Metabolism of Porphyrins and Bile Pigments
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Mitochondrial Transport of Protoporphyrinogen IX in Erythroid Cells
www.impactjournals.com/oncotarget/ Oncotarget, Vol. 6, No. 25 Editorial Mitochondrial transport of protoporphyrinogen IX in erythroid cells Yvette Y. Yien, Alessa R. Ringel and Barry H. Paw Comment on: Yien Y, et al. TMEM14C is required for erythroid mitochondrial heme metabolism. J. Clin. Invest. 2014; 124:4294-4304. Heme plays a vital role in essential processes factors, indicating the presence of extragenic modifiers of such as detoxification, oxygen transport, circadian the disease that participate in the heme synthesis pathway. rhythm, microRNA processing, respiration, regulation Among potential modifiers are the genes required for of transcription and translation, and apoptosis. The the transport of heme, heme intermediates and iron majority of heme in the body is synthesized in red blood (summarized in Figure 1). One such example is a loss-of- cells, whose function is to transport oxygen via the function mutation in MFRN1 (SLC25A37), the erythroid heme-containing oxygen carrier protein, hemoglobin. mitochondrial iron transporter, which exacerbated Defects in erythroid heme homeostasis can result in protoporphyrin IX accumulation due to a gain-of-function anemia, caused by the decrease in hemoglobin synthesis, C-terminal deletion in ALAS2 [2]. porphyria, caused by accumulation of photoreactive heme In an RNAseq screen for transporters of heme intermediates, and iron overload [1]. intermediates in terminally differentiating erythroid Heme synthesis requires the coordinated transport cells, we identified Tmem14c as a gene that is required of heme intermediates and iron within the cell and across for heme synthesis and erythropoiesis in zebrafish and membranes to provide substrates access to enzymes, mice [3]. TMEM14C is an inner mitochondrial membrane prevent intercalation of photo-reactive heme intermediates protein with three tightly packed transmembrane into cellular membranes, and minimize generation of helices, predictive of its function as a transporter [4]. -

Chapter 5 High-Pressure Stopped-Flow Kinetic Studies of Nnos
Probing the dynamics and conformational landscape of neuronal nitric oxide synthase A thesis submitted to the University of Manchester for the degree of Doctor of Philosophy in the Faculty of Life Sciences 2013 Anna Sobolewska-Stawiarz Contents Contents ...................................................................................................................... 2 List of Figures ............................................................................................................. 6 List of Tables ............................................................................................................ 10 Abstract ..................................................................................................................... 12 Declaration ................................................................................................................ 13 Copyright Statement ................................................................................................ 13 Acknowledgements ................................................................................................... 14 List of Abbreviations ............................................................................................... 15 List of Amino Acids Abbreviations ........................................................................ 17 CHAPTER 1. INTRODUCTION ........................................................................... 18 1.1 Nitric oxide synthase ......................................................................................... -

Hyperbilirubinemia
Porphyrins Porphyrins (Porphins) are cyclic tetrapyrol compounds formed by the linkage )). of four pyrrole rings through methenyl bridges (( HC In the reduced porphyrins (Porphyrinogens) the linkage of four pyrrole rings (tetrapyrol) through methylene bridges (( CH2 )) The characteristic property of porphyrins is the formation of complexes with the metal ion bound to nitrogen atoms of the pyrrole rings. e.g. Heme (iron porphyrin). Proteins which contain heme ((hemoproteins)) are widely distributed e.g. Hemoglobin, Myoglobin, Cytochromes, Catalase & Tryptophan pyrrolase. Natural porphyrins have substituent side chains on the eight hydrogen atoms numbered on the pyrrole rings. These side chains are: CH 1-Methyl-group (M)… (( 3 )) 2-Acetate-group (A)… (( CH2COOH )) 3-Propionate-group (P)… (( CH2CH2COOH )) 4-Vinyl-group (V)… (( CH CH2 )) Porphyrins with asymmetric arrangement of the side chains are classified as type III porphyrins while those with symmetric arrangement of the side chains are classified as type I porphyrins. Only types I & III are present in nature & type III series is more important because it includes heme. 1 Heme Biosynthesis Heme biosynthesis occurs through the following steps: 1-The starting reaction is the condensation between succinyl-CoA ((derived from citric acid cycle in the mitochondria)) & glycine, this reaction is a rate limiting reaction in the hepatic heme synthesis, it occurs in the mitochondria & is catalyzed by ALA synthase (Aminolevulinate synthase) enzyme in the presence of pyridoxal phosphate as a cofactor. The product of this reaction is α-amino-β-ketoadipate which is rapidly decarboxylated to form δ-aminolevulinate (ALA). 2-In the cytoplasm condensation reaction between two molecules of ALA is catalyzed by ALA dehydratase enzyme to form two molecules of water & one 2 molecule of porphobilinogen (PBG) which is a precursor of pyrrole. -

Porphyrins & Bile Pigments
Bio. 2. ASPU. Lectu.6. Prof. Dr. F. ALQuobaili Porphyrins & Bile Pigments • Biomedical Importance These topics are closely related, because heme is synthesized from porphyrins and iron, and the products of degradation of heme are the bile pigments and iron. Knowledge of the biochemistry of the porphyrins and of heme is basic to understanding the varied functions of hemoproteins in the body. The porphyrias are a group of diseases caused by abnormalities in the pathway of biosynthesis of the various porphyrins. A much more prevalent clinical condition is jaundice, due to elevation of bilirubin in the plasma, due to overproduction of bilirubin or to failure of its excretion and is seen in numerous diseases ranging from hemolytic anemias to viral hepatitis and to cancer of the pancreas. • Metalloporphyrins & Hemoproteins Are Important in Nature Porphyrins are cyclic compounds formed by the linkage of four pyrrole rings through methyne (==HC—) bridges. A characteristic property of the porphyrins is the formation of complexes with metal ions bound to the nitrogen atom of the pyrrole rings. Examples are the iron porphyrins such as heme of hemoglobin and the magnesium‐containing porphyrin chlorophyll, the photosynthetic pigment of plants. • Natural Porphyrins Have Substituent Side Chains on the Porphin Nucleus The porphyrins found in nature are compounds in which various side chains are substituted for the eight hydrogen atoms numbered in the porphyrin nucleus. As a simple means of showing these substitutions, Fischer proposed a shorthand formula in which the methyne bridges are omitted and a porphyrin with this type of asymmetric substitution is classified as a type III porphyrin. -

Noncanonical Coproporphyrin-Dependent Bacterial Heme Biosynthesis Pathway That Does Not Use Protoporphyrin
Noncanonical coproporphyrin-dependent bacterial heme biosynthesis pathway that does not use protoporphyrin Harry A. Daileya,b,c,1, Svetlana Gerdesd, Tamara A. Daileya,b,c, Joseph S. Burcha, and John D. Phillipse aBiomedical and Health Sciences Institute and Departments of bMicrobiology and cBiochemistry and Molecular Biology, University of Georgia, Athens, GA 30602; dMathematics and Computer Science Division, Argonne National Laboratory, Argonne, IL 60439; and eDivision of Hematology, Department of Medicine, University of Utah School of Medicine, Salt Lake City, UT 84132 Edited by J. Clark Lagarias, University of California, Davis, CA, and approved January 12, 2015 (received for review August 25, 2014) It has been generally accepted that biosynthesis of protoheme of a “primitive” pathway in Desulfovibrio vulgaris (13). This path- (heme) uses a common set of core metabolic intermediates that way, named the “alternative heme biosynthesis” path (or ahb), has includes protoporphyrin. Herein, we show that the Actinobacteria now been characterized by Warren and coworkers (15) in sulfate- and Firmicutes (high-GC and low-GC Gram-positive bacteria) are reducing bacteria. In the ahb pathway, siroheme, synthesized unable to synthesize protoporphyrin. Instead, they oxidize copro- from uroporphyrinogen III, can be further metabolized by suc- porphyrinogen to coproporphyrin, insert ferrous iron to make Fe- cessive demethylation and decarboxylation to yield protoheme (14, coproporphyrin (coproheme), and then decarboxylate coproheme 15) (Fig. 1 and Fig. S1). A similar pathway exists for protoheme- to generate protoheme. This pathway is specified by three genes containing archaea (15, 16). named hemY, hemH, and hemQ. The analysis of 982 representa- Current gene annotations suggest that all enzymes for pro- tive prokaryotic genomes is consistent with this pathway being karyotic heme synthetic pathways are now identified. -
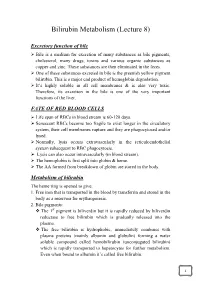
Bilirubin Metabolism (Lecture 8)
Bilirubin Metabolism (Lecture 8) Excretory function of bile Bile is a medium for excretion of many substances as bile pigments, cholesterol, many drugs, toxins and various organic substances as copper and zinc. These substances are then eliminated in the feces. One of these substances excreted in bile is the greenish yellow pigment bilirubin. This is a major end product of hemoglobin degradation. It’s highly soluble in all cell membranes & is also very toxic. Therefore, its excretion in the bile is one of the very important functions of the liver. FATE OF RED BLOOD CELLS Life span of RBCs in blood stream is 60-120 days. Senescent RBCs become too fragile to exist longer in the circulatory system, their cell membranes rupture and they are phagocytosed and/or lysed. Normally, lysis occurs extravascularly in the reticuloendothelial system subsequent to RBC phagocytosis. Lysis can also occur intravascularly (in blood stream). The hemoglobin is first split into globin & heme. The AA formed from breakdown of globin are stored in the body. Metabolism of bilirubin The heme ring is opened to give: 1. Free iron that is transported in the blood by transferrin and stored in the body as a reservoir for erythropoiesis. 2. Bile pigments: The 1st pigment is biliverdin but it is rapidly reduced by biliverdin reductase to free bilirubin which is gradually released into the plasma. The free bilirubin is hydrophobic, immediately combines with plasma proteins (mainly albumin and globulin) forming a water soluble compound called hemobilirubin (unconjugated bilirubin) which is rapidly transported to hepatocytes for further metabolism. Even when bound to albumin it’s called free bilirubin. -

Biochemistry I Enzymes
BIOCHEMISTRY I 3rd. Stage Lec. ENZYMES Biomedical Importance: Enzymes, which catalyze the biochemical reactions, are essential for life. They participate in the breakdown of nutrients to supply energy and chemical building blocks; the assembly of those building blocks into proteins, DNA, membranes, cells, and tissues; and the harnessing of energy to power cell motility, neural function, and muscle contraction. The vast majority of enzymes are proteins. Notable exceptions include ribosomal RNAs and a handful of RNA molecules imbued with endonuclease or nucleotide ligase activity known collectively as ribozymes. The ability to detect and to quantify the activity of specific enzymes in blood, other tissue fluids, or cell extracts provides information that complements the physician’s ability to diagnose and predict the prognosis of many diseases. Further medical applications include changes in the quantity or in the catalytic activity of key enzymes that can result from genetic defects, nutritional deficits, tissue damage, toxins, or infection by viral or bacterial pathogens (eg, Vibrio cholerae). Medical scientists address imbalances in enzyme activity by using pharmacologic agents to inhibit specific enzymes and are investigating gene therapy as a means to remedy deficits in enzyme level or function. In addition to serving as the catalysts for all metabolic processes, their impressive catalytic activity, substrate specificity, and stereospecificity enable enzymes to fulfill key roles in additional processes related to human health and well-being. Proteases and amylases augment the capacity of detergents to remove dirt and stains, and enzymes play important roles in producing or enhancing the nutrient value of food products for both humans and animals. -
NEONATAL Hb, O2-TRANSPORT & JAUNDICE: OVERVIEW
BILIRUBIN METABOLISM & JAUNDICE UNIVERSITY OF PNG SCHOOL OF MEDICINE AND HEALTH SCIENCES DISCIPLINE OF BIOCHEMISTRY & MOLECULAR BIOLOGY PBL MBBS II SEMINAR VJ Temple 1 Brief description of Hemoglobin (Hb) structure • Hemoglobin (Hb): Made up of 4-Subunits (Tetramer) held together by multiple non-covalent interactions; • Each subunit consist of: • Heme (Ferro-Protoporphyrin), • Globin protein; • Heme: Protoporphyrin IX and Ferrous ion (Fe2); • Globin protein folds around Heme group forming a protective Hydrophobic pocket; • Heme is the site of Oxygen binding; 2 • There are different types of Hemoglobin, with different subunits: • Foetal Hemoglobin (Hb F): 2 2 Two types of Adult Hemoglobin (Hb A): • Hb A1 represented as: 2 2 • It is the major (98%) form of Hb in adults; • Hb A2 represented as: 2 2 • It is the minor (2%) form of Hb in adults; 3 What are the major sources of Heme in humans? • RBC is major source of Heme in humans, • Life span of RBC is about 120 days, • Other sources of Heme include: • Myoglobin (Mb): Stores Oxygen in muscle cells, • Cytochromes: present in some enzymes, • Catalase: an enzyme, 4 What normally happens to RBC after 120 days? • RBC is destroyed mainly in Reticuloendothelial system (Extra-vascular system: Spleen and Liver); • Daily turnover of Hb is about 6 g/day; • Hb is broken down, • Globin protein is hydrolyzed to amino acids, • Protoporphyrin Ring in Heme is Hydrophobic, thus must be made soluble before it is excreted, • Ferrous ion is removed and stored in Iron pool, for reuse, • Protoporphyrin ring is metabolized -

Design and Fine-Tuning Redox Potentials of Metalloproteins Involved in Electron Transfer in Bioenergetics
1 Design and Fine-tuning Redox Potentials of Metalloproteins Involved in Electron Transfer in Bioenergetics Parisa Hosseinzadeh and Yi Lu Abstract: 1. Introduction A significant portion of biological processes are involved with providing vital energy sources such as ATP, and controlling the flow of energy through living systems. These bioenergetics processes, the most important of which are photosynthesis and respiration, require electron transfer (ET) between different redox partners. Metalloproteins are one of the most widely used ET centers in biology. They can be classified into three major classes: cupredoxins, which include type 1 copper (T1Cu) proteins and CuA centers [1- 10], cytochromes [10-17], and iron-sulfur (FeS) proteins [10,18-24]. Each class of ET proteins transfer electrons between different redox partners which possess different reduction potentials (E°) (Figure 1). Therefore, the ET centers need to adjust their E° in a way that matches those of their redox partners. No single class of protein can cover the entire range of physiological E°, which is between ~ -1V, at which protons are reduced to H2, and 1V, at which water is oxidized to O2. Cupredoxins usually function at the high end of the E°, while FeS proteins are mostly involved in ET reactions possessing relatively low E° [10]. The E°’s of FeS proteins overlap significantly with those of cytochromes that often have intermediate E° among the three classes of ET proteins. Figure 1. Reduction potential range of metal centers in electron transfer metalloprotein. Adapted from ref. [10] 2 In this review, we first describe the importance of tuning E° of ET centers, including the metalloproteins described above. -

The Function of Pufq in the Regulation of Bacteriochlorophyll Biosynthesis in Rhodobacter Capsulatus
The Function of PufQ in the Regulation of Bacteriochlorophyll Biosynthesis in Rhodobacter capsulatus Himani Rajeshwar Utkhede B.Sc. Simon Fraser University, 200 1 THESIS SUBMITTED IN PARTIAL FULFILLMENT OF THE REQUIREMENTS OF THE DEGREE OF MASTER OF SCIENCE in the Department of Molecular Biology and Biochemistry O Himani R. Utkhede 2004 SIMON FRASER UNIVERSITY March, 2004 All rights reserved. This work may not be reproduced in whole or in part, by photocopy or other means, without permission of the author. Approval I Name: Himani R. Utkhede Degree: Master of Science Title of Thesis: The Function of PufQ in the Regulation of Bacteriochlorophyll Synthesis in Rhodobacter capsulatus. Examining Committee: Dr. W.S. Davidson, Chair Dr. William R. Richards, Senior Supervisor Professor Emeritus, Molecular Biology and Biochemistry Simon Fraser University Dr. Michel Leroux, Supervisor Assistzt Prcfessor, ?v!s!ec.dzr Eic!ca.;- - 2~2L3.icche~isty Simon Fraser University Dr. Erika Plettner, Supervisor Assistant Professor, Chemistry Simon Fraser University Dr. Lynne Quarmby, Internal Examiner Assistant Professor, Biology Simon Fraser University Date Approved: Partial Copyright Licence The author, whose copyright is declared on the title page of this work, has granted to Simon Fraser University the right to lend this thesis, project or extended essay to users of the Simon Fraser University Library, and to make partial or single copies only for such users or in response to a request from the library of any other university, or other educational institution, on its own behalf or for one of its users. The author has further agreed that permission for multiple copying of ths work for scholarly purposes may be granted by either the author or the Dean of Graduate Studies. -
Bilirubin PDF 12Days
Bilirubin Physiology – WYNTKFTB • Bilirubin metabolism – Unconjugated – Conjugation – Excretion • Enterohepatic circulation • Implication of bilirubin metabolism – Urine – Stool • Understand the metabolic pathway as related to the disease state of JAUNDICE Don’t make me come up there and steal your google machines! BR - Alb Thank you. BG the Bilirubin an overview by howard sachs Slo-Motion Instant Replay… Heme oxygenase Biliverdin Reductase Heme oxygenase Biliverdin Reductase Bilirubin Albumin (unconjugated) …not water soluble… Unconjugated Bilirubin (‘Indirect’) Key points: • ‘Attached to albumin’: too big to pass through glomerular filtration barrier. • Intravascular: Hemoglobin ® urine • Unconjugated: not water soluble. How can we get too much unconjugated bilirubin in the serum? 1. Hemolysis • Elevated indirect bilirubin is used as a diagnostic marker (with LDH, ¯ haptoglobin) 2. Conjugation defect: inherited (Gilbert’s, Crigler-Najjar) Multidrug resistance associated protein Bilirubin binds to cytosolic binding protein, glutathione s-transferase (GST) for transport to ER Conjugation of bilirubin is catalyzed by bilirubin-uridinediphosphate (UDP)- glucuronosyltransferase (UGT1A1). Product is bilirubin diglucuronide. UDPGA is the donor sugar Multidrug resistance Endoplasmic reticulum associated protein Bilirubin diglucuronide Conjugated (direct) Bilirubin binds to cytosolic binding protein, glutathione s-transferase (GST) for transport to ER Conjugation of bilirubin is catalyzed by bilirubin-uridinediphosphate (UDP)- glucuronosyltransferase -
Characterisation, Classification and Conformational Variability Of
Characterisation, Classification and Conformational Variability of Organic Enzyme Cofactors Julia D. Fischer European Bioinformatics Institute Clare Hall College University of Cambridge A thesis submitted for the degree of Doctor of Philosophy 11 April 2011 This dissertation is the result of my own work and includes nothing which is the outcome of work done in collaboration except where specifically indicated in the text. This dissertation does not exceed the word limit of 60,000 words. Acknowledgements I would like to thank all the members of the Thornton research group for their constant interest in my work, their continuous willingness to answer my academic questions, and for their company during my time at the EBI. This includes Saumya Kumar, Sergio Martinez Cuesta, Matthias Ziehm, Dr. Daniela Wieser, Dr. Xun Li, Dr. Irene Pa- patheodorou, Dr. Pedro Ballester, Dr. Abdullah Kahraman, Dr. Rafael Najmanovich, Dr. Tjaart de Beer, Dr. Syed Asad Rahman, Dr. Nicholas Furnham, Dr. Roman Laskowski and Dr. Gemma Holli- day. Special thanks to Asad for allowing me to use early development versions of his SMSD software and for help and advice with the KEGG API installation, to Roman for knowing where to find all kinds of data, to Dani for help with R scripts, to Nick for letting me use his E.C. tree program, to Tjaart for python advice and especially to Gemma for her constant advice and feedback on my work in all aspects, in particular the chemistry side. Most importantly, I would like to thank Prof. Janet Thornton for giving me the chance to work on this project, for all the time she spent in meetings with me and reading my work, for sharing her seemingly limitless knowledge and enthusiasm about the fascinating world of enzymes, and for being such an experienced and motivational advisor.