralysis, shadows on chest X-ray in both lungs.