Rosita-2 Project
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Actors Against Trafficking for Labour Exploitation
Actors against Trafficking for Labour Exploitation Report on Cooperation between Stakeholders at the National Level in the countries of the Baltic Sea region to Address Trafficking for Labour Exploitation Written by: Stella Rössborn Council of the Baltic Sea States (CBSS) Secretariat Bjarney Friðriksdóttir, Anna Ekstedt, Anthony Jay, Vineta Polatside This study was produced with funding from the Task Force against Trafficking in Human Beings. This publication has not been formally edited © The Council of the Baltic Sea States, January 2013 2 The aim of the study is to obtain an overview national level in each member state. The of the different actors who are currently report has been designed to present an involved in the work of combating and overview of relevant actors and mandates; preventing trafficking for labour exploitation. governmental as well as non-governmental. It Actors have occasionally also been included further analyses the current forms of who have a significant potential to be involved cooperation, in terms of mechanisms in place in this work. In addition, the study has as well as relevant policies and legislation. analysed existing resources and structures, primarily for cooperation at the national level. The findings are based mainly on the expertise and experience of national actors currently This work was a necessary starting point working on the issue of trafficking for labour in identifying existing resources as well as exploitation and forced labour. As such, the challenges encountered by different actors report is meant to capture resources as well as at the national level. The results have been challenges as they are perceived and identified compiled into the report which will serve as a by the relevant national actors, according to starting point and as a basis for dialogue at the the individual context in that specific country. -

Annual Report
2011 annual report 2011 Contents Foreword 3 Organization and Staffing 4-5 Deprivation of Position by Court Judgment 6-7 Documenting Decisions in Criminal Cases 8-9 Police Corruption in Norway 10-11 The Conduct of Police Employees 12-13 The Use of Police Signature in Private Contexts 14-15 Incidents during Detention 16-17 Statistics 18-21 Decisions to Prosecute in 2011 22-25 Emergency Turn-Outs in 2011 26-27 Administrative Assessments in 2011 28-31 Court cases in 2011 32-35 Meetings and Lectures in 2011 36-37 The Norwegian Bureau for the Investigation of Police Affairs 38 Articles from Previous Annual Reports 39 annual report Copy Print Photo / Norwegian Bureau for the / PJ-trykk, Oslo / Frank Holm, Alelier Klingwall Investigation of Police Affairs / Cornelius Poppe, Berit Roald, ScanpiX Illustrations / Politiforum Design / layout / Harald Nygård / Getty Images / Newmarketing AS / Geir Hansen Foreword The purpose of the Annual Reports from the Bureau is, in addition to presenting statistical data, to point to opportunities for learning through experience. This year’s report focuses, among other things, on police detention. he Bureau has forwarded 220 cases that decisions regarding measures taken dur- the Bureau was maintained by the Director of to administrative assessment since its ing detention are not sufficiently documented. Public Prosecution. Testablishment on 1 January 2005. Typi- cally these cases have not resulted in punitive Despite the fact that the number of cases is One of the objectives of creating of the Bureau reactions, but the investigation has revealed a relatively small compared to the number of was to strengthen the public’s confidence in need for an improvement of routines. -

Calendario Uci 2020
CALENDARIO UCI 2020 23/10/19 01/11/19 59 Vuelta a Guatemala GUATEMALA 2.2 25/10/19 03/11/19 Tour du Faso BURKINA FASO 2.2 02/11/19 03/11/19 Road Elite Caribbean Championships CUBA 1.2 02/11/19 10/11/19 Tour de Singkarak INDONESIA 2.2 08/11/19 10/11/19 Tour of Quanzhou Bay CHINA 2.2 10/11/19 10/11/19 Tour de Okinawa JAPAN 1.2 10/11/19 17/11/19 Tour du Sénégal SENEGAL 2.2 17/11/19 23/11/19 Tour of Fuzhou CHINA 2.1 18/12/19 22/12/19 Tour of Selangor MALAYSIA 2.2 16/12/19 25/12/19 Vuelta Internacional a Costa Rica COSTA RICA 2.2 04/01/20 06/01/20 Cambodia Bay Cycling Tour CAMBODIA 2.2 15/01/20 19/01/20 New Zealand Cycle Classic NEW ZEALAND 2.2 25/01/20 25/01/20 Gravel and Tar Classic NEW ZEALAND 1.2 20/01/20 26/01/20 La Tropicale Amissa Bongo GABON 2.1 21/01/20 26/01/20 Santos Tour Down Under AUSTRALIA 2.UWT 30/01/20 30/01/20 Race Torquay AUSTRALIA 1.1 30/01/20 30/01/20 Trofeo Felanitx, Ses Salines, Campos SPAIN 1.1 31/01/20 31/01/20 Lloseta - Andratx SPAIN 1.1 01/02/20 01/02/20 Trofeo Serra de Tramuntana SPAIN 1.1 02/02/20 02/02/20 Grand Prix Cycliste la Marseillaise FRANCE 1.1 02/02/20 02/02/20 Trofeo Playa de Palma - Palma SPAIN 1.1 02/02/20 02/02/20 Cadel Evans Great Ocean Road Race AUSTRALIA 1.UWT 04/02/20 08/02/20 Tour of Saudi Arabia SAUDI ARABIA 2.1 08/02/20 08/02/20 Tel Aviv Classic ISRAEL 1.1 05/02/20 09/02/20 Etoile de Bessèges FRANCE 2.1 05/02/20 09/02/20 Jayco Herald Sun Tour AUSTRALIA 2.1 05/02/20 09/02/20 Volta a la Comunitat Valenciana SPAIN 2.Pro 11/02/20 16/02/20 Tour Colombia 2.1 COLOMBIA 2.1 11/02/20 16/02/20 Tour of Oman -

Dialogue a Journal from the Petroleum Safety Authority Norway
2013 no 2 DIALOGUE A JOURNAL FROM THE PETROLEUM SAFETY AUTHORITY NORWAY CAN WE PLAN FOR THE UNTHINKABLE? 22 JULY IN AMENAS NOKAS SECTION 9-3 CAN WE PLAN FOR THE UNTHINKABLE? DIALOG UE THE UNTHINKABLE Emergency preparedness is a key term for everyone involved with both security and safety in the petroleum sector. Players must have effective systems in place to prevent and respond to hazards and accidents which could result from their everyday activities. But they must also be prepared to deal with possible conscious attacks – 4 10 terrorism and deliberate assaults. No pat definitions exists for either security or safety. Incidents occasionally occur which nobody imagined possible and which no scenario had taken into account. Such events can overturn established truths and pose deep challenges for society. SECURITY The PSA has been given responsibility in 2013 for “security section” 9-3 of the Petroleum Activities Act, covering emergency preparedness 26 against deliberate attacks. That requires the industry to adopt and maintain measures to secure its facilities. This issue accordingly takes a look at three watershed events of recent years – the Nokas robbery in Stavanger during 2004, CONTENTS the terrorist attacks in Oslo and Utøya on 22 July 2011, and the BEING BETTER PREPARED 4-7 hostage drama at Algeria’s In Amenas facility in 2013. We introduce some of those who have sought to establish what CHANGING THREATS 8-9 failed, and present their analyses of what went wrong. They make 12 PREPAREDNESS A PRIORITY 10-11 it clear that work on risk and preparedness cannot be confined to particular industries. -

Politiet Politidirektoratet
POLITIET POLITIDIREKTORATET Arbeids- og sosialdepartementet NATIONAL POLICE DIRECTORATE Postboks 8019 Dep 0030 OSLO Deres referanse: Vår referanse: Sted, Dato 15/6209 201503828-19 008 Oslo, 09.12.2015 HØRING - ENDRINGER I FORSKRIFT OM HMS-KORT FOR BYGGE- OG ANLEGGSPLASSER, FORSKRIFT OM OFFENTLIG GODK-1ENNING AV RENHOLDSVIRKSOMHETER OG FORSKRIFT OM SIKKERHET, HELSE OG ARBEIDSMIUØ PÅ BYGGE- OG ANLEGGSPLASSER (BYGGHERREFORSKRIFTEN) Politidirektoratet viser tll Arbeids- og soslaldepartementets høringsbrev av 11. september 2015 om endringer I forskrift om HMS-kort for bygge- og anleggsplasser, forskrift om offentlig godkjenning av renholdsvirksomheter og forskrift om sikkerhet, helse og arbeidsmIljø på bygge- og anleggsplasser (byggherreforskriften). Justis- og beredskapsdepartementet oversendte høringen tIl Politidirektoratet den 13. oktober 2015. FrIst for merknader tiI Arbeids- og soslaldepartementet er satt til 11. desember 2015. Politidirektoratet har forelagt høringen for underliggende instanser. Vi har mottatt høringsuttalelser fra Kripos, Nasjonalt ID-senter, Oslo pollUdistrIkt og Rogaland politidistrikt, som er delvis innarbeidet i direktoratets høringssvar. Uttalelsene følger vedlagt I kopi. Innledning Forslagene som fremmes i høringen er et ledd I gjennomføringen av regjeringens strategl mot arbeidslivskriminalitet. Det fremgår av høringsnotatet at ArbeidstIlsynet i økende grad erfarer at kortene blir mIsbrukt. Typiske eksempler er angitt å være utstedelse av kort på bakgrunn av falske legitimasjonsdokumenter kort blIr brukt av -
2021 UCI ROAD Calendar - Interac�Ve Version Coming… 18.11.2020
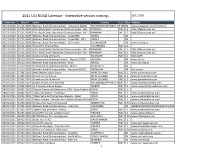
2021 UCI ROAD Calendar - Interac5ve version coming… 18.11.2020 Date From Date To Name Country Cat. Class WebSite 15/11/2020 16/11/2020 Na5onal Road Championships - Venezuela (2020) BOLIVARIAN REPUBLIC OF VENEZUELACN www,instagram.com/fvciclismo 21/11/2020 21/11/2020 Elite Road Central American Championships - ME - ITTPANAMA ME 1.2 hUp://fepaci.com.pa/ 21/11/2020 21/11/2020 Elite Road Central American Championships - WE - ITTPANAMA WE 1.2 hUp://fepaci.com.pa/ 21/11/2020 21/11/2020 Na5onal Road Championships - Israel (IRR) ISRAEL CN 21/11/2020 21/11/2020 Na5onal Road Championships - Israel (IRR - WE) ISRAEL CN 15/11/2020 22/11/2020 Na5onal Road Championships - El Salvador EL SALVADOR CN www.fsc.org.sv 18/11/2020 22/11/2020 Grand Prix Chantal Biya CAMEROON ME 2.2 22/11/2020 22/11/2020 Elite Road Central American Championships - WE - IRRPANAMA WE 1.2 hUp://fepaci.com.pa/ 22/11/2020 22/11/2020 Elite Road Central American Championships - ME - IRRPANAMA ME 1.2 hUp://fepaci.com.pa/ 23/11/2020 28/11/2020 Vuelta Ciclista al Ecuador ECUADOR ME 2.2 ECUADOR 02/12/2020 05/12/2020 Championnats Na5onaux Route - Algérie (2020) ALGERIA CN www.fac.dz 05/12/2020 06/12/2020 Na5onal Road Championships - Brasil BRAZIL CN www.cbc.esp.br 11/12/2020 13/12/2020 Championnats Na5onaux Route - Maroc MOROCCO CN 12/12/2020 13/12/2020 Na5onal Road Championships - Paraguay (2020) PARAGUAY CN Fpc.org.py 13/01/2021 17/01/2021 New Zealand Cycle Classic NEW ZEALAND ME 2.2 www.cycletournz.com 23/01/2021 23/01/2021 Gravel and Tar Classic NEW ZEALAND ME 1.2 www.gravelandtar.com -

Offshore Terror Preparedness in the Barents Sea
Offshore terror preparedness in the Barents Sea “Preparing for the unexpected” EN310E: Master of Sciences in Energy Management Karin Dahl & Marte Haugan Master thesis – Master of Sciences in Energy Management Bodø, 2014 Preface This master thesis represents the final semester of a two-year Master of Science degree within the Energy Management program at Bodø Graduate School of Business and MGIMO University in Moscow. We have faced many challenges along the way in this study. This is mainly due to the limited information shared about terrorism, both from public and private actors. We have gathered highly important, interesting and informative material from our interviews with representatives from the petroleum industry and already published data. Throughout the study we have been confirmed by several participants the importance of this study for the petroleum industry’s security. First of all we want to give a sincere thanks to our supervisor, Odd Jarl Borch, for constructive criticism and guidelines along the way. He has been an incredibly important resource for us in terms of relevant literature, areas to focus on, interesting discussions and topics and especially to obtain interview candidates. Finally we will gratitude all the interview participants for their willingness to participate in this study sharing their knowledge and experience within the topic studied. Their input and information has been essential and highly necessary for the ability to conduct this research. Bodø, 20th May 2014 Karin Dahl & Marte Haugan Keywords: Preparedness team, Preparedness system, Terrorism, Barents Sea, Managerial roles, Security Bodø Graduate School of Business i Master thesis – Master of Sciences in Energy Management Bodø, 2014 Summary The petroleum industry is constantly moving further north on the NCS, where oil and gas operators are facing new challenges in more complex environments. -

2021 UCI World Calendar
2021 UCI ROAD Calendar - Interac5ve version coming... As of Feb 01, 2021 Date From Date To Name Country Cat Class WebSite 13/01/2021 17/01/2021 New Zealand Cycle Classic NEW ZEALAND ME 2.2 www.cycletournz.com 23/01/2021 23/01/2021 Gravel and Tar Classic NEW ZEALAND ME 1.2 www.gravelandtar.com 23/01/2021 23/01/2021 Gravel and Tar la Femme NEW ZEALAND WE 1.2 www.gravelandtar.com 17/01/2021 24/01/2021 Vuelta al Tachira en Bicicleta BOLIVARIAN REPUBLIC OFME VENEZUELA2.2 www.lavueltaaltachira.com 24/01/2021 24/01/2021 Clàssica Comunitat Valenciana 1969 - Gran Premio ValenciaSPAIN ME 1.2 26/01/2021 29/01/2021 Na5onal Road Championships - Qatar QATAR CN h[ps://qatarcycling.org/ 31/01/2021 31/01/2021 Grand Prix Cycliste la Marseillaise FRANCE ME 1.1 www.lamarseillaise.fr 06/02/2021 06/02/2021 Grand Prix Alanya TURKEY ME 1.2 www.cyclingalanya.com 03/02/2021 07/02/2021 Etoile de Bessèges - Tour du Gard FRANCE ME 2.1 www.etoiledebesseges.com 03/02/2021 07/02/2021 Na5onal Road Championships - Australia AUSTRALIA CN www.roadna5onals.org.au 05/02/2021 07/02/2021 Na5onal Road Championships - Namibia NAMIBIA CN www.namcf.org 07/02/2021 07/02/2021 Grand Prix Gazipasa TURKEY ME 1.2 www.cyclingalanya.com 11/02/2021 14/02/2021 Tour de la Provence FRANCE ME 2.Pro h[p://www.tourdelaprovence.fr/ 12/02/2021 14/02/2021 Na5onal Road Championships - New Zealand NEW ZEALAND CN www.eliteroadna5onals.nz 14/02/2021 14/02/2021 Clasica de Almeria SPAIN ME 1.Pro www.clasicadealmeria.net 18/02/2021 19/02/2021 Manavgat Side Junior TURKEY MJ 2.1 www.cyclingalanya.com 18/02/2021 -

Rider Name Nation Date of Birth Length (Cm) Weight (Kg) Favorite
Rider Name Nation Date of Length Weight Favorite Best Bio / fun fact birth (cm) (kg) race achievement 1. BARBIER France 18 December 1.79m 78 kg Le 4 Jours 1st place in Paris Rudy is a pure sprinter. He is Rudy 1992 de Troyes with his one of the fastest riders in the Dunkerque brother finishing world and the rider who gave 3rd and his five the team the biggest number other professional of victories last season. victories. 2. BERWICK Australia 15 december 1.75m 59kg 2nd in GC Herald 2021 will be Berwick’s first Sebastian 1999 Sun Tour 2020 year as a professional cyclist, and he will immediately compete on WorldTour level with the team. 3. BEVIN Patrick New 15 February 1.80m 75kg 4th place in the Bevin is an expierenced all- Zealand 1991 World rounder, especially skillful in Championships TT’s. He will be an asset in the individual time team’s Grand Tour ambitions. trial in 2019 4. BIERMANS Belgium 30 October 1.84 m 78 kg Paris- 9th GC Tour of Jenthe finished twice second in Jenthe 1995 Roubaix Belgium the Paris-Roubaix espoirs race, and won the Ronde van Vlaanderen U19 in 2013. Jenthe is a true classic- specialist, eating cobbles for breakfast. 5. BOIVIN Canada 25 May 1.8 m 78 kg Milan-San Two times Guillaume loves both sprinting Guillaume 1989 Remo Canadian national and classics. He grew up champion playing ice-hockey and is still a huge fan of the sport. In the team Boivin is better known as ‘G’. -

UCI ROAD Calendar - Season 2020 19.05.2020
UCI ROAD Calendar - Season 2020 19.05.2020 Date Date To Name Venue Country Category Class Email WebSite From 23/10/2019 01/11/2019 59 Vuelta a Guatemala GUA ME 2.2 fciclismo.guat www.fedeciclismogua.org [email protected] 02/11/2019 02/11/2019 Road Elite Caribbean Championships - ME ITT CUB ME 1.2 [email protected] 02/11/2019 02/11/2019 Road Elite Caribbean Championships - WE ITT CUB WE 1.2 [email protected] 25/10/2019 03/11/2019 Tour du Faso BUR ME 2.2 [email protected] www.tourdufaso.bf 03/11/2019 03/11/2019 Road Elite Caribbean Championships - ME IRR CUB ME 1.2 [email protected] www.copaci.org 03/11/2019 03/11/2019 Road Elite Caribbean Championships - WE IRR CUB WE 1.2 [email protected] 02/11/2019 10/11/2019 Tour de Singkarak INA ME 2.2 [email protected] 08/11/2019 10/11/2019 Tour of Quanzhou Bay CHN ME 2.2 [email protected] 10/11/2019 10/11/2019 Tour de Okinawa JPN ME 1.2 [email protected] www.tour-de-okinawa.jp 16/11/2019 16/11/2019 Tour De France Shanghai Criterium CHN ME CRT service@china- http://www.ch ina- letour.com letour.com 10/11/2019 17/11/2019 Tour du Sénégal SEN ME 2.2 [email protected]; [email protected] 17/11/2019 23/11/2019 Tour of Fuzhou CHN ME 2.1 [email protected] www.touroffz.com 03/12/2019 07/12/2019 Vuelta a Colombia Femenina COL WE 2.2 PRESIDENCIA@FED WWW.FEDERACI ERACIONCOLOMBIA ONCOLOMBIANA NADECICLISMO.COM DECICLISMO.COM 05/12/2019 08/12/2019 South East Asian Games PHI JR antolentino. -

Winner of the 2007 Tour De France, Alberto Contador, As Well As His Astana Teammates Levi Leipheimer, Winner of the 2008 Tour Of
INSIDE THE UCI/ASO CONFLICT ABOUT ORGANIZING CYCLING AS A SPORT: THE UNIBET CASE BENOIT HANSEZ INTRODUCTION Winner of the 2007 Tour de France, Alberto Contador, as well as his Astana teammates Levi Leipheimer, winner of the 2008 Tour of California and ranked third in the 2007 Tour de France, and Andreas Klöden, ranked second in the 2004 and 2006 Tours de France, have been denied participation in the 2008 Tour de France. This results from a decision of the Tour de France organizer, Amaury Sport Organisation (ASO), not to invite the cycling team Astana to the cycling races that it organizes in 2008, including the 2008 Tour de France. ASO’s decision is based on the damage caused by this team during the 2007 Tour de France and to cycling in general, both in 2006 and 2007.1 Prior to the start of the 2006 Tour de France, Astana was excluded from the Tour de France after five of its riders were implicated in a doping scandal. In the 2007 Tour de France, Astana pulled out of the Tour de France after its team leader Alexander Vinokourov tested positive for blood doping on July 24, 2007. Astana’s doping problem is a small piece of a long history of drugs scandals that have tarnished the credit of professional cycling over the last decade. Suffice to remember the highly media covered Festina affair in the 1998 Tour de France where the Festina physician Willy Voet was caught by border officials with large quantities of doping products in his Festina team car, and several members of the team, including the 1997 World Champion Laurent Brochard, were arrested and admitted to taking erythropoietin (EPO).2 Suffice also to cite the name of the famous Spanish doping case, Operación Puerto, against Dr. -

Belgium at a Glance
Belgium at a glance Belgium – a bird's eye view Belgium, a country of regions ................................................................ 5 A constitutional and hereditary monarchy .............................................6 A country full of creative talent ............................................................. 7 A dynamic economy ...............................................................................8 Treasure trove of contrasts ...................................................................8 Amazing history! ....................................................................................9 The advent of the state reform and two World Wars ........................... 10 Six state reforms ...................................................................................11 Working in Belgium An open economy .................................................................................13 Flexibility, quality and innovation ..........................................................13 A key logistics country ......................................................................... 14 Scientific research and education .........................................................15 Belgium – a way of life A gourmet experience ...........................................................................17 Fashion, too, is a Belgian tradition ...................................................... 18 Leading-edge design ............................................................................ 19 Folklore and traditions