Morriston ED
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Candidate Information Pack
Candidate Information Contents Section 1 – Welcome and Foreword 3 Section 2 – The NHS in Wales 5 Section 3 – Purpose, vision, aims and values 7 Section 4 – How we are structured and overview of services 9 Section 5 – Strategic change, challenges and planning 14 Section 6 – Working in partnership with Universities 18 Section 7 – A very special and unique place to live and work 25 Chairman’s Foreword Dear Candidate ABMU Health Board is ambitious - we aim to create a new model of a 21st century health economy, based on our core values of Caring for Each Other, Working Together and Always Improving. We want an Executive Director who shares our values and has ambition, drive and determination to help us create that. In Wales, NHS policy is the responsibility of the Welsh Government and health policy has diverged significantly from that operating in England where a market-driven system, increasingly based on competition, has developed. In Wales the emphasis is on collaboration not competition. Unlike in England, the seven Health Boards in Wales Andrew Davies, Chairman deliver an integrated service and are responsible for both commissioning and planning all levels of citizen-centred healthcare services, as well as delivering them. In practice, this means that ABMU Health Board is delivering - and developing - services which range from primary and community health care, mental health, and responsibility for public health, through to highly specialised tertiary services. We are doing this in close partnership with our local authority, third sector -

Patient Experience Report April - June 2019
Appendix 1 Patient Experience Report April - June 2019 This report provides information on Patient Feedback and Experience, what it means and how we are using it to improve the service. Included within this report is the current performance of The Health Board’s Service Delivery Units and learning. Index 1. Patient Experience Update ........................................ Page 2 2. Learning from Events............................................... Page 9 3. Compliments ................................................................ Page 12 4. Concerns Management................................................. Page 13 5. Patient Safety Solutions ………………………………… Page 15 6. Arts in Health................................................................. Page 16 7. Delivery Unit Reports .................................................... Page 19 __________________________________________________________________________________________ 1 1. PATIENT EXPERIENCE 1.1 Inpatient Discharge Feedback Rates The Patient Experience Team continues to provide support and guidance to the Service Delivery Units (“SDU”) on increasing the number of surveys completed. The graph below indicates the discharge feedback rate benchmarked against the best performing Trusts for patient feedback returns in NHS England (35%). The Health Board’s aim is to increase the rate to 35%. April 2019 was 24.16%, May 2019 was 23.32% and June 2019 was 26.56%. Apr-19 May-19 Jun-19 NHS England Discharge 35.0% 35.0% 35.0% Swansea Bay UHB Inpatient Discharge 24.2% 23.3% 26.6% __________________________________________________________________________________________ -

Incidence, Prevalence and Healthcare Outcomes in Idiopathic Intracranial
Published Ahead of Print on January 20, 2021 as 10.1212/WNL.0000000000011463 Neurology Publish Ahead of Print DOI: 10.1212/WNL.0000000000011463 Incidence, Prevalence and Healthcare Outcomes in Idiopathic Intracranial Hypertension: A Population Study Latif Miah MBBCh1*; Huw Strafford MSc1*; Beata Fonferko-Shadrach MPH1; Joe Hollinghurst PhD1; Inder MS Sawhney MD1,2; Savvas Hadjikoutis MD2, Mark I Rees DSc1,3; Rob Powell PhD1,2; Arron Lacey PhD1; W Owen Pickrell PhD1,2 The Article Processing Charge was funded by Health Data Research (HDR) UK. This is an open access article distributed under the terms of the Creative Commons Attribution License 4.0 (CC BY), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Neurology® Published Ahead of Print articles have been peer reviewed and accepted for publication. This manuscript will be published in its final form after copyediting, page composition, and review of proofs. Errors that could affect the content may be corrected during these processes. Copyright © 2021 The Author(s). Published by Wolters Kluwer Health, Inc. on behalf of the American Academy of Neurology. Author affiliations: 1Swansea University Medical School, Swansea University, Swansea; 2Neurology Department, Morriston Hospital, Swansea Bay University Health Board; 3Faculty of Medicine and Health, University of Sydney. *These authors contributed equally to the manuscript Online supplementary data (uploaded as a separate file to Zenodo repository): Tables e-1 to e-8, Figures e-1 to e-5 Web Address: https://zenodo.org/record/4064064 File name: Supp_Data_IIH.docx Keywords: Idiopathic intracranial hypertension, Cohort studies, Prevalence studies, Incidence studies, Quality of life Publication History: This article has not been published previously Submission Type: Article Title character count: 104 Number of Tables: 2 Number of Figures: 5 Number of References: 23 Word count (abstract): 244 Word count (paper): 3567 Corresponding author: Dr. -

Report on the Examination Into the Swansea Local Development Plan 2010 – 2025
Adroddiad i Gyngor Report to Swansea Abertawe Council gan: by: Rebecca Phillips BA (Hons) MSc DipM Rebecca Phillips BA (Hons) MSc DipM MRTPI MCIM MRTPI MCIM Paul Selby BEng (Hons) MSc MRTPI Paul Selby BEng (Hons) MSc MRTPI Arolygyddion a benodir gan Weinidogion Inspectors appointed by the Welsh Cymru Ministers Dyddiad: 31/01/19 Date: 31/01/19 PLANNING AND COMPULSORY PURCHASE ACT 2004 (AS AMENDED) SECTION 64 REPORT ON THE EXAMINATION INTO THE SWANSEA LOCAL DEVELOPMENT PLAN 2010 – 2025 Plan submitted for examination on 28 July 2017 Hearings held 6 February – 28 March 2018 and 10 – 11 September 2018 Cyf ffeil/File ref: 515477 Swansea Local Development Plan 2010-2025 – Inspectors’ Report Abbreviations used in this report AA Appropriate Assessment AONB Area of Outstanding Natural Beauty AQMA Air Quality Management Area CBEEMS Carmarthen Bay and Estuaries European Marine Site DAMs Development Advice Maps DCWW Dŵr Cymru Welsh Water FCA Flood Consequences Assessment HRA Habitats Regulations Assessment IDP Infrastructure Delivery Plan IMAC Inspectors’ Matters Arising Change LDP Local Development Plan LHMA Local Housing Market Assessment LPA Local Planning Authority LSA Local Search Area MAC Matters Arising Change MoU Memorandum of Understanding NRW Natural Resources Wales PPW Planning Policy Wales RSL Registered Social Landlord SA Sustainability Appraisal SCARC Swansea Central Area Retail Centre SCARF Swansea Central Area Regeneration Framework SDA Strategic Development Area SEA Strategic Environmental Assessment SHPZ Strategic Housing Policy -

View in Website Mode
31 bus time schedule & line map 31 Swansea - Morriston Cross View In Website Mode The 31 bus line (Swansea - Morriston Cross) has 4 routes. For regular weekdays, their operation hours are: (1) Birchgrove: 7:30 AM - 10:50 PM (2) Morriston: 3:10 PM (3) Morriston Hospital: 7:00 AM - 7:05 PM (4) Swansea: 6:40 AM - 10:00 PM Use the Moovit App to ƒnd the closest 31 bus station near you and ƒnd out when is the next 31 bus arriving. Direction: Birchgrove 31 bus Time Schedule 32 stops Birchgrove Route Timetable: VIEW LINE SCHEDULE Sunday 7:50 PM - 10:50 PM Monday 7:30 AM - 10:50 PM Bus Station H, Swansea Garden Street, Swansea Tuesday 7:30 AM - 10:50 PM Sainsbury'S, St Thomas Wednesday 7:30 AM - 10:50 PM Quay Parade, Swansea Thursday 7:30 AM - 10:50 PM Ship Inn, St Thomas Friday 7:30 AM - 10:50 PM Kilvey Terrace, Grenfell Park Saturday 8:05 PM - 10:50 PM Pentreguinea Road, Swansea Maesteg Street, Grenfell Park Foxhole Road, Foxhole 31 bus Info Direction: Birchgrove Pentrechwyth Road, Pentre-Chwyth Stops: 32 Trip Duration: 33 min Gwyndy Stores, Pentre-Chwyth Line Summary: Bus Station H, Swansea, Sainsbury'S, St Thomas, Ship Inn, St Thomas, Kilvey Pen-Y-Garn, Hanover Square Terrace, Grenfell Park, Maesteg Street, Grenfell Park, B5444, Bonymaen Community Foxhole Road, Foxhole, Pentrechwyth Road, Pentre- Chwyth, Gwyndy Stores, Pentre-Chwyth, Pen-Y-Garn, Jersey Arms, Pentre-Chwyth Hanover Square, Jersey Arms, Pentre-Chwyth, Chip Shop, Bonymaen, Bonymaen Inn, Bonymaen, Clinic, Chip Shop, Bonymaen Bonymaen, Caernarfon Way, Bonymaen, Cefn Hengoed School, -

Neath 32 Swansea
First Swansea - Birchgrove - Morriston Hospital 31 via Bonymaen, Trallwn & Enterprise Park Swansea - Neath 32 via Bonymaen, Trallwn, Birchgrove & Skewen Swansea - Trallwn/Frederick Place 33 via Bonymaen MONDAY TO FRIDAY Ref.No.: 71R Service No 33 33 31 31 32 33 31 33 32 33 31 33 32 33 SD Swansea City Bus Station 0550 0635 .... 0730 0745 0800 0815 0830 0845 0900 0915 0930 0945 1000 Sainsbury's 0554 0639 .... 0734 0749 0804 0819 0834 0849 0904 0919 0934 0949 1004 St Thomas (Ship Inn) 0556 0641 .... 0736 0753 0806 0821 0836 0853 0906 0921 0936 0953 1006 Maesteg Street 0558 0643 .... 0739 0755 0810 0825 0840 0855 0910 0925 0940 0955 1010 Bonymaen Inn 0601 0647 0700B0746 0800 0815 0830 0845 0900 0915 0930 0945 1000 1015 Colwyn Avenue (Post Office) 0604 0650 0704 0748 0805 0820 0835 0850 0905 0920 0935 0950 1005 1020 Trallwn (Shops) 0609 0656 0710 0754 0811 0826 0841 0856 0911 0926 0941 0956 1011 1026 Trallwn Glan-y-Wern Road .... 0658 .... .... .... 0829 .... 0859 .... 0929 .... 0959 .... 1029 Frederick Place (Brynteg) .... 0702 .... .... .... 0834 .... 0904 .... 0934 .... 1004 .... 1034 Peniel Green 0611 .... 0713 0759 0816 .... 0844 .... 0916 .... 0944 .... 1016 .... Birchgrove (Ffordd-y-Mynydd) .... .... .... .... 0820 .... .... .... 0920 .... .... .... 1020 .... Birchgrove (Bridgend Inn) 0615 .... 0717 .... 0822 .... 0850 .... 0922 .... 0950 .... 1022 .... Birchgrove School .... .... .... 0806 .... .... .... .... .... .... .... .... .... .... Birchgrove (Heol Dulais) 0616 .... 0719 .... 0824 .... 0852 .... 0924 .... 0952 .... 1024 ... -
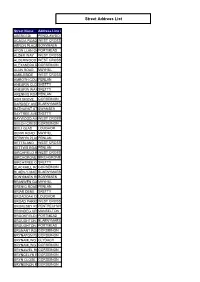
Street Address List
Street Address List Street Name Address Line 2 ABERCEDI PENCLAWDD ACACIA ROAD WEST CROSS AERON PLACEBONYMAEN AFON LLAN GARDENSPORTMEAD ALDER WAY WEST CROSS ALDERWOOD ROADWEST CROSS ALEXANDRA ROADGORSEINON ALUN ROAD MAYHILL AMBLESIDE WEST CROSS AMROTH COURTPENLAN ANEURIN CLOSESKETTY ANEURIN WAYSKETTY ARENNIG ROADPENLAN ASH GROVE GORSEINON BARDSEY AVENUEBLAENYMAES BATHURST STREETSWANSEA BAYTREE AVENUESKETTY BAYWOOD AVENUEWEST CROSS BEECH CRESCENTGORSEINON BEILI GLAS LOUGHOR BERW ROAD MAYHILL BERWYN PLACEPENLAN BETTSLAND WEST CROSS BETTWS ROADPENLAN BIRCHFIELD ROADWEST CROSS BIRCHGROVE ROADBIRCHGROVE BIRCHTREE CLOSESKETTY BLACKHILL ROADGORSEINON BLAEN-Y-MAESBLAENYMAES DRIVE BONYMAEN ROADBONYMAEN BRANWEN GARDENSMAYHILL BRENIG ROAD PENLAN BRIAR DENE SKETTY BROADOAK COURTLOUGHOR BROAD PARKSWEST CROSS BROKESBY ROADPENTRECHWYTH BRONDEG CRESCENTMANSELTON BROOKFIELD PLACEPORTMEAD BROUGHTON AVENUEBLAENYMAES BROUGHTON AVENUEPORTMEAD BRUNANT ROADGORSEINON BRYNAFON ROADGORSEINON BRYNAMLWG CLYDACH BRYNAMLWG ROADGORSEINON BRYNAWEL ROADGORSEINON BRYNCELYN ROADGORSEINON BRYN CLOSE GORSEINON BRYNEINON ROADGORSEINON BRYNEITHIN GOWERTON BRYNEITHIN ROADGORSEINON BRYNFFYNNONGORSEINON ROAD BRYNGOLAU GORSEINON BRYNGWASTADGORSEINON ROAD BRYNHYFRYD ROADGORSEINON BRYNIAGO ROADPONTARDULAIS BRYNLLWCHWRLOUGHOR ROAD BRYNMELIN STREETSWANSEA BRYN RHOSOGLOUGHOR BRYNTEG CLYDACH BRYNTEG ROADGORSEINON BRYNTIRION ROADPONTLLIW BRYN VERNEL LOUGHOR BRYNYMOR THREE CROSSES BUCKINGHAM ROADBONYMAEN BURRY GREENLLANGENNITH BWLCHYGWINFELINDRE BYNG STREET LANDORE CABAN ISAAC ROADPENCLAWDD -

Swansea Council
Swansea Council WEEKLY LIST OF PLANNING APPLICATIONS REGISTERED WEEK ENDING: 23rd October 2020 WEEK No. 43 On-line Planning Application Information Application forms, plans and supporting documentation for these applications can be viewed at http://property.swansea.gov.uk Phil Holmes BSc (Hons), MSc, Dip Econ Head of Planning & City Regeneration Application No: 2020/1958/OUT Date 21.10.2020 Registered: Electoral Division: Bishopston - Area 2 Status: Being Considered Map Ref: 258029 188733 Development Type: Minor Dwellings Location: Land To Rear, 97 Bishopston Road, Bishopston, Swansea, SA3 3EW Proposal: Detached dwelling (outline) Applicant: Mr Robert Jenkins Agent: Miss Helen Flynn Application No: 2020/2111/FUL Date 22.10.2020 Registered: Electoral Division: Bishopston - Area 2 Status: Being Considered Map Ref: 258319 188146 Development Type: Householder Location: 30 Whitestone Road, Bishopston, Swansea, SA3 3DB Proposal: Two single storey side extensions, single storey rear extension with recessed balcony above, side roof extension to link existing dormers, three rooflights to the North East elevation, one roof light to the South West elevation, fenestration alterations and widening of driveway / access point. Applicant: Mr & Mrs Antwhistle Agent: Mr Adam Rewbridge Application No: 2020/2125/TCA Date 21.10.2020 Registered: Electoral Division: Bishopston - Area 2 Status: Being Considered Map Ref: 257801 189440 Development Type: Tree Preservation Orders Location: 9 Church Lane, Bishopston, Swansea, SA3 3JT Proposal: Works to trees in Bishopston -

Abertawe Bro Morgannwg Nhs Trust
EXTREME WEATHER CONDITIONS POLICY AND PROCEDURE. This document may be made available in alternative formats and other languages, on request, as is reasonably practicable to do so. The policy has been screened for relevance to equality. No potential negative impact has been identified so a full equality impact assessment is not required. Policy Owner: Director of Workforce and OD Approved by: Health Board Partnership Forum Issue Date: December 2009 Revised: January 2020 Review Date: February 2021 Policy ID: HB69 Revised January 2020 Revised February 2015: Amendments: Section 3.1b- Staff are required to attend a Swansea Bay University Health Board site if they are able to do so. They should not report to health care sites outside of Swansea Bay University Health Board. Section 5.1- Staff employed by another NHS Health Board who attend premises within Swansea Bay University Health Board, must not be a permitted to work. (Agreed by HBPF 10th February 2015) Revised March 2018 Amendments: Section 4.3. The decision to pay staff for additional hours worked will be made by the Service Director or their designated representative. Section 4.8. Clarifies the position in the policy that where employees are not entitled to paid leave for their absence in accordance with section 3, and annual leave, time in lieu or working back the hours at another time are not available, the time off will be unpaid. (Agreed – HBPF- 1st March 2018) Revised January 2020: Amendments: Section 3.1 and section 5.1 amended to make reference to the Interim Procedure for Volunteer Staff Deployment during Adverse Weather. -
Development of a Mid and South West Wales Regional Centre Of
Name of Meeting Board Date of Meeting 28 March 2019 Agenda item: 9.2.280319 Development of a Mid and South West Wales Regional Centre of Excellence Cellular Pathology Laboratory, Regional Diagnostic Immunology Laboratory & Regional Medical Microbiology Facility at Morriston Hospital, Swansea Executive lead: Dr Quentin Sandifer, Executive Director of Public Health Services and Medical Director Author: Ms Heather Edwards, Business Planning Manager, Abertawe Bro Morgannwg University Health Board, with amendment where necessary by Dr Quentin Sandifer, Executive Director of Public Health Services and Medical Director Approval/Scrutiny Business Executive Team, 18 March 2019 route: Purpose To seek Board approval on the Strategic Outline Case (SOC) prior to submission to Welsh Government. Nationally NHS Pathology services face a number of challenges. Within the Mid and South West Wales’ region, Hywel Dda University Health Board (HDUHB), Abertawe Bro Morgannwg University Health Board (ABMUHB) and Public Health Wales NHS Trust (PHW) are struggling to manage workforce and sustainability pressures, to maintain quality and safety issues and to meet clinically driven targets. Without investment in sustainable services we cannot deliver essential improvements and fit for purpose laboratories. Investment would allow us to co-locate and develop regionalised services and to support more innovative and sustainable service models which could be future-proofed, and be flexible enough, to respond to changing demand, new technologies and innovations. In 2017 a South West Wales Regional Pathology Reconfiguration Project Board was established to draft a Strategic Outline Business Case (SOC) to address these regional challenges in line with the national direction of travel for regional pathology services. -

1D Woodlands Avenue Clydach Swansea Price £295,000 SA6
1d Woodlands Avenue Clydach Swansea SA6 5GA Price £295,000 • Small development of executive homes • Option to complete to own specification • Potential 5 bed+ accommodation • Possible granny flat within design • Open views to the front • Near local park and village centre • Good links to M4, and Morriston hospital • uPVC Double glazing will be provided • Pleasant open views to the front General Description Opportunity from the builder to complete this substantial new home to your own internal specification. Will provide 5 to 7 bedrooms, and incorpororate a granny annexe if required. Situated on a small development of similar executive homes, enjoying good links to the M4 and Morriston hospital. Tel: 01792 795 727 Email: [email protected] Web: www.ctf-uk.com 1d Woodlands Avenue, Clydach, Swansea SA6 5GA Property Description First Floor Opportunity to tailor this new home to your own internal specification!. The living space is on three levels, and Cloak Room could accommodate 5+ bedrooms, and incorporate a Lounge (16' 1" x 14' 3") or (4.90m x 4.35m) ’granny’ annexe if required. The current layout is for three bedrooms, all with en-suites, a lounge/dining room, Dining Area (17' 11" x 13' 4") or (5.45m x 4.06m) kitchen, utility, and a cloakroom, with the lower level left for the buyer to design to their own requirement which Kitchen/Breakfast Room (16' 5" x 15' 7") or (5.00m x could be a ’granny annexe’ or further bedrooms and 4.75m) living accommodation to the main house. The property is situated on a small development of similar executive Utility (6' 9" x 6' 5") or (2.05m x 1.95m) homes, ideally placed for good local amenities, parks, Bedroom (11' 10" x 11' 2") or (3.60m x 3.40m) golf course, the M4, Morriston hospital, and enjoys pleasant open views. -

Swansea Bay University Health Board
Schedule of Accreditation issued by United Kingdom Accreditation Service 2 Pine Trees, Chertsey Lane, Staines-upon-Thames, TW18 3HR, UK Swansea Bay University Health Board Issue No: 007 Issue date: 09 June 2021 ABM University Health Board Contact: Dr Andar Gunneberg Headquarters Tel: +44 (0) 1792 703988 1 Talbot Gateway 8918 E-Mail: [email protected] Port Talbot Website: www.abm.wales.nhs.uk SA12 7BR Accredited to ISO 15189:2012 Testing performed by the Organisation at the locations specified below Locations covered by the organisation and their relevant activities Laboratory locations: Location details Activity Location code Pathology Department Local contact Clinical Biochemistry M Morriston Hospital Dr Andar Gunneberg Haematology Heol Maes Eglwys Immunology Morriston Blood Transfusion Swansea Phlebotomy SA6 6NL Management of two lab-based blood fridges B Pathology Department Local contact Clinical Biochemistry Princess of Wales Hospital Dr Andar Gunneberg Haematology Coity Road Toxicology Bridgend Blood Transfusion CF31 1RQ Phlebotomy Management of two lab-based blood fridges Pathology department Local contact Clinical Biochemistry S Singleton Hospital Dr Andar Gunneberg Haematology Sketty Lane Blood Transfusion Swansea Phlebotomy SA2 8QA Management of two lab-based blood fridges Hot lab Local contact Full blood count MHL Pathology Department Dr Andar Gunneberg Routine coagulation tests Morriston Hospital Heol Maes Eglwys Morriston Swansea SA6 6NL Assessment Manager: AB2 Page 1 of 24 Schedule of Accreditation issued by United