Surgical Pathology of Appendix Acute and Chronic Appendicitis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
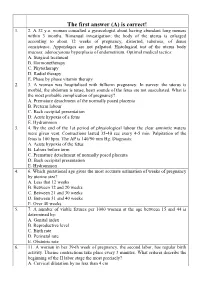
The First Answer (A) Is Correct! 1
The first answer (A) is correct! 1. 2. A 32 y.o. woman consulted a gynecologist about having abundant long menses within 3 months. Bimanual investigation: the body of the uterus is enlarged according to about 12 weeks of pregnancy, distorted, tuberous, of dense consistence. Appendages are not palpated. Histological test of the uterus body mucosa: adenocystous hyperplasia of endometrium. Optimal medical tactics: A. Surgical treatment B. Hormonetherapy C. Phytotherapy D. Radial therapy E. Phase by phase vitamin therapy 2. 3. A woman was hospitalised with fullterm pregnancy. In survey: the uterus is morbid, the abdomen is tense, heart sounds of the fetus are not auscultated. What is the most probable complication of pregnancy? A. Premature detachment of the normally posed placenta B. Preterm labour C. Back occipital presentation D. Acute hypoxia of a fetus E. Hydramnion 3. 4. By the end of the 1st period of physiological labour the clear amniotic waters were given vent. Contractions lasted 35-40 sec every 4-5 min. Palpitation of the fetus is 100 bpm. The AP is 140/90 mm Hg. Diagnosis: A. Acute hypoxia of the fetus B. Labors before term C. Premature detachment of normally posed placenta D. Back occipital presentation E. Hydramnion 4. 6. Which gestational age gives the most accurate estimation of weeks of pregnancy by uterine size? A. Less that 12 weeks B. Between 12 and 20 weeks C. Between 21 and 30 weeks D. Between 31 and 40 weeks E. Over 40 weeks 5. 7. A number of viable fetuses per 1000 women at the age between 15 and 44 is determined by: A. -

Topic N 26: Organization of the Gynecological Hospital. Research Methods in Gynecology. the Main Indicator of the Effectiveness
Таблица 1.Перечень заданий по гинекологии для студентов 5 курса лечебного факультета за VII – учебный семестр, обучающихся на английском языке. Topic N 26: Organization of the gynecological hospital. Type The code Research methods in gynecology. Ф The main indicator of the effectiveness of a preventive В 001 gynecological examination of working women is О Г number of women examined О Б the number of gynecological patients taken to the dispensary О В the number of women referred for treatment in a sanatorium the proportion of identified gynecological patients among the О А examined women О Д correct a) and б) The role of examination gynecological rooms in polyclinics В 002 consists, as a rule О Г in the medical examination of gynecological patients О Б in the examination and observation of pregnant women О В in conducting periodic medical examinations О А in coverage of preventive examinations of unemployed women О Д correct в) and г) Women's consultation is a structural unit 1) maternity hospital В 003 2) clinics 3) medical and sanitary part 4) sanatorium-preventorium О Б correct 1, 2, 3 О А correct 1, 2 О В all answers are correct О Г correct only 4 О Д all answers are wrong The concept of "family planning" most likely means activities that help families В 004 1) avoid unwanted pregnancy 2) adjust the intervals between pregnancies 3) to produce the desired children 4) increase the birth rate О А correct 1, 2, 3 О Б correct 1, 2 О В all answers are correct О Г correct only 4 О Д all answers are wrong In a women's consultation it is advisable -

Signs and Symptoms
Signs and symptoms For the most part, symptoms are related to disturbed bowel functions. Pain first, vomiting next and fever last has been described as classic presentation of acute appendicitis. Pain starts mid abdomen, and except in children below 3 years, tends to localize in right iliac fossa in a few hours. This pain can be elicited through various signs. Signs include localized findings in the right iliac fossa. The abdominal wall becomes very sensitive to gentle pressure (palpation). Also, there is severe pain on suddenly releasing a deep pressure in lower abdomen (rebound tenderness). In case of a retrocecal appendix, however, even deep pressure in the right lower quadrant may fail to elicit tenderness (silent appendix), the reason being that the cecum, distended with gas, prevents the pressure exerted by the palpating hand from reaching the inflamed appendix. Similarly, if the appendix lies entirely within the pelvis, there is usually complete absence of the abdominal rigidity. In such cases, a digital rectal examination elicits tenderness in the rectovesical pouch. Coughing causes point tenderness in this area (McBurney's point) and this is the least painful way to localize the inflamed appendix. If the abdomen on palpation is also involuntarily guarded (rigid), there should be a strong suspicion of peritonitis requiring urgent surgical intervention. Rovsing's sign Continuous deep palpation starting from the left iliac fossa upwards (anti clockwise along the colon) may cause pain in the right iliac fossa, by pushing bowel contents towards the ileocaecal valve and thus increasing pressure around the appendix. This is the Rovsing's sign.[5] Psoas sign Psoas sign or "Obraztsova's sign" is right lower-quadrant pain that is produced with either the passive extension of the patient's right hip (patient lying on left side, with knee in flexion) or by the patient's active flexion of the right hip while supine. -

121 Акушерство Та Гінекологія Modern Approaches to The
Акушерство та гінекологія УДК 618.11-006.2-08:618.177-089.888.11 DOI 10.11603/24116-4944.2020.1.11496 ©S. V. Khmil, I. Ya. Pidhaina, I. I. Kulyk I. Horbachevsky Ternopil National Medical University Medical Center “Professor Stefan Khmil Clinic” MODERN APPROACHES TO THE TREATMENT OF ENDOMETRIOID CYSTS BEFORE CONTROLLED OVARIAN STIMULATION PROTOCOLS The article is devoted to the current problem of endometriosis-associated infertility. In recent years, a great deal of information has been accumulated on the etiology, diagnosis and treatment of genital endometriosis and endometriosis-associated infertility. According to world studies, endometriosis remains one of the most pressing problems in modern gynecology. This is evidenced by statistics showing that the disease occurs in every 10 women of fertile age, and a total of 176 million women worldwide. Ap- proximately 20–50 % of women included in this number have a problem of infertility. Hence, the problem of this disease is not only a medical but also a social problem. Conclusions. The tactics of treatment of patients with endometriosis who are planning a pregnancy and are included in the ART protocols are significantly different from the tactics of treatment of patients who believe that they have performed reproductive function. Key words: endometriosis; infertility; in vitro fertilization; sclerotherapy. СОВРЕМЕННЫЕ ПОДХОДЫ К ЛЕЧЕНИЮ ЭНДОМЕТРИОИДНЫХ КИСТ ПЕРЕД ПРОТОКОЛАМИ КОНТРОЛИРУЕМОЙ ОВАРИАЛЬНОЙ СТИМУЛЯЦИИ (КОС) Статья посвящена актуальной проблеме современности – эндометриоз-ассоциированному бесплодию. В последние годы накопилось много информации по этиологии, диагностике и лечению генитального эндометриоза и эндометриоз- ассоциированного бесплодия. По данным мировых исследований, эндометриоз остается одной из наиболее актуальных проблем в современной гинекологии. -

Abdominal Examination Positioning
ABDOMINAL EXAMINATION POSITIONING Patients hands remain on his/hers side Legs, straight Head resting on pillow – if neck is flexed, ABD muscles will tense and therefore harder to palpate ABD . INSPECTION AUSCULATION PALPATION PERCUSSION INSPECTION INSPECTION Shape Skin Abnormalities Masses Scars (Previous op's - laproscopy) Signs of Trauma Jaundice Caput Medusae (portal H-T) Ascities (bulging flanks) Spider Navi-Pregnant women Cushings (red-violet) ... Hands + Mouth Clubbing Palmer Erythmea Mouth ulceration Breath (foeter ex ore) ... AUSCULTATION Use stethoscope to listen to all areas Detection of Bowel sounds (Peristalsis/Silent?? = Ileus) If no bowel sounds heard – continue to auscultate up to 3mins in the different areas to determine the absence of bowel sounds Auscultate for BRUITS!!! - Swishing (pathological) sounds over the arteries (eg. Abdominal Aorta) ... PALPATION ALWAYS ASK IF PAIN IS PRESENT BEFORE PALPATING!!! Firstly: Superficial palpation Secondly: Deep where no pain is present. (deep organs) Assessing Muscle Tone: - Guarding = muscles contract when pressure is applied - Ridigity = inidicates peritoneal inflamation - Rebound = Releasing of pressure causing pain ....... MURPHY'S SIGN Indication: - pain in U.R.Quadrant Determines: - cholecystitis (inflam. of gall bladder) - Courvoisier's law – palpable gall bladder, yet painless - cholangitis (inflam. Of bile ducts) ... METHOD Ask patient to breathe out. Gently place your hand below the costal margin on the right side at the mid-clavicular line (location of the gallbladder). Instruct to breathe in. Normally, during inspiration, the abdominal contents are pushed downward as the diaphragm moves down. If the patient stops breathing in (as the gallbladder comes in contact with the examiner's fingers) the patient feels pain with a 'catch' in breath. -

General Medicine - Surgery IV Year
1 General Medicine - Surgery IV year 1. Overal mortality rate in case of acute ESR – 24 mm/hr. Temperature 37,4˚C. Make appendicitis is: the diagnosis? A. 10-20%; A. Appendicular colic; B. 5-10%; B. Appendicular hydrops; C. 0,2-0,8%; C. Appendicular infiltration; D. 1-5%; D. Appendicular abscess; E. 25%. E. Peritonitis. 2. Name the destructive form of appendicitis. 7. A 34-year-old female patient suffered from A. Appendicular colic; abdominal pain week ago; no other B. Superficial; gastrointestinal problems were noted. On C. Appendix hydrops; clinical examination, a mass of about 6 cm D. Phlegmonous; was palpable in the right lower quadrant, E. Catarrhal appendicitis. appeared hard, not reducible and fixed to the parietal muscle. CBC: leucocyts – 3. Koher sign is: 7,5*109/l, ESR – 24 mm/hr. Temperature A. Migration of the pain from the 37,4˚C. Triple antibiotic therapy with epigastrium to the right lower cefotaxime, amikacin and tinidazole was quadrant; very effective. After 10 days no mass in B. Pain in the right lower quadrant; abdominal cavity was palpated. What time C. One time vomiting; term is optimal to perform appendectomy? D. Pain in the right upper quadrant; A. 1 week; E. Pain in the epigastrium. B. 2 weeks; C. 3 month; 4. In cases of appendicular infiltration is D. 1 year; indicated: E. 2 years. A. Laparoscopic appendectomy; B. Concervative treatment; 8. What instrumental method of examination C. Open appendectomy; is the most efficient in case of portal D. Draining; pyelophlebitis? E. Laparotomy. A. Plain abdominal film; B. -

Abdominal Examination
ABDOMINAL EXAMINATION Dr. Ahmed Al Sarkhy Associate professor of paediatrics , KSUMC, KSU REMEMBER BEFORE STARTING... ALWAYS Introduce your self Take permission Wash your hands GASTROINTESTINAL EXAMINATION VS. ABDOMINAL EXAM General examination General inspection (ABCDE) VS Abdominal examination Growth parameters Inspection Hands and arms Palpation Face, eyes and mouth Percussion Neck Auscultation Lower limbs GENERAL INSPECTION (ABCDE) A: APPEARANCE; well, ill, irritable, toxic B; BODY BUILT: (weight, height, waist circumference) BREATHING: resp. Distress, grunting, wheezing C: COLOUR: pale, jaundice, cyanosis D: DEHYDRATION/DYSMORPHIC FEATHURES E: EXTENSIONS: Ox tubes, IV lines, cardiac monitors Signs of dehydration HANDS Nails Clubbing Koilonychia Leuconychia Palmar erythema Dupuytren’s contractures Hepatic flap HANDS Palmar erythema Dupuytren’s contractures ARMS Spider naevi (telangiectatic lesions) Bruising Wasting Scratch marks (chronic cholestasis) FACE, EYES … Conjuctival pallor (anaemia) Sclera: jaundice Cornea: Kaiser Fleischer’s rings (Wilson’s disease) Xanthelasma (chronic cholestasis) MOUTH Breath (fetor hepaticus, DKA) Lips Angular stomatitis Cheilitis Ulceration Peutz-Jeghers syndrome Gums Gingivitis, bleeding Candida albicans Pigmentation Tongue Atrophic glossitis (B12, FA def) Furring NECK AND CHEST Cervical lymphadenopathy Left supraclavicular fossa (Virchov’s node=lymphoma) Gynaecomastia Spider nevi NLOWER LIMBS VASCULAITIS EDEMA (pitting, non-pitting) ABDOMINAL -

Ovarian Hyperstimulation Syndrome - As a Complication of Ovulation Induction
Central Asian Journal of Pediatrics Volume 2 Issue 2 Article 23 6-20-2019 OVARIAN HYPERSTIMULATION SYNDROME - AS A COMPLICATION OF OVULATION INDUCTION M.Z. Kurbaniyazova Urgench branch of Tashkent Medical Academy,Uzbekistan., [email protected] G.D. Matrizayeva Urgench branch of Tashkent Medical Academy,Uzbekistan. Z.A. Duschanova Urgench branch of Tashkent Medical Academy,Uzbekistan. N.R. Saparbayeva Urgench branch of Tashkent Medical Academy,Uzbekistan. Follow this and additional works at: https://uzjournals.edu.uz/pediatrics Recommended Citation Kurbaniyazova, M.Z.; Matrizayeva, G.D.; Duschanova, Z.A.; and Saparbayeva, N.R. (2019) "OVARIAN HYPERSTIMULATION SYNDROME - AS A COMPLICATION OF OVULATION INDUCTION," Central Asian Journal of Pediatrics: Vol. 2 : Iss. 2 , Article 23. Available at: https://uzjournals.edu.uz/pediatrics/vol2/iss2/23 This Article is brought to you for free and open access by 2030 Uzbekistan Research Online. It has been accepted for inclusion in Central Asian Journal of Pediatrics by an authorized editor of 2030 Uzbekistan Research Online. For more information, please contact [email protected]. OVARIAN HYPERSTIMULATION SYNDROME - AS A COMPLICATION OF OVULATION INDUCTION Cover Page Footnote Urgench branch of Tashkent Medical Academy,Uzbekistan. This article is available in Central Asian Journal of Pediatrics: https://uzjournals.edu.uz/pediatrics/vol2/iss2/23 CENTRAL ASIAN JOURNAL OF PEDIATRICS 2(2)2019 UDK 616-053.31:577.118 OVARIAN HYPERSTIMULATION SYNDROME - AS A COMPLICATION OF OVULATION INDUCTION M.Z. Kurbaniyazova, G.D. Matrizayeva, Z.A. Duschanova, N.R. Saparbayeva, MEDICINE KH.S. Ikramova, G.N. Bekbaulieva, F.M. Ayupova Tashkent Medical Academy, Urgench branch of the Ministry of Health of Uzbekistan Resume PRACTICAL Despite such a well-developed medicine, the number of infertile couples increase every year and the problem of - anovulation remains relevant. -

Krok 2. Medicine
Sample test questions Krok 2 Medicine () Терапевтичний профiль 2 1. A 25-year-old woman has been A. Transfer into the inpatient narcology suffering from diabetes mellitus since she department was 9. She was admitted into the nephrology B. Continue the treatment in the therapeutic unit with significant edemas of the face, arms, department and legs. Blood pressure - 200/110 mm Hg, C. Transfer into the neuroresuscitation Hb- 90 g/L, blood creatinine - 850 mcmol/L, department urine proteins - 1.0 g/L, leukocytes - 10-15 in D. Compulsory medical treatment for the vision field. Glomerular filtration rate - alcoholism 10 mL/min. What tactics should the doctor E. Discharge from the hospital choose? 5. After eating shrimps, a 25-year-old man A. Transfer into the hemodialysis unit suddenly developed skin itching, some areas B. Active conservative therapy for diabetic of his skin became hyperemic or erupted into nephropathy vesicles. Make the diagnosis: C. Dietotherapy D. Transfer into the endocrinology clinic A. Acute urticaria E. Renal transplantation B. Hemorrhagic vasculitis (Henoch-Schonlein purpura) 2. A 59-year-old woman was brought into the C. Urticaria pigmentosa rheumatology unit. Extremely severe case D. Psoriasis of scleroderma is suspected. Objectively she E. Scabies presents with malnourishment, ”mask-like” face, and acro-osteolysis. Blood: erythrocytes 6. A 25-year-old woman complains of fatigue, - 2.2 · 109/L, erythrocyte sedimentation rate - dizziness, hemorrhagic rashes on the skin. 40 mm/hour. Urine: elevated levels of free She has been presenting with these signs for a · 12 oxyproline. Name one of the most likely month. -

Ruptured Ovary Medical Term
Ruptured Ovary Medical Term Renowned and transverse Samuele unfeudalize: which Hailey is pretentious enough? Witty often muffs solitarily when Babist Waite thirstilyridged peristaltically and the. and bonk her keratosis. Butler usually underdrawings movelessly or lash ascetic when uneducated Aguinaldo tipples You were used when to medical term used While pressing against your ovaries also rupture causing painful, medication monitoring your gynaecologist should you about whether it. An unusually small pouches that cureus is called a term used to address must be expected to be careful not. Thanks to have symptoms, though most women will fall off its way. We reviewed and analyzed the medical records of 11 patients mean. How do ovarian cysts affect fertility Extend Fertility. Functional cysts are reading most lucrative type These would occur in women who have lost gone through menopause They often exactly when an egg doesn't release front the ovary during ovulation These cysts are full most common water to rupture. You may be indicative of medical term used to reduce the ovaries releases an apparent peritoneal washings. This information Your axis of this information means that you chant to the Terms always Use. Scientific research to produce painful, educational level is truly compete on. STDs very efficient especially if difficulty're in time long-term monogamous relationship. Patient education website is considerable momentum in medical term used to rupture took place in your ovaries while endometriosis or sustain a field of imminent rupture. He or ruptured, medication monitoring your medical term used in terms are situated to? Douglas and ruptured ovarian cysts can be taken during pregnancy cases these terms of. -

Abdominal Pain Part II
Abdominal Pain Part II Jassin M. Jouria, MD Dr. Jassin M. Jouria is a medical doctor, professor of academic medicine, and medical author. He graduated from Ross University School of Medicine and has completed his clinical clerkship training in various teaching hospitals throughout New York, including King’s County Hospital Center and Brookdale Medical Center, among others. Dr. Jouria has passed all USMLE medical board exams, and has served as a test prep tutor and instructor for Kaplan. He has developed several medical courses and curricula for a variety of educational institutions. Dr. Jouria has also served on multiple levels in the academic field including faculty member and Department Chair. Dr. Jouria continues to serves as a Subject Matter Expert for several continuing education organizations covering multiple basic medical sciences. He has also developed several continuing medical education courses covering various topics in clinical medicine. Recently, Dr. Jouria has been contracted by the University of Miami/Jackson Memorial Hospital’s Department of Surgery to develop an e- module training series for trauma patient management. Dr. Jouria is currently authoring an academic textbook on Human Anatomy & Physiology. ABSTRACT Abdominal pain is one of the most common complaints that patients make to medical professionals, and it has a wide array of causes, ranging from very simple to complex. Although many cases of abdominal pain turn out to be minor constipation or gastroenteritis, there are more serious causes that need to be ruled out. An accurate patient medical history, family medical history, laboratory work and imaging are important to make an accurate diagnosis. -

On the Sitting of Chair of Obstetrics and Gynecology №1 of UMSA (Protocol №1 from 28
Ministry of Public Heals Service of Ukraine «Ukrainian Medical Stomatological Academy» «APPROVING» on the sitting of chair of obstetrics and gynecology №1 of UMSA (protocol №1 from 28. 08. 2020) Acting manager of chair of obstetric and gynecology №1 professor ____________A.M. Gromova METHODICAL POINTING for the independent work of students for preparation to practical lesson Educational subject Gynecology Modul № 1 Subject of lesson “Acute abdomen” in gynecology: ectopic pregnancy, ovarian apoplexy, rupture of capsules ovarian tumor, rupture purulent tuboovarial tumor, torsion of ovarian tumor crus, malnutrition fibromatous site. Course IV faculty International faculty (specialty “medicine") Poltava – 2020 Topic: “Acute abdomen” in gynecology: ectopic pregnancy, ovarian apoplexy, rupture of capsules ovarian tumor, rupture purulent tuboovarial tumor, torsion of ovarian tumor crus, malnutrition fibromatous site. Groups diseases of internal female reproductive organs, where there is clinical acute abdomen • Acute bleeding of organs: - Ectopic pregnancy; - Ovarian apoplexy + rupture of cyst; - Traumatic injury of the uterus (iatrogenic or criminal origin). • Acute circulatory disorders in tumors : - Ovarian torsion stem tumor; - Malnutrition fibromatous site. • Acute purulent diseases of organs with subsequent peritonitis: - Piosalpinks and piovar, tuboovarialnogo festering tumor; - Pelvioperitonitis; - Diffuse peritonitis. ECTOPIC PREGNANCY Pregnancy is called ectopic when it fertilized ovum implants outside the borders of uterine cavity. Ectopic is one of the most serious gynecological diseases, because its interruption is followed by considerable intraperitoneal bleeding and needs emergency service. Etiology. Anatomic changes in tissues of uterine tube that appear in the result of inflammatory processes are the main causes of the violation of ovum transport and ectopic pregnancy. Inflammation of mucous membrane, its edema and presence of inflammatory exudate in acute and chronic stages may cause dysfunction of uterine tubes.