July 2019 GF Newsletter and Recipes
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Mixed Grille Entrees
Creative Catering PAGES General Information 2 - 3 Hors D’oeuvres 4 - 5 Party Trays 6 Breakfast Buffets 7 Deli Style Lunch Buffets 8 Working Bag Lunches 9 Specialty Salad Creation 10 Buffet Cuisine / Accompaniments 11 - 12 Themed Buffets 13 - 14 Plated Cuisine / Accompaniments 15 - 17 Desserts 18 Beverages 19 Homemade Soups 20 For Personalized Service, Please Call Us at (563) 582-5100 General Information Creative Catering Creative Catering is proud to present innovative and delicious cuisine, a step ahead of the tra- ditional, for all of your catering needs. Our specialized styles of menus and services are availa- ble to accommodate all size groups at many budgetary levels. We pride ourselves on custom tailoring catering services and menu concepts based on each customer’s individual needs. We will do our best to fill every request. Our expertise of catering and event planning covers a broad spectrum of clientele from simplistic corporate and social gatherings, festive holiday celebrations, corporate picnics to elaborate affairs featuring thousands of enchanted guests. Our Guarantee We guarantee total satisfaction and on-time service. The creative catering manager is always available to assist you with expert special event planning and orchestration. Placing an Order Call Creative Catering at 563.582.5100. Standard orders should be placed 48 hours prior to the start of your event, to ensure product availability. For placing orders for special services or items, we recommend placing your order two to three weeks in advance. When making a reservation, please provide the following information: Date and time of catered event Number of attendees Location of event and building Contact name and phone numbers Name of person holding event/type of event Pick-up time All orders will be delivered within a 30-minute window prior to your serving time. -

Mondays to Sundays Dial 19 for Room Service
6:00AM - 11:30PM | MONDAYS TO SUNDAYS DIAL 19 FOR ROOM SERVICE BREAKFAST American Breakfast P250 Breakfast Burrito P250 • Two fried eggs Sausage patty, bacon, 2 pieces eggs, hash brown with • Ham or Crispy Bacon cilantro leaves wrapped in tortilla, • Bread, butter & jam served with sliced tomatoes • Coffee or tea and grilled button mushrooms on the side • Chilled orange juice or sliced fresh fruit in season with choice of coffee, tea or chilled orange juice. Filipino Breakfast P250 Dirty Breakfast P269 • Two fried eggs Our version of the English breakfast: crispy bacon • Choice of Beef Tapa, Pork Longganisa, Chicken and sausage patty, two fried eggs, beans served Longganisa, Skinless Longganisa, Pork Tocino, with hash browns and grilled button mushrooms, Chicken Tocino, or Corned Beef with choice of coffee, tea or chilled orange juice. • Garlic fried rice • Pickled papaya Pancake/Waffles P120 • Coffee or tea Served with butter and maple syrup • Chilled orange juice or sliced fresh fruit in season with ham P180 with bacon P220 Breakfast Ala Carte Fried Eggs P100 Extra Bacon P120 Plain Bread P80 Plain Omelette P100 Oatmeal with Fresh Milk P100 Wheat Bread P80 Vegetable Omelette P120 Cornflakes with Fresh Milk P100 Garlic Bread P80 Ham & Cheese Omelette P150 SOUP Cheddar Broccoli Soup P150 Minestrone Soup P120 Rich cheddar cheese perfectly balanced A hearty Italian clear soup made wholesome flavorful with fresh broccoli. Served with a slice of toast. vegetables. Served with a slice of toast. Cream of Zucchini Soup Cream of Mushroom Soup P120 with Herbs P130 Creamy mushroom soup topped with croutons. Freshly pureed zucchini in a creamy soup. -

Taste of Homemakers 2012 Recipe Book
2 APPETIZERS/SNACKS Jean’s Cheese Ball Imogene Jordan, Anthoston Homemakers INGREDIENTS — 2 (8 oz.) pkgs. cream cheese 1 (8 oz.) pkg. shredded Cheddar cheese 1 Tablespoon finely chopped onion 1 Tablespoon finely chopped green pepper 1 (2 oz.) jar diced pimento Garlic powder to taste Chopped pecans DIRECTIONS — Mix the cream cheese and cheddar cheese, then add in onion, green pepper, pimento and garlic powder. Stir to mix ingredients well. Chill in refrigerator for an hour or more then form into a ball. Roll in chopped pecans to coat. Serve with crackers. Stuffed Celery Jeanette New, The Village Homemakers INGREDIENTS — Cream Cheese Chopped pecans DIRECTIONS — Mix well and stuff celery. NOTE: May substitute peaches and/or pineapple for pecans. Teriyaki Chicken Wings Marilyn Watson, Town and Country Homemakers INGREDIENTS — 3 lbs. chicken wings 3/4 teaspoon pepper 1/4 teaspoon garlic powder 1/3 cup lemon juice 1/4 cup catsup 1/4 cup soy sauce 1/4 cup oil 2 Tablespoons brown sugar DIRECTIONS— Mix sauce, then add chicken and marinate overnight in refrigerator. Arrange in a single layer baking dish and cook until done. Bake at 350 degrees for 45 minutes. 3 Bud’s Best Cheese Ball Karen Hill, Town & Country Homemakers INGREDIENTS — 8 oz. cream cheese 8 oz. reduced fat cream cheese 1/2 cup Stonewall Kitchen Apple Cranberry OR Old Farmhouse Chutney 4 green onions, diced (approximately 1/4 cup) 1 clove garlic, minced Dash of salt Dash of pepper 1 cup shredded Colby-Jack cheese 1/2 cup finely chopped pecans DIRECTIONS — Mix together the cream cheeses, chutney, onion, garlic, salt and pepper. -

During Exercise
How do you review safety & sanitation? How do you teach knife skills? Talk about knife cuts, demonstrate with potatoes, practice on potatoes, 2 per person, and then fry potatoes or bake with variety of seasonings. Use youtube videos to show knife cuts Paper is used to see the size of the cuts Review sanitation then make chicken Caesar salad. One person is designated as the safety supervisor. Case study of student that is doing things that are wrong. Show the bacteria found on a cell phone. Keep phones put away during labs. Poison Picnic – CDC Website Knife skills use knox gelatin in sheet pans, cut then melt down and reuse Cut veggies then use the next day in a soup lab, make French fries, vegetable tray Kahoot for review game Glo germ – toss a ball and then check hands in black light Set up kitchens with mistakes have students identify them, caution tape to rope off Kitchen ninja game – New Mexico state univeristy Knife skills, frittata. Make all knife cuts with paper and a ruler, cut up and put in an envelope Relay with knife skills What labs do you do? Safety & Sanitation- 3 different dips, chicken stir fry, cream of tomato soup, salsa demo Steak stir fry, whole wheat turkey wrap, eggs benedict Yeast breads – 2 day cinnamon rolls, pretzels, angel rolls, scones with cinnamon buter Consumerism – calzones, different types of mac & cheese Crunch wraps – like taco bell http://life-in-the-lofthouse.com/taco-bell-crunchwrap-supreme-copycat/ Create your own salad from basic supplies Chicken strips with Haney mustard sauce Recipes with less -

Connections Member Newsletter - December 2017
CONNECTIONS MEMBER NEWSLETTER - DECEMBER 2017 Holiday Brunch Stunning decorations, exquisite food, live music & a visit from Santa await! Page 4 Holiday Workshop Holiday Cocktail Party Heather Moore Jewelry Show Join us for this family-friendly event, This year's festivities include Find the perfect gifts for the holidays in which you and your children can hors d'oeuvres, custom while supporting your Club! create homemade keepsakes! cocktails and prizes. Page 4 Page 5 Page 8 NEW MEMBERSHIP FOR PROSPECTIVE MEMBERS If someone you refer joins under MONDAY the Centennial Plan, 1 2 you'll receive a $50 gift certificate! 4 5 6 7 8 9 THE CENTENNIAL MEMBERSHIP 11 12 13 14 15 16 Celebrating our Connection to the Community & 100 Years on E. Wilson ROUNDTABLE LUNCH 12 PM 18 19 20 21 22 23 IT’S OUR ANNIVERSARY, BUT YOU (AND YOUR REFERRALS) GET THE BENEFITS! MONTHLY PAYMENT: $100 = Only $50 in dues + $50 for YOU to spend on food, 25 26 27 28 29 30 beverage, and event admission purchases CLUB CLOSED ONE-TIME INITIATION: $100 off standard fee of $500 Referring member enjoys a $50 gift certificate for each Why Refer? new member. Help us reach our goal of recruiting 100 new members in our building's 100th year. 02 For more information, please contact Krista Laubmeier: [email protected] or 608-255-4861. www.madisonclub.org CLUB HOURS DECEMBER 2017 Mon. - Thurs.: 7 AM - 10:30 PM MONDAY TUESDAY WEDNESDAY THURSDAY FRIDAY SATURDAY Fridays: 7 AM - 11 PM 1 2 Saturdays: 4 PM - 11 PM Sundays: Closed FISH FRY SPECIAL BREAKFAST: Complimentary coffee and pastries in Churchill’s Lounge Weekdays: 7 - 9:30 AM 4 5 6 7 8 9 LUNCH: LADIES BRIDGE FISH FRY HOLIDAY Weekdays: 11:30 AM - 2 PM 11:30 AM SPECIAL WORKSHOP 9:00 AM DINNER: Monday - Saturday: 5 - 9 PM HEATHER 10 B. -

Plane Crash Kills 5 Soldiers
(Periodicals postage paid in Seattle, WA) TIME-DATED MATERIAL — DO NOT DELAY In Your Neighborhood Norwegian Heritage Who will wear How Jell-O the Miss Norway En sann venn betyr mer for vår lykke enn tusen fiender changed crown? for vår ulykke. everything Read more on page 13 – Marie von Ebner-Eschenbach Read more on page 14 Norwegian American Weekly Vol. 123 No. 12 March 23, 2012 Established May 17, 1889 • Formerly Western Viking and Nordisk Tidende $1.50 per copy Norway.com News Find more at www.norway.com Plane crash kills 5 soldiers News Apple, the world’s most valuable Military exercise company with a market value of turns deadly with more than USD 550 billlion, beats the Norwegian pension mountain crash in fund in value. The Norwegian state pension fund reported their northern Sweden 2011 results on March 16. The year-end balance amounted to NOK 3.312 billion, slightly less STAFF COMPILATIO N than the market value of Apple, Norwegian American Weekly after reporting a loss of NOK 86 billion last year. Interestingly enough, Apple was the Pension Fund’s single most profitable in- Five Norwegian aviation of- vestments last year. fers died when the Norwegian (blog.norway.com/category/ military transport aircraft Hercules news) C 130-J went missing in northern Sweden on March 15. The aircraft Culture and officers were participating in Frustration over Stockholm’s the international military exercise claim to be the “Capital of Scan- “Cold Response,” with 14 coun- dinavia” has reached new levels, tries represented by more than as angry Norwegian delegates 16,000 soldiers. -
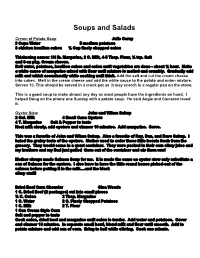
Soups and Salads
Soups and Salads Cream of Potato Soup Julie Cerny 3 Cups Water 5 medium potatoes 3 chicken bouillon cubes ½ Cup finely chopped onion Thickening sauce: 1/4 lb. Margarine, 2 C. Milk, 45 Tbsp. Flour, ½ tsp. Salt and 8oz pkg. Cream cheese. Boil water, potatoes, bouillon cubes and onion until vegetables are done about ½ hour. Make a white sauce of margarine mixed with flour until mixture is melted and crumbly. Gradually add milk and whisk occasionally while cooking until thick. Add the salt and cut the cream cheese into cubes. Melt in the cream cheese and add the white sauce to the potato and onion mixture. Serves 10. This should be served in a crock pot as it may scorch in a regular pan on the stove. This is a good soup to make almost any day as most people have the ingredients on hand. I helped Doug on the phone one Sunday with a potato soup. He said Angie and Cameron loved it. Oyster Stew John and Wilma Sukup 2 Gal. Milk 4 Small Cans Oysters 4 T. Margarine Salt & Pepper to taste Heat milk slowly, add oysters and simmer 10 minutes. Add margarine. Serve. This was a favorite of John and Wilma Sukup. Also a favorite of Ray, Dan, and Dave Sukup. I hated the grainy taste of the oysters. Mother used to order these little beasts fresh from the grocery. They would come in a quart container. They were packed in their own slimy juice and my brothers and my Dad just pulled them out of the container and ate them raw! Mother always made Salmon Soup for me. -

Stephanie Plum and I’M a Fugitive Apprehension Agent in Trenton, New Jersey
Thank you for downloading this Simon & Schuster ebook. Get a FREE ebook when you join our mailing list. Plus, get updates on new releases, deals, recommended reads, and more from Simon & Schuster. Click below to sign up and see terms and conditions. CLICK HERE TO SIGN UP Already a subscriber? Provide your email again so we can register this ebook and send you more of what you like to read. You will continue to receive exclusive offers in your inbox. For Carolyn Reidy A remarkable lady who was always a champion for me and Stephanie. CHAPTER ONE My name is Stephanie Plum and I’m a fugitive apprehension agent in Trenton, New Jersey. I’m not especially brave, so you would think I’d pretty much stay out of trouble. Unfortunately, I occasionally ignore the obvious signs of danger and stumble into something ugly with the potential for disaster. This was one of those times. I was in a tunnel under a strip club, and I was with my coworker, Lula. “This is a bad idea,” Lula said to me. “My nipples are all shrunk up and trying to hide inside my body. It’s like what men’s gonads do when someone comes at them with a butcher knife. Those suckers abandon ship and there’s nothing left but an empty nut sack. Not that I know rsthand. I’m just sayin’ what I hear.” Aside from being a bounty hunter, I think I’m pretty normal. I have shoulder-length curly brown hair that’s usually pulled back into a ponytail, blue eyes from my mother’s Hungarian ancestors, and a bunch of rude hand gestures from my father’s Italian side of the family. -

South Dakota State University Farmhouse Fraternity Cookbook
6outb llakota 6tate ltnibtr�ttp jfarmT!,ou�t jfrattrnttp · Cookbook � '( (_� 'i..J _Q___:-., ,�,..,.,\ s .s k, � \ 9� �3S'-\'2_'3,'-\-0 , - ----- ·-· ,r,f.• , ...'- 11iln� i. I I n1: - I •I I , ·•·i"l', h �,,! If there is one thingthat the men of FannHouse can agreeon it is thatthey likeFOOD! However, they do express differences of opinion on their favorite food items. In aneffort to compile a collection of recipes which are"FarmH ouse favorites", the idea for this recipe book began. It is our hope that this cook book will makem eal planning easier at FannHouseand at your house. Thank you for your support. Deb DeBates, Housemother 1991 � Present Paul H Hoffer, Alumni Relations Chairman 1994 FannHouseFraternity@ TheObject 'The object of our Fr.uemity is 10 promocc 800d fellowship, 10 enco..... studiousness. and to inspire its memben in scelcin1 the best in their chosen lines of study u well u in life. Propess shall mark our every step: the spirit of con1eniality shall reip at all times; and every member shall be honest witb himselfas widl his brc,Chen. Men elected to ourmembenbip are considered to be of aood moral cbancter, to be hiah in scholarship. to have the capacity for imecinl ud mati.. frieDds. ud ID pve promise of service IO their fellowmea 111dto lbeworld. To beMd becomesuch may• timesrequR a sacrifice of li11111. pleasureMd comfona. The abovestatement is theessence ofFann HomeFraternity. Fromthe first Fanni-louseClub meeting on February8, I 965,that was attendedby 12 men. to the mostrecently held chapter meeting that 49 attend.F annHouseMembers have prided themselveson canying out the Object's words. -

608.755.4123 Soup-Er Fall Buffet Traditional
2020 608.755.4123 www.besteventscatering.com Soup-er Fall Buffet Traditional CHOICE OF two soups Thanksgiving Buffet Roasted Red Pepper & Tomato Soup Tossed Salad with Assorted Dressings Ham & Potato Corn Chowder Sage Stuffing Autumn Wild Rice Mashed Potatoes with Turkey Gravy Creamy Butternut Squash Soup Sliced Light & Dark Roasted Turkey Meat Classic Beef Stew Chicken Tortilla Soup Buttered Green Beans Homestyle Creamy Chicken Noodle Cranberry Sauce Pumpkin Pie Served with Crusty French Bread Slices, Butter and Crackers. Herb Dinner Rolls souper fall buffet Thanksgiving buffet $8.25 per person $16.25 per person Oktoberfest Buffet North Woods Buffet Bavarian Beer Cheese Dip with Pretzel Bites Organic Spring Greens Fruchtsalat Mit Nussen drizzled with cranberry vinaigrette dressing & topped with fresh fruit salad with nuts sliced cucumbers, sliced radish & vine ripened tomatoes Roasted Chicken n’ Spaetzle roasted chicken and German dumplings with Herb Encrusted Roast Pork Loin onion in a brown butter cream sauce with Door County cherry port wine reduction Beer & Onion Roasted Bratwurst Redskin Garlic Mashed Potatoes with buns & kraut on the side Green Beans with Dill Tarragon Cognac Glazed Baby Carrots Potato Pancakes with hot homemade apple sauce Herb Dinner Rolls Oktoberfest Buffet North Woods buffet $15.85 per person $14.95 per person Wisconsin Bountiful Buffet Tossed Garden Salad with Assorted Dressings Rustic Roasted Garlic Chicken Breast with Asiago Gravy Beef Tips with Mushrooms & Onions Buttered Egg Noodles Garlic Roasted Vegetables with Oregano & Basil Butter Herbed Dinner Rolls & Butter Bountiful buffet $16.95per person LIKE WHAT YOU SEE? CONTACT US TO BOOK YOUR NEXT MEAL! 608-755-4123 | [email protected] Harvest Box Lunch Specials You must order a Minimum of 5 of each kind of lunch or a surcharge of $2.75 per lunch will apply. -

About the Menu & Meal Service Billing & Payment
Catering Menu Phone: 701-320-9280 ~ Web: www.jamestownNDcatering.com Email: [email protected] Thank you for considering Emma Rosie’s Homecookin’ for your next event! Please be sure to read this page in its entirety before browsing through the menu; it will likely answer many questions that may arise. Please call or email with questions and for our availability for your event date. Please note that we do generally require a minimum of forty guests for a catered event, however we may be able to accommodate smaller groups depending on our schedule, so please do ask. About the Menu & Meal Service Your meal is not necessarily limited to the items on this menu; we can present you with custom options if the items listed here don't suit your event! If you have any special requests for your meal, please let us know, and we will do our best to accommodate. Special dietary needs can generally be accommodated if advance notice is given. All menu items may not be available for all size groups or at all venues; please confirm your choices with us before printing menus, etc. for your event. The prices listed on this menu include buffet-style service, tended when appropriate, and upscale disposable dinnerware. Samples of disposables are available for viewing upon request. Special order disposables are also available. Stoneware dishes, stainless utensils, and glassware may be available for use depending on venue. Table service is available. Cake service is available. When you choose us, you will always receive well-presented, flavorful, quality food and personal service including professional, helpful staff to ensure the service at your event goes smoothly. -

House Dinner Menu Details
House Dinner Menu Details Mission: The Ronald McDonald House of Rochester, Minnesota provides a home-away-from-home and caring support to families seeking medical care for their children. Our House Dinner program offers children and families staying at our House the comfort of a warm and delicious meal, prepared with love from our caring community. MENU REQUIREMENTS • The healthy balanced menu is up to your group; please check other dates for menus surrounding yours to avoid meal redundancy. Required: Main dish, side dish, salad and/or vegetable Optional: Fruit, bread/rolls, dessert, beverages We have tap water and lemonade mix available onsite for use. We have lots of spaghetti and taco nights at our House. If desired to do either option, please make it a pasta or taco bar with choices. We have cookies available daily for families, if providing a dessert with dinner, please consider a fun and exciting alternative such as bars, brownies, pie, etc. Groups are not required to offer vegetarian or other special dietary options, but are welcome to. Gluten-friendly items can be prepared, but we are not a gluten-free kitchen. Be aware of common food allergies in Do not serve the food served o Milk o Unpasteurized milk & juice o Eggs o Cheese made from unpasteurized milk o Peanuts o Raw sprouts (alfalfa, bean, or other) o Tree nuts (almonds, walnuts, pecans) o Raw or uncooked meat, fish, eggs o Soybeans o Alcohol: prohibited from RMH grounds, o Wheat including use of alcohol as an ingredient o Fish o Shellfish Per US Department of Agriculture Per US Food & Drug Administration (FDA) MENU IDEAS Main Course • Pasta Bar: variety of noodles, sauces: marinara, Alfredo, cheese, pesto, meat-sauce; toppings: meatballs, grilled chicken, sausage, steamed veggies, parmesan cheese, crushed red pepper, basil, etc.