Malposition of Central Venous Catheter in the Jugular Venous Arch Via
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Unusual Venous Drainage of the Common Facial Vein. a Morphologycal Study ORIGINAL
International INTERNATIONAL ARCHIVES OF MEDICINE 2018 Medical Society SECTION: HUMAN ANATOMY Vol. 11 No. 29 http://imedicalsociety.org ISSN: 1755-7682 doi: 10.3823/2570 Unusual Venous Drainage of the Common Facial Vein. A Morphologycal Study ORIGINAL Sergio Ivan Granados-Torres1, Humberto Ferreira-Arquez2 1 Medicine student sixth Semester, University of Pamplona, Norte de Abstract Santander, Colombia, South America 2 Professor Human Morphology, Medicine Background: Anatomical knowledge of the facial vasculature is cru- Program, University of Pamplona, Morphology Laboratory Coordinator, cial not only for anatomists but also for oral and maxillofacial surgery, University of Pamplona. plastic surgeon, otorhinolaryngologists. Access pathways, pedicled and free flap transfer, and explantation and transplantation of total Contact information: faces are based on the proper assessment and use of the facial veins and arteries. The anatomical variations reported in the present study Ivan Granados-Torres. confirms the need for preoperative vascular imaging for sure good Address: University Campus, Kilometer venous outflow for the free flap survival. 1. Via Bucaramanga. Norte de Santander, Colombia. Suramérica, Pamplona Zip code: Aims: The aim of the present study was to describe a rare anato- 543050 Tel: 573176222213 mical variation of the common facial vein which not been previously described. [email protected] Methods and Findings: Head and neck region were carefully dissected as per standard dissection procedure, studied serially during the years 2013-2017 in 15 males and 2 females, i.e. 34 sides, embal- med adults cadavers with different age group, in the laboratory of Morphology of the University of Pamplona. In 33 sides (97 %) of the cases the anterior facial vein (FV) terminated into the internal jugular vein via the common facial vein (CFV) as per standard anatomic des- cription. -

A Rare Variation of Superficial Venous Drainage Pattern of Neck Anatomy Section
ID: IJARS/2014/10764:2015 Case Report A Rare Variation of Superficial Venous Drainage Pattern of Neck Anatomy Section TANWI GHOSAL(SEN), SHABANA BEGUM, TANUSHREE ROY, INDRAJIT GUPta ABSTRACT jugular vein is very rare and is worth reporting. Knowledge Variations in the formation of veins of the head and neck of the variations of external jugular vein is not only important region are common and are well explained based on their for anatomists but also for surgeons and clinicians as the embryological background. Complete absence of an vein is frequently used for different surgical procedures and important and major vein of the region such as external for obtaining peripheral venous access as well. Keywords: Anomalies, External jugular vein, Retromandibular vein CASE REPOrt the subclavian vein after piercing the investing layer of deep During routine dissection for undergraduate students in the cervical fascia [1]. Apart from its formative tributaries, the Department of Anatomy of North Bengal Medical College, tributaries of EJV are anterior jugular vein, posterior external Darjeeling, an unusual venous drainage pattern of the head jugular vein, transverse cervical vein, suprascapular vein, and neck region was found on the right side in a middle aged sometimes occipital vein and communications with internal female cadaver. The right retromandibular vein (RMV) was jugular vein [Table/Fig-4]. formed within the parotid gland by the union of right maxillary During embryonic period, superficial head and neck veins and superficial temporal vein. The RMV which was wider than develop from superficial capillary plexuses which will later facial vein continued downwards and joined with the facial form primary head veins. -

Port Placement Via the Anterior Jugular Venous System: Case Report, Anatomic Considerations, and Literature Review
Hindawi Case Reports in Radiology Volume 2017, Article ID 2790290, 5 pages https://doi.org/10.1155/2017/2790290 Case Report Port Placement via the Anterior Jugular Venous System: Case Report, Anatomic Considerations, and Literature Review Gernot Rott and Frieder Boecker Radiological Department, Bethesda-Hospital Duisburg, Heerstr. 219, 47053 Duisburg, Germany Correspondence should be addressed to Gernot Rott; [email protected] Received 14 February 2017; Accepted 28 March 2017; Published 10 April 2017 Academic Editor: Dimitrios Tsetis Copyright © 2017 Gernot Rott and Frieder Boecker. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. We report on a patient who was referred for port implantation with a two-chamber pacemaker aggregate on the right and total occlusion of the central veins on the left side. Venous access for port implantation was performed via left side puncture of the horizontal segment of the anterior jugular vein system (AJVS) and insertion of the port catheter using a crossover technique from the left to the right venous system via the jugular venous arch (JVA). The clinical significance of the AJVS and the JVA forcentral venous access and port implantation is emphasised and the corresponding literature is reviewed. 1. Introduction left-sided central veins with the presence of a cervical collat- eral venous flow from the left to the right side reaching the Venous access for chest port implantation may be compro- nonoccluded right-sided central veins, specifically the con- mised for a variety of reasons and finding a suitable alter- fluence to the right innominate vein (IV) and, as part of the native can be difficult. -
27. Veins of the Head and Neck
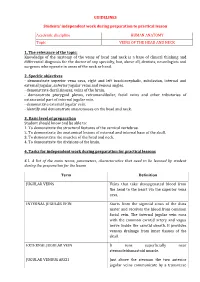
GUIDELINES Students’ independent work during preparation to practical lesson Academic discipline HUMAN ANATOMY Topic VEINS OF THE HEAD AND NECK 1. The relevance of the topic: Knowledge of the anatomy of the veins of head and neck is a base of clinical thinking and differential diagnosis for the doctor of any specialty, but, above all, dentists, neurologists and surgeons who operate in areas of the neck or head. 2. Specific objectives - demonstrate superior vena cava, right and left brachiocephalic, subclavian, internal and external jugular, anterior jugular veins and venous angles. - demonstrate dural sinuses, veins of the brain. - demonstrate pterygoid plexus, retromandibular, facial veins and other tributaries of extracranial part of internal jugular vein. - demonstrate external jugular vein. - identify and demonstrate anastomoses on the head and neck. 3. Basic level of preparation Student should know and be able to: 1. To demonstrate the structural features of the cervical vertebrae. 2. To demonstrate the anatomical lesions of external and internal base of the skull. 3. To demonstrate the muscles of the head and neck. 4. To demonstrate the divisions of the brain. 4. Tasks for independent work during preparation for practical lessons 4.1. A list of the main terms, parameters, characteristics that need to be learned by student during the preparation for the lesson Term Definition JUGULAR VEINS Veins that take deoxygenated blood from the head to the heart via the superior vena cava. INTERNAL JUGULAR VEIN Starts from the sigmoid sinus of the dura mater and receives the blood from common facial vein. The internal jugular vein runs with the common carotid artery and vagus nerve inside the carotid sheath. -

Thyroid Gland- Surgical Anatomy
Thyroid Gland- Surgical Anatomy March 2019 VARSHNEY UG Lecture 1 Bi-lobed gland over 2nd & 3rd tracheal ring Weight : 20 – 30 gr March 2019 VARSHNEY UG Lecture 2 Samuel D. Gross – 1866 , Philadelphia A System of Surgery Thyroid surgery: ‘Horrid butchery’ “No honest and sensible surgeon would ever engage in thyroid surgery” March 2019 VARSHNEY UG Lecture 3 1909 Nobel Prize Theodur Kocher (1841-1917) • Mortality: • 1889 – 2.4% • 1900 – 0.18% • Emphasis on meticulous technique • Performed 5000 cases by death in 1917 March 2019 VARSHNEY UG Lecture 4 Thyroidectomy Neck Release Moraitis, Shaha. JSO 2006 •Open the “gift wrap” •Separate fascia from the muscles •Separate strap muscles •Separate sternomastoid muscle March 2019 VARSHNEY UG Lecture 5 Thyroid Gland moves with deglutition Ligament of Berry (Condensation of Pretracheal fascia) Inferior constrictor- 2 parts Thyropharyngeus {Thyroid cartilage} Cricopharyngeus {Cricoid cartilage} [Contraction – Thyroid and cricoid move up] March 2019 VARSHNEY UG Lecture 6 The thyroid gland is a very vascular structure. Superior thyroid artery (ECA), Inferior thyroid artery ( Thyrocervical trunk) Arteria thyroideaima artery (2-12% ) (innominate, subclavian, right common carotid, internal mammary, or the aortic arch. March 2019 VARSHNEY UG Lecture 7 The superior thyroid vein follows the pathway of the superior thyroid artery. The middle thyroid veins directly flow into the internal jugular vein. The inferior thyroid veins can be found just anterior to the trachea and often anastomose with each other March 2019 VARSHNEY UG Lecture 8 Nerve supply March 2019 VARSHNEY UG Lecture 9 SLN Dissection of the superior thyroid vessels parallel to the vessels on surface of thyroid & exposure of SLN. -

Posterior Mediastinum: Mediastinal Organs 275
104750_S_265_290_Kap_4:_ 05.01.2010 10:43 Uhr Seite 275 Posterior Mediastinum: Mediastinal Organs 275 1 Internal jugular vein 2 Right vagus nerve 3 Thyroid gland 4 Right recurrent laryngeal nerve 5 Brachiocephalic trunk 6 Trachea 7 Bifurcation of trachea 8 Right phrenic nerve 9 Inferior vena cava 10 Diaphragm 11 Left subclavian artery 12 Left common carotid artery 13 Left vagus nerve 14 Aortic arch 15 Esophagus 16 Esophageal plexus 17 Thoracic aorta 18 Left phrenic nerve 19 Pericardium at the central tendon of diaphragm 20 Right pulmonary artery 21 Left pulmonary artery 22 Tracheal lymph nodes 23 Superior tracheobronchial lymph nodes 24 Bronchopulmonary lymph nodes Bronchial tree in situ (ventral aspect). Heart and pericardium have been removed; the bronchi of the bronchopulmonary segments are dissected. 1–10 = numbers of segments (cf. p. 246 and 251). 15 12 22 6 11 5 2 1 14 2 23 1 3 21 3 20 24 4 5 4 17 8 5 6 6 15 8 7 8 9 9 10 10 Relation of aorta, pulmonary trunk, and esophagus to trachea and bronchial tree (schematic drawing). 1–10 = numbers of segments (cf. p. 246 and 251). 104750_S_265_290_Kap_4:_ 05.01.2010 10:43 Uhr Seite 276 276 Posterior Mediastinum: Mediastinal Organs Mediastinal organs (ventral aspect). The heart with the pericardium has been removed, and the lungs and aortic arch have been slightly reflected to show the vagus nerves and their branches. 1 Supraclavicular nerves 12 Right pulmonary artery 24 Left vagus nerve 2 Right internal jugular vein with ansa cervicalis 13 Right pulmonary veins 25 Left common carotid artery -

Veins of the Systemic Circulation
O.L. ZHARIKOVA, L.D.CHAIKA VEINS OF THE SYSTEMIC CIRCULATION Minsk BSMU 2020 0 МИНИСТЕРСТВО ЗДРАВООХРАНЕНИЯ РЕСПУБЛИКИ БЕЛАРУСЬ БЕЛОРУССКИЙ ГОСУДАРСТВЕННЫЙ МЕДИЦИНСКИЙ УНИВЕРСИТЕТ КАФЕДРА НОРМАЛЬНОЙ АНАТОМИИ О. Л. ЖАРИКОВА, Л.Д.ЧАЙКА ВЕНЫ БОЛЬШОГО КРУГА КРОВООБРАЩЕНИЯ VEINS OF THE SYSTEMIC CIRCULATION Учебно-методическое пособие Минск БГМУ 2018 1 УДК 611.14 (075.8) — 054.6 ББК 28.706я73 Ж34 Рекомендовано Научно-методическим советом в качестве учебно-методического пособия 21.10.2020, протокол №12 Р е ц е н з е н т ы: каф. оперативной хирургии и топографической анатомии; кан- дидат медицинских наук, доцент В.А.Манулик; кандидат филологических наук, доцент М.Н. Петрова. Жарикова, О. Л. Ж34 Вены большого круга кровообращения = Veins of the systemic circulation : учебно-методическое пособие / О. Л. Жарикова, Л.Д.Чайка. — Минск : БГМУ, 2020. — 29 с. ISBN 978-985-21-0127-1. Содержит сведения о топографии и анастомозах венозных сосудов большого круга кровообраще- ния. Предназначено для студентов 1-го курса медицинского факультета иностранных учащихся, изучающих дисциплину «Анатомия человека» на английском языке. УДК 611.14 (075.8) — 054.6 ББК 28.706я73 ISBN 978-985-21-0127-1 © Жарикова О. Л., Чайка Л.Д., 2020 © УО «Белорусский государственный медицинский университет», 2020 2 INTRODUCTION The cardiovascular system consists of the heart and numerous blood and lymphatic vessels carrying blood and lymph. The major types of the blood ves- sels are arteries, veins, and capillaries. The arteries conduct blood away from the heart; they branch into smaller arteries and, finally, into their smallest branches — arterioles, which give rise to capillaries. The capillaries are the smallest vessels that serve for exchange of gases, nutrients and wastes between blood and tissues. -

Blood Finds a Way: Pictorial Review of Thoracic Collateral Vessels Thomas J
Marini et al. Insights into Imaging (2019) 10:63 https://doi.org/10.1186/s13244-019-0753-3 Insights into Imaging EDUCATIONAL REVIEW Open Access Blood finds a way: pictorial review of thoracic collateral vessels Thomas J. Marini*, Komal Chughtai, Zachary Nuffer, Susan K. Hobbs and Katherine Kaproth-Joslin Abstract In the healthy patient, blood returns to the heart via classic venous pathways. Obstruction of any one of these pathways will result in blood flow finding new collateral pathways to return to the heart. Although significant anatomic variation exists and multiple collateral vessels are often present in the same patient, it is a general rule that the collateral pathways formed are a function of the site of venous blockage. Therefore, knowledge of typical collateral vessel systems can provide insight in localizing venous obstruction and characterizing its severity and chronicity. In addition, knowledge of collateral anatomy can be essential in interventional procedural and/or surgical planning, especially when placing catheters in patients with venous blockage. In this pictorial review, we provide a systematic approach to understanding collateral pathways in patients with venous obstruction in the upper body. Keywords: Veins, Collaterals, Superior vena cava, Superior vena cava syndrome, Thrombosis, Obstruction Key points axillary vein would be expected to produce significantly more shoulder collaterals than a partial blockage of the Venous obstruction occurs secondary to mass effect, same vessel that developed over a shorter timeframe. stenosis, and/or thrombosis. Therefore, an understanding of the most common ven- No matter the site of obstruction, blood always finds ous collateral pathways can provide the insight necessary a way back to the heart via collaterals. -
Review of the Variations of the Superficial Veins of the Neck
Open Access Review Article DOI: 10.7759/cureus.2826 Review of the Variations of the Superficial Veins of the Neck Dominic Dalip 1 , Joe Iwanaga 1 , Marios Loukas 2 , Rod J. Oskouian 3 , R. Shane Tubbs 4 1. Seattle Science Foundation, Seattle, USA 2. Anatomical Sciences, St. George's University, St. George's, GRD 3. Neurosurgery, Swedish Neuroscience Institute, Seattle, USA 4. Neurosurgery, Seattle Science Foundation, Seattle, USA Corresponding author: Joe Iwanaga, [email protected] Abstract The venous drainage of the neck can be characterized into superficial or deep. Superficial drainage refers to the venous drainage of the subcutaneous tissues, which are drained by the anterior and external jugular veins (EJVs). The brain, face, and neck structures are mainly drained by the internal jugular vein (IJV). The superficial veins are found deep to the platysma muscle while the deep veins are found encased in the carotid sheath. The junction of the retromandibular vein and the posterior auricular vein usually form the EJV, which continues along to drain into the subclavian vein. The anterior jugular vein is usually formed by the submandibular veins, travels downward anterior to the sternocleidomastoid muscle (SCM), and drains either into the EJV or the subclavian vein. Other superficial veins of the neck to consider are the superior, middle, and inferior thyroid veins. The superior thyroid and middle thyroid veins drain into the IJV whereas the inferior thyroid vein usually drains into the brachiocephalic veins. Categories: Miscellaneous Keywords: external jugular, vein, superficial, internal jugular, thyroid vein Introduction And Background The external jugular vein (EJV) is the preferred vein when performing a central venous catheterization. -

A Patient Has the Affection of the Head of the Femur of Ischemic Origin Diagnosed
A patient has the affection of the head of the femur of ischemic origin diagnosed. Which artery is damaged? Ramus acetabularis A. femoralis A. illiaca extcrna A. profunda femoris A. umbilicalis A 70-year-old female patient was diagnosed with fracture of left femoral neck accompanied by disruption of ligament of head of femur. The branch of the following artery is damaged: Obturator Femoral External iliac Inferior gluteal Internal pudendal Specify parts of the aorta. The ascending, the arch and the descending parts The cervical, the petrous, the cavernous and cerebral parts The prevertebral, the cervical, the atlantic and intracranial parts The cervical, the atlantic and intracranial parts The cerebral part Specify parts of the descending aorta. The thoracic and abdominal parts The cervical, the petrous, the cavernous and cerebral parts The prevertebral, the cervical, the atlantic and intracranial parts The cervical, the atlantic and intracranial parts The ascending, the arch and the descending parts The narrowing of large vessel caused worsening of outflow of blood from the left ventricle. Which vessel has undergone pathological changes? Aorta Pulmonary trunk Pulmonary vein Superior vena cava Inferior vena cava A woman underwent an operation because of extrauterine (tubal) pregnancy. In course of the operation the surgeon should ligate the branches of the following arteries: Uterine and ovarian Superior cystic and ovarian Inferior cystic and ovarian Uterine and superior cystic Uterine and inferior cystic Specify the terminal branches of the abdominal aorta. The right and left common iliac arteries The median sacral artery The left gastric artery The lateral sacral artery and lumbar arteries The coeliac trunk and superior mesenteric artery Sick woman, 48 years old, needs in surgical intervention for ovarian neoplasms. -

The Boundaries of the Region Are Margo Supraorbitalis, Linea Temporalis Superior, Linea Nuchae Superior Till Protuberantia Occipitalis Externa
Topographical anatomy & operative surgery of the head. Topographical pecularities of regions of the head and its practical importance. Main principles of surgical treatments The boundaries and divisions. The border between the head and a neck carried out (conditionally) to the inferior margin of mandible, angle of mandible, posterior margin of the vertical process of the mandible; the anterior and posterior edges of the mastoid process, superior nuchal line (linea nuchae superior), external occipital protuberance (protuberantia occipitalis externa). Then it passes symmetrically to the opposite side. On the head distinguish cerebral and facial departments, according to the cerebral and facial skull. The border between these departments passes by supraorbital margin, superior margin of the zygomatic arch to the porus acusticus externus. All that is down and anterior to this border belongs to the facial department, which is upward and backward, refers to the cerebral department. The cerebral department is divided into calvaria (fornix cranii) and bases of skull (basis cranii). The boundary between the base of scull and calvaria is mainly passes by the horizontal plane which joins the nasion to the inion (an imaginary line that passes along the supraorbital margin - margo supraorbitalis, superior margin of the zygomatic arch - arcus zigomaticus, base of the mastoid process - processus mastoideus, upper nuchal line - linea nuchae superior to inion). The parts of the skull located above this plane belong to the calvaria; located below - to the base of skull. Calvaria areas. 1) fronto-parietal-occipital region - regio frontoparietooccipitalis; 2) Temporal region - regio temporalis. Fronto-parieto-occipital region (regio fronto-parieto-occipitalis) The boundaries of the region are margo supraorbitalis, linea temporalis superior, linea nuchae superior till protuberantia occipitalis externa. -

A Patient with a Cavernous Sinus Dural Arteriovenous Fistula in Whom an Approach Through the Jugular Venous Arch Involving Facial Vein Return Was Adopted
Journal of Neuroendovascular Therapy Advance Published Date: September 30, 2020 DOI: 10.5797/jnet.cr.2020-0033 A Patient with a Cavernous Sinus Dural Arteriovenous Fistula in Whom an Approach through the Jugular Venous Arch Involving Facial Vein Return Was Adopted Takayuki Nagase, Koji Tokunaga, Kyoichi Watanabe, Tsuyoshi Umeda, Yasuki Suruga, Yuji Takasugi, Satoshi Inoue, Hideki Kiriyama, and Kengo Matsumoto Objective: We report the case of a cavernous sinus dural arteriovenous fistula (CSdAVF) treated by transvenous embolization (TVE) via the jugular venous arch (JVA) connecting bilateral superficial cervical veins. Case Presentation: A male patient in his 50s presenting with diplopia and headache was diagnosed with a CSdAVF. The first session of TVE resulted in incomplete obliteration of the fistula due to poor accessibility through the inferior petrosal sinus (IPS), and postoperative computed tomography angiography (CTA) disclosed a newly developed drainage route into the facial vein (FV) connecting to the anterior jugular vein (AJV) and the JVA. The patient underwent the second session of TVE through the JVA, FV, and the superior ophthalmic vein (SOV), and obliteration was achieved. Conclusion: There is a considerable variation in the anatomy of facio-cervical veins in patients with CSdAVF. Meticulous preoperative evaluation of the venous drainage route using modern diagnostic tools is indispensable to achieve successful results in patients with CSdAVF. Keywords▶ dural arteriovenous fistula, coil embolization, jugular venous arch