Immunotherapy Also: Middleton Society, Advancing Health Equity
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Emergency Care and Trauma Symposium
51 st Annual Emergency Care and Trauma Symposium June 24-26, 2019 uwhealth.org/emssymposium Emergency Care and Trauma Kalahari Resort and Convention Center | 1305 Kalahari Drive | Wisconsin Dells 2019 51 st Annual Emergency Care and Trauma Symposium June 24-26, 2019 Kalahari Resort and Convention Center 1305 Kalahari Drive Wisconsin Dells, WI 53965 Sponsored by UW Health • UW Med Flight • UW CHETA UW Emergency Education Center University Hospital Level One Trauma Center Berbee Walsh Department of Emergency Medicine University of Wisconsin School of Medicine and Public Health uwhealth.org/emssymposium Emergency Care and Trauma Emergency Who Should Attend? The 51st Annual Emergency Care and Trauma Symposium is designed to educate prehospital and hospital emergency and trauma providers. This includes all levels of prehospital EMS personnel and hospital emergency nurses. Education for EMS and nursing will be offered, with presentations and hands-on sessions based on the educational need of the participant. Patients will be present when appropriate. Symposium Outcomes June 24th Outcomes Participants will: • Enhance their knowledge surrounding best practices for the emergent care of pediatric blunt trauma injuries. • Learn key elements of an effective mass casualty response program and strategies to address challenges that can occur during multi-agency responses at a large-scale incident. June 25th Outcomes Participants will: • Learn the newest strategies and techniques to care for patients in the pre-hospital and emergency settings. • Learn key assessments and interventions for suspected non-accidental trauma and human trafficking cases. • Enhance their knowledge of emergent/initial care for burn injuries. June 26th Outcomes Participants will: • Identify methods to collect and preserve evidence for criminal cases. -

White Coats a Strong Symbol for Students Who Dream of Becoming Doctors
Volume 16 • Number 4 • fALL 2014 FOR ALUMNI, FRIENDS, FACULTY AND STUDENTS OF THE UNIVERSITY OF WISCONSIN SCHOOL OF MEDICINE AND PUBLIC HEALTH Quarterly White Coats A STRONG SYMBOL FOR STUDENTS WHO DREAM OF BECOMING DOCTORS WOMEN IN LEADERSHIP p. 4 MEDICAL SCIENTIST TRAINING PROGRAM p. 10 MIDDLETON SOCIETY p. 16 There’s More Online! Visit med.wisc.edu/quarterly QUARTERLY JANUARY 2015 The Magazine for Alumni, Friends, Wednesday, January 14 Operation Education, Health Sciences Faculty and Students of the University of Wisconsin CONTENTS School of Medicine and Public Health Learning Center QUARTERLy • Fall 2014 • Volume 16 • Number 4 EDITOR Kris Whitman MARCH 2015 ART DIRECTOR Friday, March 6 Winter Event, Fluno Center, Madison Christine Klann PRINCIPAL PHOTOGRAPHER John Maniaci APRIL 2015 PRODUCTION Michael Lemberger Friday, April 24 WMAA Board of Directors Spring Meeting, Health Sciences Learning Center; WISCONSIN MEDICAL WMAA Awards Banquet, Union South ALUMNI ASSOCIATION (WMAA): EXECUTIVE DIRECTOR Karen S. Peterson MAY 2015 EDITORIAL BOARD Friday, May 15 SMPH Graduation, Union South Christopher L. Larson, MD ’75, chair Kathryn S. Budzak, MD ’69 Patrick McBride, MD ’80, MPH Maureen Mullins, MD ’79 JUNE 2015 CALENDAR Sandra L. Osborn, MD ’70 JUNe 4-6 • mediCAL ALUMNI WEEKEND Patrick Remington, MD ’81, MPH Wade Woelfle, MD ’95 Thursday, June 4- Reunions for classes of 1950, ’55, ’60, ’65 and ’75 Saturday, June 6 and a celebration for all classes that graduated EX OFFICIO MEMBERS in 1965 or earlier! Robert N. Golden, MD, Andrea Larson, Karen -

Board of Regents of the University of Wisconsin System Agenda
Board of Regents of the University of Wisconsin System Office of the Secretary 1860 Van Hise Hall Madison, Wisconsin 53706 (608)262-2324 October 29 2003 TO: Each Regent FROM: Judith A. Temby RE: Agendas and supporting documents for meetings of the Board and Committees to be held Thursday at The Lowell Center, 610 Langdon St. and Friday at 1820 Van Hise Hall, 1220 Linden St., Madison on November 6 and 7, 2003. Thursday, November 6, 2003 10:00 a.m. - 12:30 p.m. - Regent Study Groups • Revenue Authority and Other Opportunities, Lowell Center, Lower Lounge • Achieving Operating Efficiencies, Lowell Center, room B1A • Re-Defining Educational Quality, Lowell Center room B1B • The Research and Public Service Mission, State Capitol • Our Partnership with the State, Lowell Center, room 118 12:30 - 1:00 p.m. - Lunch, Lowell Center, Lower Level Dinning room 1:00 p.m. - Board of Regents Meeting on UW System and Wisconsin Technical College System Credit Transfer Lowell Center, room B1A/B1B 2:00 p.m. – Committee meetings: Education Committee Lowell Center, room 118 Business and Finance Committee Lowell Center, room B1A/B1B Physical Planning and Funding Committee Lowell Center, Lower Lounge 3:30 p.m. - Public Investment Forum Lowell Center, room B1A/B1B Friday, November 7, 2003 9:00 a.m. - Board of Regents 1820 Van Hise Hall Persons wishing to comment on specific agenda items may request permission to speak at Regent Committee meetings. Requests to speak at the full Board meeting are granted only on a selective basis. Requests to speak should be made in advance of the meeting and should be communicated to the Secretary of the Board at the above address. -

Fall 2020 in PDF Format
FOR UNIVERSITY OF WISCONSIN–MADISON ALUMNI AND FRIENDS FALL 2020 Badgers vs. the Pandemic Meet UW heroes in the fight against COVID-19. Page 22 Vision Protesters kneel near Memorial Library, showing solidarity with the Black Lives Matter movement. Following the killing of George Floyd by Minneap- olis police on Memorial Day weekend, demonstra- tions began in cities around the country, including Madison, where they centered on the capitol and State Street. Photo by Jeff Miller On Wisconsin 3 THE “DIDN’T MISS A SPOT” POLICY KnowYourDrive® rewards polished driving with big savings. You take the wheel when it comes to your savings with KnowYourDrive. Get a close look at your driving habits and free access to tools to improve your driving behaviors for a bigger discount. Because you should get rewarded for your attention to detail. Sign up today and get a 10% discount on auto insurance. Get a quote. Find an Agent. AmFam.com. American Family Mutual Insurance Company, S.I. & its Operating Companies, 6000 American Parkway, Madison, WI 53783 ©2020 018549 – 6/20 Some products not available in every state. Program discounts will vary based on driving behavior. Discount does not apply to fixed fees that are part of your policy. Discounts may vary by state, vehicle, policy form and company underwriting the auto policy. Discounts may not apply to all coverages. Discounts are subject to regulatory approval; some discounts may not be available in all states. Contents Volume 121, Number 3 Shakuntala Makhijani examines Lab mix Beau at the Dane County Humane Society. See page 46. -
THE KEY VOL 79 NO 3 AUTUMN 1962.Pdf
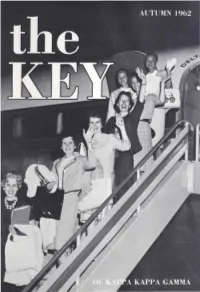
VOLUME 79 NUMBER 3 The first college women's frat ernity magazine Published continuously the KEY since 1882 OF KAPPA KAPPA GAMMA AUTUMN 1962 Send all editorial material and COVER: Airborne Kappas arrive on the first charter flight to correspondence to the a Kappa convention. Ranging up the steps, they are: Barbara EDITOR Russell Kunz, n A-Illinois, Champaign-Urbana alumna dele Mrs. Robert H . Simmons gate; Sue Sather, n IT-Washington, active delegate; ~ancy 15 6 North Roosevelt Avenue Columbus 9, Ohio Sampson Nethercutt, r H-Washington State, alumna VISitor; Virginia Pitts Malico, r r-Whitman, Spokane alumna deleg_ate; Martha Lynn, X-Minnesota, active visitor; Karen Rushmg, Send all business i terns to the X-Minnesota, active delegate; Diane Haas Clover, n-Kansas, BUSINESS MANAGER adviser to r Z-Arizona. Miss Clara 0. Pierce Fraternity Headquarters 530 East Town Street 3 Devotional given at opening session Columbus 16, Ohio (For other devotionals, see pages 11, 27, 29, 43, and 45) Send changes of address, six weeks prior to month of pub .. 4 " ... four square to all the winds that blow" lication, to 9 What I wish for a fraternity chapter FRATERNITY HEADQUARTERS 12 The rest is our own doing 530 East Town Street 19 The state of the Kappa union Columbus 16, Ohio 22 "All mimsy were the Borogoves" (Duplicate copies cannot be sent to replace those unde 23 Scholarship grants announced livered through failure to send advance notice.) 28 The World and K K r 30 A bit of this and that Deadline dates are August 1, September 25, November 15, 32 Alumnre Day activity January 15 for Autumn, Winter, Mid-Winter, and 33 Magazine sales bring rewards Spring issues respectively. -

Mcardle Laboratory for Cancer Research Department of Oncology
CANCER BIOLOGY GRADUATE PROGRAM UNIVERSITY OF WISCONSIN SCHOOL OF MEDICINE AND PUBLIC HEALTH Academic Policies and Procedures Handbook McArdle Laboratory for Cancer Research Department of Oncology 2017-2018 - 3 - I. PROGRAM OVERVIEW P.1-2 II. NEW STUDENTS P.3 III. ORIENTATION P.4 IV. ROTATIONS P.4-5 V. CURRICULUM REQUIREMENTS P.6-11 VI. ENROLLMENT P. 12-13 VII. PROGRESS REQUIREMENTS P. 13-17 VIII. GRIEVANCE PROCEDURES P.17-18 IX. FINANCIAL INFORMATION P. 18 X. HEALTH & WELLNESS P.19-20 XI. LAB SAFETY P.20-21 XII. MCARDLE BASICS P.21 XIII. PROGRAM CONTACTS P.21 4 I. PROGRAM OVERVIEW This handbook is intended for graduate students who are pursuing a Ph.D. Degree in Cancer Biology at the University of Wisconsin-Madison. The Cancer Biology Graduate Program is an interdepartmental program administered at the McArdle Laboratory for Cancer Research (also known as the Department of Oncology) in the School of Medicine and Public Health. The Cancer Biology Program consists of over 50 trainers that span multiple departments across UW-Madison. The UW-Madison Graduate School is the ultimate authority for granting graduate degrees at the University. The Graduate School’s Academic Policies and Procedures provide essential information regarding general University requirements (https://grad.wisc.edu/acadpolicy/). The policies in this handbook provide additional information specific to the Cancer Biology Program. Degrees and course requirements may change over time. Students are required to meet the degree and course requirements in effect when they entered the program. Administrative procedures and processes may also change over time. Students are required to follow the procedures and processes listed in the most current handbook. -

THE SEARCH for the CHAIR, BERBEEWALSH DEPARTMENT of EMERGENCY MEDICINE Madison, Wisconsin
THE SEARCH FOR THE CHAIR, BERBEEWALSH DEPARTMENT OF EMERGENCY MEDICINE Madison, Wisconsin The University of Wisconsin School of Medicine and Public Health invites applications and nominations for the position of chair of the BerbeeWalsh Department of Emergency Medicine. The Opportunity Over the past decade, the BerbeeWalsh Department of Emergency Medicine (DEM) has established an exceptionally strong financial, operational, and administrative foundation. The second chair in the department’s history will have the opportunity to lead a proven team that is poised for growth, dedicated to providing optimal and outstanding patient care for individual patients and families, and committed to developing tomorrow’s leaders in emergency medicine. Today, the department is home to more than forty faculty, including faculty with dual certification in pediatrics, critical care, and palliative care. The emergency medicine residency program welcomes 13 residents per class and has hosted up to nine fellowship programs per year. A clinically skilled and stable advanced practice provider (APP) pool is integrated seamlessly into the department, taking on a variety of learner, provider, and administrative roles. Together, the faculty, residents, and APPs staff four emergency departments (EDs): the adult and pediatrics, burn and trauma, level I ED at the University Hospital; the American Family Children’s Hospital ED; The American Center ED on the east side of Madison that is adjacent to a planned $255 million expanded hub for specialty care; and the William S. Middleton Memorial Veteran’s Hospital ED. The department’s providers deliver true emergency care as part of an operationally efficient health system. Approximately more than 90 percent of the patient market is insured, and therefore lower-acuity patients have robust urgent care centers as alternative options to the ED. -

Patient Survives Near Fatal Accident Shares Amazing Story and an Important Safety Message
UW Health OurConnecting you to health news and resources • uwhealth.org SPRING/SUMMER 2014 Patient Survives Near Fatal Accident Shares Amazing Story and an Important Safety Message There are 19 steps inside the stairwell at the UW Health “We were surprised to get him out of the OR,” Agarwal Rehabilitation Clinic in Middleton, WI. says. “An entire team took care of him and got him through this injury–which should have been fatal.” A child could zip up and down those stairs, without a second thought. But for Mark Friend, every step up and UW Health plastic and reconstructive surgeon Samuel down is a calculated process, as he learns how to Poore, MD and UW Health orthopedic surgeon David manipulate–and more importantly, trust–his state-of- Goodspeed, MD followed up Dr. Agarwal’s work on the-art prosthetic leg. Friend’s amputated leg. But before going into surgery, Goodspeed called Amy Paulios of Prosthetic His prosthetic knee has a microprocessor in it, one that Laboratories in Monona. “He had the foresight to think bends and helps slow the speed of his body as it lowers. about how much of Friend’s leg was needed for a “Once that goes, you’ve got to trust yourself to go to prosthetic limb.” Paulios says, “He was thinking that far the next step,” says Friend, who has to pull his leg back ahead on Mark’s behalf, which I find to be phenomenal.” to trigger the process. It’s a complicated system, one Friend also suffered serious injuries to his right leg and that requires a lot of thought and everything going right underwent major reconstructive knee surgery. -

Out on a Limb Wollerman Steven R
SELL YOUR HOME EASIER! Local, Experienced & Trusted Get the RIGHT Real Estate Advice... Get Geiger JASON GEIGER It’s your paper! (608) 277-2167 Friday, July 11, 2014 • Vol. 1, No. 5 • Fitchburg, WI • ConnectFitchburg.com • $1 Office Next to Great Dane - Fitchburg GeigerRealtors.com adno=358758-01 Inside Library ‘pulled this town together’ Fitchburg native chases songwriting But at its third birthday, dreams Page 10 supporters say there’s still lots of work to do SCOTT GIRARD Unified Newspaper Group Kathleen Martens has lived in Fitchburg for 28 years, but until three years ago, she had to go to Oregon to get her fix of nonfiction books. Flea market creates “I read a lot,” said Marten, one of 12,000 Fitch- camaraderie burg residents who had a library card in another community before the library was built, based on statistics given by library supporters in 2009. Page 7 Marten was on hand when that changed, on June 29, 2011, with the opening of Fitchburg’s own library. Three years later, she and her two grand- Sports sons were back to celebrate the building’s third birthday. “I think (the library’s) what has pulled this town together,” Martens said. “It’s become such an important part of our life.” Becoming an important part of community life is what the ultimate goal for the library was, in a city that has no downtown and no school district of its own, said library board member Pauli Niko- lay. VAHS boys win “We’d like the heart and soul of the community state lacrosse to be the library, and provide functions for babies all the way up through grandparents and senior championship citizens,” Nikolay said. -

Senate Journal
--- - - -- -----.- .. __ . -- - Ninetieth Regular Session WEDNESDAY, September 2, 1992 The chief clerk makes the foUowing entries under the The report for the period April I, 1992, through June above date. 30, 1992, is attached. Sina:rely, PETITIONS AND COMMUNICATIONS James R. Klauser State of Wisconsin Secretary ~tofA~tration State of Wisconsin AUSUSt 18, 1992 Legislative Audit Bureau To the Honorable the Lesislature: September I, 1992 This report is transmitted as required by sec. To the Honorable the Legislature: 20.002(11)(f) of the Wisconsin Statutes, (for distribution to the appropriate standing committees under sec. We have completed an evaluation ofthe ~t 13.172(3) Stats.), and confirms that the Department of of Natural Resoun:es' Nonpoint Source Water Pollution Administration has found it necessary to exercise the Abatement Program. This is the Second of two reports "temporary reaUocation of balances" authority provided mandated by Wisconsin Act 27, the 1987-89 Biennial by this section in order to meet payment responsibilities Budget. We completed the first evaluation in May 1989. and cover resultins negative balances during the month The Program is managed in cooperation with the of July, 1992. Department of Agriculture, Trade and Consumer On July 13, 1992, the Transportation Fund balana: Protection's Soil and Water Resource Management was $-14.9 miUion. This shortfall continued until July Program. 23, 1992 when the balana: reached $+9.2 million. The Sina: our last evaluation, the Department of Natural shortfall was due to delay in the receipt of Revenue Bond Resources has improved some financial practices related proceeds. to the Nonpoint program, and the problem of a recurring On July 20, 1992, the Environmental Qean-up Fund large balana: has been corrected. -

Minutes of the Regular Meeting of the Board of Regents of the University of Wisconsin: May 12, 1956
Minutes of the regular meeting of the Board of Regents of the University of Wisconsin: May 12, 1956. 1956 [s.l.]: Board of Regents of the University of Wisconsin System, 1956 https://digital.library.wisc.edu/1711.dl/ZAOLYFQ6AKUOX87 Copyright 2008 Board of Regents of the University of Wisconsin System The libraries provide public access to a wide range of material, including online exhibits, digitized collections, archival finding aids, our catalog, online articles, and a growing range of materials in many media. When possible, we provide rights information in catalog records, finding aids, and other metadata that accompanies collections or items. However, it is always the user's obligation to evaluate copyright and rights issues in light of their own use. 728 State Street | Madison, Wisconsin 53706 | library.wisc.edu a | | CO | | Regular Board 5/12/56 - 2 | | - Upon motion of Regent Watson, seconded by Regent Werner, it was os | VOTED, That the gifts and grants listed in EXHIBIT A, attached, be ac~= ~ | cepted; and that the Vice President of Business and Finance be authorized to sign | | the agreements. - | | SO a | oo | | a Upon motion of Regent Renk, seconded by Regent Steiger, it was | a - VOTED, That the Actions by the President, since the April 7, 1956, meeting | of the Board of Regents, covering resignations and terminations, appointments, 7 | | leaves of absence, changes in status or salary of personnel, and resignations to ac- | cept other U.W. appointments (EXHIBIT B attached) be approved, ratified and con= > firmed, | Oo | — | OO President Fred reported that The Benjamin Smith Reynolds Award for Excel- | 7 lence in Teaching of Future Engineers was awarded to Professor Raymond J. -

GRADUATE STUDENT LIFE 2018–2019 Graduate Student Life
GRADUATE STUDENT LIFE 2018–2019 Graduate Student Life 2018–2019 2018–2019 edition of Graduate Student Life was updated and published in May 2018 as a service to graduate students at the University of Wisconsin–Madison. Table of Contents Introduction Welcome to Graduate School at UW–Madison 1. University of Wisconsin–Madison ........................................................................5 UW–Madison History, Getting Started, Studying, Planning Ahead 2. City of Madison ....................................................................................................18 Weather, Government, Staying Informed, Getting Involved, City Events, Accommodations for Visitors, Beyond Madison 3. Student Services and Organizations ..................................................................28 Graduate Student Involvement, The Wisconsin Unions, Diversity and Multiculturalism on Campus, Students with Disabilities, Family and Parent Resources, Food Resources 4. International Students.........................................................................................41 International Student Resources, New International Students 5. Finances and Employment ..................................................................................51 Tuition, Student Accounts, and Bills, Graduate Student Funding, Financial Information, Help with Money Management 6. Housing ................................................................................................................61 Campus Area Housing, Campus Housing 7. Transportation ......................................................................................................69