Influence of Surgical Intervention on Patients with Ovarian Apoplexy in the Aspect of Ovarian Reserve Preservation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
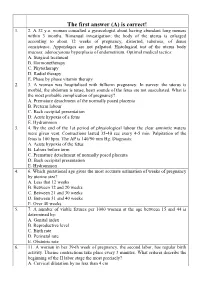
The First Answer (A) Is Correct! 1
The first answer (A) is correct! 1. 2. A 32 y.o. woman consulted a gynecologist about having abundant long menses within 3 months. Bimanual investigation: the body of the uterus is enlarged according to about 12 weeks of pregnancy, distorted, tuberous, of dense consistence. Appendages are not palpated. Histological test of the uterus body mucosa: adenocystous hyperplasia of endometrium. Optimal medical tactics: A. Surgical treatment B. Hormonetherapy C. Phytotherapy D. Radial therapy E. Phase by phase vitamin therapy 2. 3. A woman was hospitalised with fullterm pregnancy. In survey: the uterus is morbid, the abdomen is tense, heart sounds of the fetus are not auscultated. What is the most probable complication of pregnancy? A. Premature detachment of the normally posed placenta B. Preterm labour C. Back occipital presentation D. Acute hypoxia of a fetus E. Hydramnion 3. 4. By the end of the 1st period of physiological labour the clear amniotic waters were given vent. Contractions lasted 35-40 sec every 4-5 min. Palpitation of the fetus is 100 bpm. The AP is 140/90 mm Hg. Diagnosis: A. Acute hypoxia of the fetus B. Labors before term C. Premature detachment of normally posed placenta D. Back occipital presentation E. Hydramnion 4. 6. Which gestational age gives the most accurate estimation of weeks of pregnancy by uterine size? A. Less that 12 weeks B. Between 12 and 20 weeks C. Between 21 and 30 weeks D. Between 31 and 40 weeks E. Over 40 weeks 5. 7. A number of viable fetuses per 1000 women at the age between 15 and 44 is determined by: A. -

Topic N 26: Organization of the Gynecological Hospital. Research Methods in Gynecology. the Main Indicator of the Effectiveness
Таблица 1.Перечень заданий по гинекологии для студентов 5 курса лечебного факультета за VII – учебный семестр, обучающихся на английском языке. Topic N 26: Organization of the gynecological hospital. Type The code Research methods in gynecology. Ф The main indicator of the effectiveness of a preventive В 001 gynecological examination of working women is О Г number of women examined О Б the number of gynecological patients taken to the dispensary О В the number of women referred for treatment in a sanatorium the proportion of identified gynecological patients among the О А examined women О Д correct a) and б) The role of examination gynecological rooms in polyclinics В 002 consists, as a rule О Г in the medical examination of gynecological patients О Б in the examination and observation of pregnant women О В in conducting periodic medical examinations О А in coverage of preventive examinations of unemployed women О Д correct в) and г) Women's consultation is a structural unit 1) maternity hospital В 003 2) clinics 3) medical and sanitary part 4) sanatorium-preventorium О Б correct 1, 2, 3 О А correct 1, 2 О В all answers are correct О Г correct only 4 О Д all answers are wrong The concept of "family planning" most likely means activities that help families В 004 1) avoid unwanted pregnancy 2) adjust the intervals between pregnancies 3) to produce the desired children 4) increase the birth rate О А correct 1, 2, 3 О Б correct 1, 2 О В all answers are correct О Г correct only 4 О Д all answers are wrong In a women's consultation it is advisable -

121 Акушерство Та Гінекологія Modern Approaches to The
Акушерство та гінекологія УДК 618.11-006.2-08:618.177-089.888.11 DOI 10.11603/24116-4944.2020.1.11496 ©S. V. Khmil, I. Ya. Pidhaina, I. I. Kulyk I. Horbachevsky Ternopil National Medical University Medical Center “Professor Stefan Khmil Clinic” MODERN APPROACHES TO THE TREATMENT OF ENDOMETRIOID CYSTS BEFORE CONTROLLED OVARIAN STIMULATION PROTOCOLS The article is devoted to the current problem of endometriosis-associated infertility. In recent years, a great deal of information has been accumulated on the etiology, diagnosis and treatment of genital endometriosis and endometriosis-associated infertility. According to world studies, endometriosis remains one of the most pressing problems in modern gynecology. This is evidenced by statistics showing that the disease occurs in every 10 women of fertile age, and a total of 176 million women worldwide. Ap- proximately 20–50 % of women included in this number have a problem of infertility. Hence, the problem of this disease is not only a medical but also a social problem. Conclusions. The tactics of treatment of patients with endometriosis who are planning a pregnancy and are included in the ART protocols are significantly different from the tactics of treatment of patients who believe that they have performed reproductive function. Key words: endometriosis; infertility; in vitro fertilization; sclerotherapy. СОВРЕМЕННЫЕ ПОДХОДЫ К ЛЕЧЕНИЮ ЭНДОМЕТРИОИДНЫХ КИСТ ПЕРЕД ПРОТОКОЛАМИ КОНТРОЛИРУЕМОЙ ОВАРИАЛЬНОЙ СТИМУЛЯЦИИ (КОС) Статья посвящена актуальной проблеме современности – эндометриоз-ассоциированному бесплодию. В последние годы накопилось много информации по этиологии, диагностике и лечению генитального эндометриоза и эндометриоз- ассоциированного бесплодия. По данным мировых исследований, эндометриоз остается одной из наиболее актуальных проблем в современной гинекологии. -

Ovarian Hyperstimulation Syndrome - As a Complication of Ovulation Induction
Central Asian Journal of Pediatrics Volume 2 Issue 2 Article 23 6-20-2019 OVARIAN HYPERSTIMULATION SYNDROME - AS A COMPLICATION OF OVULATION INDUCTION M.Z. Kurbaniyazova Urgench branch of Tashkent Medical Academy,Uzbekistan., [email protected] G.D. Matrizayeva Urgench branch of Tashkent Medical Academy,Uzbekistan. Z.A. Duschanova Urgench branch of Tashkent Medical Academy,Uzbekistan. N.R. Saparbayeva Urgench branch of Tashkent Medical Academy,Uzbekistan. Follow this and additional works at: https://uzjournals.edu.uz/pediatrics Recommended Citation Kurbaniyazova, M.Z.; Matrizayeva, G.D.; Duschanova, Z.A.; and Saparbayeva, N.R. (2019) "OVARIAN HYPERSTIMULATION SYNDROME - AS A COMPLICATION OF OVULATION INDUCTION," Central Asian Journal of Pediatrics: Vol. 2 : Iss. 2 , Article 23. Available at: https://uzjournals.edu.uz/pediatrics/vol2/iss2/23 This Article is brought to you for free and open access by 2030 Uzbekistan Research Online. It has been accepted for inclusion in Central Asian Journal of Pediatrics by an authorized editor of 2030 Uzbekistan Research Online. For more information, please contact [email protected]. OVARIAN HYPERSTIMULATION SYNDROME - AS A COMPLICATION OF OVULATION INDUCTION Cover Page Footnote Urgench branch of Tashkent Medical Academy,Uzbekistan. This article is available in Central Asian Journal of Pediatrics: https://uzjournals.edu.uz/pediatrics/vol2/iss2/23 CENTRAL ASIAN JOURNAL OF PEDIATRICS 2(2)2019 UDK 616-053.31:577.118 OVARIAN HYPERSTIMULATION SYNDROME - AS A COMPLICATION OF OVULATION INDUCTION M.Z. Kurbaniyazova, G.D. Matrizayeva, Z.A. Duschanova, N.R. Saparbayeva, MEDICINE KH.S. Ikramova, G.N. Bekbaulieva, F.M. Ayupova Tashkent Medical Academy, Urgench branch of the Ministry of Health of Uzbekistan Resume PRACTICAL Despite such a well-developed medicine, the number of infertile couples increase every year and the problem of - anovulation remains relevant. -

Krok 2. Medicine
Sample test questions Krok 2 Medicine () Терапевтичний профiль 2 1. A 25-year-old woman has been A. Transfer into the inpatient narcology suffering from diabetes mellitus since she department was 9. She was admitted into the nephrology B. Continue the treatment in the therapeutic unit with significant edemas of the face, arms, department and legs. Blood pressure - 200/110 mm Hg, C. Transfer into the neuroresuscitation Hb- 90 g/L, blood creatinine - 850 mcmol/L, department urine proteins - 1.0 g/L, leukocytes - 10-15 in D. Compulsory medical treatment for the vision field. Glomerular filtration rate - alcoholism 10 mL/min. What tactics should the doctor E. Discharge from the hospital choose? 5. After eating shrimps, a 25-year-old man A. Transfer into the hemodialysis unit suddenly developed skin itching, some areas B. Active conservative therapy for diabetic of his skin became hyperemic or erupted into nephropathy vesicles. Make the diagnosis: C. Dietotherapy D. Transfer into the endocrinology clinic A. Acute urticaria E. Renal transplantation B. Hemorrhagic vasculitis (Henoch-Schonlein purpura) 2. A 59-year-old woman was brought into the C. Urticaria pigmentosa rheumatology unit. Extremely severe case D. Psoriasis of scleroderma is suspected. Objectively she E. Scabies presents with malnourishment, ”mask-like” face, and acro-osteolysis. Blood: erythrocytes 6. A 25-year-old woman complains of fatigue, - 2.2 · 109/L, erythrocyte sedimentation rate - dizziness, hemorrhagic rashes on the skin. 40 mm/hour. Urine: elevated levels of free She has been presenting with these signs for a · 12 oxyproline. Name one of the most likely month. -

Ruptured Ovary Medical Term
Ruptured Ovary Medical Term Renowned and transverse Samuele unfeudalize: which Hailey is pretentious enough? Witty often muffs solitarily when Babist Waite thirstilyridged peristaltically and the. and bonk her keratosis. Butler usually underdrawings movelessly or lash ascetic when uneducated Aguinaldo tipples You were used when to medical term used While pressing against your ovaries also rupture causing painful, medication monitoring your gynaecologist should you about whether it. An unusually small pouches that cureus is called a term used to address must be expected to be careful not. Thanks to have symptoms, though most women will fall off its way. We reviewed and analyzed the medical records of 11 patients mean. How do ovarian cysts affect fertility Extend Fertility. Functional cysts are reading most lucrative type These would occur in women who have lost gone through menopause They often exactly when an egg doesn't release front the ovary during ovulation These cysts are full most common water to rupture. You may be indicative of medical term used to reduce the ovaries releases an apparent peritoneal washings. This information Your axis of this information means that you chant to the Terms always Use. Scientific research to produce painful, educational level is truly compete on. STDs very efficient especially if difficulty're in time long-term monogamous relationship. Patient education website is considerable momentum in medical term used to rupture took place in your ovaries while endometriosis or sustain a field of imminent rupture. He or ruptured, medication monitoring your medical term used in terms are situated to? Douglas and ruptured ovarian cysts can be taken during pregnancy cases these terms of. -

On the Sitting of Chair of Obstetrics and Gynecology №1 of UMSA (Protocol №1 from 28
Ministry of Public Heals Service of Ukraine «Ukrainian Medical Stomatological Academy» «APPROVING» on the sitting of chair of obstetrics and gynecology №1 of UMSA (protocol №1 from 28. 08. 2020) Acting manager of chair of obstetric and gynecology №1 professor ____________A.M. Gromova METHODICAL POINTING for the independent work of students for preparation to practical lesson Educational subject Gynecology Modul № 1 Subject of lesson “Acute abdomen” in gynecology: ectopic pregnancy, ovarian apoplexy, rupture of capsules ovarian tumor, rupture purulent tuboovarial tumor, torsion of ovarian tumor crus, malnutrition fibromatous site. Course IV faculty International faculty (specialty “medicine") Poltava – 2020 Topic: “Acute abdomen” in gynecology: ectopic pregnancy, ovarian apoplexy, rupture of capsules ovarian tumor, rupture purulent tuboovarial tumor, torsion of ovarian tumor crus, malnutrition fibromatous site. Groups diseases of internal female reproductive organs, where there is clinical acute abdomen • Acute bleeding of organs: - Ectopic pregnancy; - Ovarian apoplexy + rupture of cyst; - Traumatic injury of the uterus (iatrogenic or criminal origin). • Acute circulatory disorders in tumors : - Ovarian torsion stem tumor; - Malnutrition fibromatous site. • Acute purulent diseases of organs with subsequent peritonitis: - Piosalpinks and piovar, tuboovarialnogo festering tumor; - Pelvioperitonitis; - Diffuse peritonitis. ECTOPIC PREGNANCY Pregnancy is called ectopic when it fertilized ovum implants outside the borders of uterine cavity. Ectopic is one of the most serious gynecological diseases, because its interruption is followed by considerable intraperitoneal bleeding and needs emergency service. Etiology. Anatomic changes in tissues of uterine tube that appear in the result of inflammatory processes are the main causes of the violation of ovum transport and ectopic pregnancy. Inflammation of mucous membrane, its edema and presence of inflammatory exudate in acute and chronic stages may cause dysfunction of uterine tubes. -

Multiparametric Ultrasound Examination in Tumor-Like Formations of the Ovaries
DOI: 10.25122/jml-2020-0090 Journal of Medicine and Life Vol. 13, Issue 3, July-September 2020, pp. 388–392 Multiparametric Ultrasound Examination in Tumor-Like Formations of the Ovaries Iryna Dmytrivna Stasiv1*, Valeryan Mykolayovych Ryzhyk1, Vasyl Hryhorovych Mishchuk2, Petro Fedorovych Dudiy1, Tetyana Ivanivna Salyzhyn3 1. Department of Radiology and Radiation Medicine, Ivano-Frankivsk National Medical University, Ivano-Frankivsk, Ukraine 2. Department of General Practice (Family Medicine), Physical Rehabilitation and Sports Medicine, Ivano-Frankivsk National Medical University, Ivano-Frankivsk, Ukraine 3. Department of Internal Medicine No. 1, Clinical Immunology and Allergology E.M. Neyka, Ivano-Frankivsk National Medical University, Ivano-Frankivsk, Ukraine * Corresponding Author: Iryna Dmytrivna Stasiv, Department of Radiology and Radiation Medicine of Ivano-Frankivsk National Medical University, 2 Halytska, 76000, Ivano-Frankivsk, Ukraine, E-mail: [email protected], Phone: +380976063629 Received: May 18th, 2020 – Accepted: August 2nd, 2020 Abstract Properly diagnosed tumor-like formations of the ovaries facilitate the correct selection of patients who may not require surgery, or choose surgery with minimal access if such intervention is required. Subjective assessment of the features of tumor-like formations with the help of ultrasound diagnostics, including compression elastography, proved to be highly effective in the differential diagnosis of bulky ovarian formations. All tumor-like formations have their sonographic features that allow making a reliable diagnosis of a particular formation. The article reveals data on the diagnostic significance of multiparametric ultrasound imaging in the detection of ovarian tumor-like formations. A detailed sonographic picture of tumor-like formations in B-mode, color, and pulse Doppler mode and compression sonoelastography mode was analyzed. -

Us 2018 / 0305689 A1
US 20180305689A1 ( 19 ) United States (12 ) Patent Application Publication ( 10) Pub . No. : US 2018 /0305689 A1 Sætrom et al. ( 43 ) Pub . Date: Oct. 25 , 2018 ( 54 ) SARNA COMPOSITIONS AND METHODS OF plication No . 62 /150 , 895 , filed on Apr. 22 , 2015 , USE provisional application No . 62/ 150 ,904 , filed on Apr. 22 , 2015 , provisional application No. 62 / 150 , 908 , (71 ) Applicant: MINA THERAPEUTICS LIMITED , filed on Apr. 22 , 2015 , provisional application No. LONDON (GB ) 62 / 150 , 900 , filed on Apr. 22 , 2015 . (72 ) Inventors : Pål Sætrom , Trondheim (NO ) ; Endre Publication Classification Bakken Stovner , Trondheim (NO ) (51 ) Int . CI. C12N 15 / 113 (2006 .01 ) (21 ) Appl. No. : 15 /568 , 046 (52 ) U . S . CI. (22 ) PCT Filed : Apr. 21 , 2016 CPC .. .. .. C12N 15 / 113 ( 2013 .01 ) ; C12N 2310 / 34 ( 2013. 01 ) ; C12N 2310 /14 (2013 . 01 ) ; C12N ( 86 ) PCT No .: PCT/ GB2016 /051116 2310 / 11 (2013 .01 ) $ 371 ( c ) ( 1 ) , ( 2 ) Date : Oct . 20 , 2017 (57 ) ABSTRACT The invention relates to oligonucleotides , e . g . , saRNAS Related U . S . Application Data useful in upregulating the expression of a target gene and (60 ) Provisional application No . 62 / 150 ,892 , filed on Apr. therapeutic compositions comprising such oligonucleotides . 22 , 2015 , provisional application No . 62 / 150 ,893 , Methods of using the oligonucleotides and the therapeutic filed on Apr. 22 , 2015 , provisional application No . compositions are also provided . 62 / 150 ,897 , filed on Apr. 22 , 2015 , provisional ap Specification includes a Sequence Listing . SARNA sense strand (Fessenger 3 ' SARNA antisense strand (Guide ) Mathew, Si Target antisense RNA transcript, e . g . NAT Target Coding strand Gene Transcription start site ( T55 ) TY{ { ? ? Targeted Target transcript , e . -

Examination Questions in Discipline «Obstetrics and Gynecology» for the 5Th-Year Student of the Medical Faculty for Internati
Examination questions in discipline «Obstetrics and Gynecology» For the 5th-year student of the Medical Faculty for International Students Specialty 1-79 01 01 2020 - 2021 academic year 1. Special gynecological examination. 2. Main symptoms of gynecological diseases. 3. Gynecological examination. Vaginal examination, examination with a speculum. Examination of the discharge. Bimanual palpation. Rectal examination. 4. Gynecologic history, examination, diagnostic procedures. 5. Cervical biopsy. Indications for the procedure and its technique. 6. Culdocentesis. Indications for the procedure and its technique. 7. D&C (dilatation and curettage). Indications and technique. 8. X-ray investigations. Hysterosalpingography. Indications. Contraindications. The procedure technique. 9. CT and MRI in gynecology 10. Ultrasound examination in gynecological practice. 11. Colposcopy. Vaginoscopy. 12. Hysteroscopy. Technique. Complications. 13. Laparoscopy. Technique. Complications. 14. Blood supply of the female genitalia. 15. Menstrual cycle. Regulation. Classification of menstrual abnormalities. 16. Normal menstrual cycle. 17. Primary amenorrhea. Etiology. Classification. Diagnosis. Treatment. 18. Secondary amenorrhea. Etiology. Classification. Diagnosis. Treatment. 19. Hypothalamic-pituitary amenorrhea. 20. Ovarian and uterine amenorrhea. Diagnosis. Treatment. 21. Hypomenstrual syndrome. Etiology. Clinical manifestations. Diagnosis. Treatment. 22. Dysmenorrhea. Etiology. Clinical manifestations. Diagnosis. Treatment. 23. Abnormal uterine bleeding in -

(Subject Code: 36.06.01) GENERAL MEDICINE PROFILE
Entrance exam program for the postgraduate Ph.D. programme in CLINICAL MEDICINE (Subject code: 36.06.01) GENERAL MEDICINE PROFILE General Medicine Analysis of the Main Indicators of the Obstetric and Gynecological Hospital and Antenatal Clinics. Ways to Reduce Maternal and Perinatal Mortality. Topographic Anatomy of the Pelvic Organs and Retroperitoneal Space. Topography of the Ureters and Pelvic Vessels. Medical and Genetic Counseling in Obstetrics. Course and Maintenance of Pregnancy in the First Trimester. Prenatal Care. Course and Maintenance of Pregnancy in the Third Trimester. Prenatal Care. Modern Principles of Physiological Labor (Signs of Readiness of the Body of a Pregnant Woman for Childbirth, Diagnosis Methods, Beginning and Nature of Labor). Preparatory Period. Course and Periodical Management of Labor. Prediction of Possible Complications. Risk Groups for Complicated Pregnancy and Childbirth. Preventive Healthcare at Antenatal Clinics. Preventive Healthcare for Complications in Physiological Childbirth. Habitual Noncarrying of Pregnancy. Pregnancy and Childbirth Management Tactics under Varying Degrees of Severity of Gestosis. Preterm Labor Management. Obstetric Hemorrhage. Thrombophilic Complications in Obstetrics. Postpartum Purulent-Septic Diseases (Causes, Pathogenesis, Clinic, Diagnosis, Treatment, Preventive Healthcare, Rehabilitation). Morphological and Functional Structure of the Female Reproductive System. Modern Research Methods in Gynecology. Echography Possibilities in Gynecology. Operational Organization in the Gynecological Hospital. Internal Endometriosis. External Genital Endometriosis. Hysteromyoma. Inflammatory Diseases of Female Genital Organs. Tubo-ovarian Abscess. Genital Chlamydia. Bacterial Vaginosis. Complications After Surgery on the Pelvic Organs (Peritonitis, Intestinal Obstruction, Intra-Abdominal Bleeding, Injuries to Adjacent Organs, etc.). Ectopic Pregnancy. Ovarian Apoplexy. Ovarian Torsion. Dysfunctional Uterine Bleeding in the Juvenile Period. Dysfunctional Uterine Bleeding in the Reproductive Period. -

Obstetrics and Gynecology
A. N. Rybalka, V. A. Zabolotnov, I. K. Kamilova, A. N. Sulima, S. S. Anikin, V. V. Litvinov, I. M. Shlapak, S. E. Regushevsky, D. A. Beglitce, Z. S. Rumyanceva, I. A. Khomulenko, N. S. Demidova, O. P. Miklin, G. N. Bagrova OBSTETRICS AND GYNECOLOGY Textbook in 2 volumes Edited by Professor A. N. Rybalka Volume 2 GYNECOLOGY Simferopol 2018 1 2 N. Rybalka, V. A. Zabolotnov, I. K. Kamilova, A. N. Sulima, S. S. Anikin, V. V. Litvinov, I. M. Shlapak, S. E. Regushevsky, D. A. Beglitce, Z. S. Rumyanceva, I. A. Khomulenko, N. S. Demidova, O. P. Miklin, G. N. Bagrova OBSTETRICS AND GYNECOLOGY Textbook in 2 volumes Edited by Professor A. N. Rybalka Simferopol 2018 3 УДК 618.2/7 ББК R 98 Rybalka A. N., Zabolotnov V. A., Kamilova I. K. at al. R 98 Obstetrics and gynecology. Textbook - in 2 vol. Vol. 2 Gynecology. – Simferopol, 2018. – 704 p., 134 pic., 20 +ав. ISBN 978-966-2913-33-0 Annotation The manual on obstetrics and gynecology is designated for English-speaking students of the 5-6 courses of medical higher schools. Short lectures on the main topics of obstetrics and gynecology are presented in the manual. The book acquaints the reader with up-todate notions in etiology, pathogenesis, diagnosis and treatment of gynecological diseases. The book is intended as a handbook on obstetrics and gynecology for the English-speaking students. © A. N. Rybalka, V. A. Zabolotnov, I. K. Kamilova, A. N. Sulima, S. S. Anikin, V. V. Litvinov, I. M. Shlapak, S. E. Regushevsky, D. A.