2020 Integrated Atlas of Mental Health Care of the Australian Capital Territory
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Tuggeranong United Football Club-Junior Manual 2019
1 | Page Tuggeranong United Football Club 2019 JUNIORS TEAM MANUAL For Managers and Coaches (as at February 2019) Tuggeranong United Football Club is an incorporated community organisation registered under the Associations Incorporations Act. A copy of the Club’s Constitution is available from the Club on request. TUFC colours are bottle green, gold and white. TUFC is an affiliate of Capital Football, which has responsibility for organising football (soccer) in the ACT, under the authority of the Football Federation of Australia (FFA) and FIFA, the international body. The Juniors teams and competition are based at the Wanniassa playing fields, Hyland Place. 1 | Page 2 | Page TABLE OF CONTENTS Introduction 4 Role of the Manager in Brief 4 Role of the Coach in Brief 4 Section 1 – General information 5 Spectators 7 Member Protection 7 Gear 8 Training 9 Match Days 10 Pitch Dressing 12 Referees 12 Section 2 - Miniroos – U5 to U9 14 Beginning of the season 14 Draws and Grounds 14 Gear 14 Training 14 Match Days 15 Pitch Dressing 15 End of Season 15 2 | Page 3 | Page Section 3 - Small Sided Football – U10 to U11 16 Beginning of the season 16 Draws and Grounds 16 Gear 17 Training 17 Match Days 17 Pitch Dressing 19 End of Season 19 Section 4 - Youth Football – U12 to U18 20 Beginning of Season 20 Draws and Grounds 20 Gear 21 Training 21 Match Days 21 Match Cards 23 Pitch Dressing 25 End of Season 25 Section 5 - Fundraising and Tournaments 27 Volunteers Always Welcome 27 3 | Page 4 | Page INTRODUCTION: Thank you for volunteering as a team official. -

3. Planning and Legislation
Capital Metro Authority Capital Metro Russell Extension Project - Preliminary Environmental Assessment 3. Planning and legislation 3.1 Overview The planning approvals process for the Project would comprise a mix of both Territory and Commonwealth requirements as the Project corridor falls under the administrative authority of both the National Capital Authority (NCA) and the ACT Government through the Environment and Planning Directorate (EPD). The authority jurisdictions of the NCA and EPD are discussed in section 3.2 below. This Chapter provides an overview of the applicable planning and approvals process that the Russell Extension Project would be required to follow to gain approval. 3.1.1 Approach to planning approvals for the Russell Extension Project As noted above, the Russell Extension Project would be undertaken as Stage 2 of the proposed Civic to Gungahlin Project (Stage 1). An Environmental Impact Statement for the Stage 1 Civic to Gungahlin Project and is currently (as at September 2015) being determined by EPS. As such, the Russell Extension Project environment and planning approvals are being progressed separately to the Stage 1 planning approvals. This approach has the following key implications to the Russell Extension Project: the Environmental Impact Statement (EIS) currently being prepared for the Stage 1 Civic to Gungahlin Project under the ACT Planning & Development Act 2007 (P&D Act) does not address the Russell Extension Project the Stage 1 Gungahlin to Civic Development Application to be submitted to the ACT Government -

Minutes of Public Meeting
Minutes of Public Meeting 7 pm Wednesday 3 April 2019 Canberra Southern Cross Club Estimated attendance: Fifty five 1 Welcome: President, Fiona Carrick, welcomed and thanked attendees. MLAs in attendance: Mr Alistair Coe, Leader of the ACT Liberal Party Ms Caroline Le Couteur 2 Minutes of the last meeting held on 6 March 2019 - Not Discussed. 3 Chair Report: Our presenters will explain to us who does what with respect to urban renewal Clarification of misconceptions: the WVCC is not anti-development - we want development to be done well, with the needs of the community at the forefront of planning, including planning for public spaces and community facilities. If we had a plan we could stage development of community facilities A recent media article said that there are people who talk down developments. While we may have a view about some of the developments in Woden - o the WVCC does not talk Woden down o Woden is our home and we want the best outcomes for our community The Woden Experiment – the Town Square is looking great with people stopping and using the nature play and the table tennis table We need active fronts around the square – eg cafes, pubs and book stalls A reminder of the original planning for Woden included the east west community link, what happened to it? The Woden Town Centre Master Plan includes a map of opportunities which includes the east west link. What are the opportunities to re-instate the link and make it better? The zoning provides for 28 storeys around the perimeter of the Town Square which allows 3 hours of sunlight on a quarter of the square in the winter solstice. -
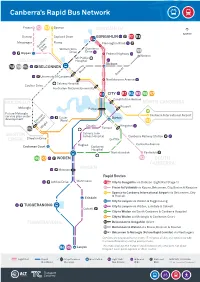
Canberra's Rapid Bus Network
Canberra’s Rapid Bus Network Fraser R2 R3 Spence GUNGAHLIN NORTH Dunlop Copland Drive GUNGAHLIN R1 R8 Macgregor Florey Flemington Road Southern Cross William Slim Gundaroo Drive Drive Drive R9 Kippax Federal Highway Watson UC Public BELCONNEN Hospital Dickson R8 R9 FRC BELCONNEN Bruce Downer University of Canberra Northbourne Avenue Calvary Hospital Coulter Drive Australian National University CITY R1 R4 R5 R6 R7 Constitution Avenue MOLONGLO NORTH CANBERRA Russell Molonglo Parkes Future Molonglo Canberra International Airport service plan under Cotter Barton development Road Denman R3 Prospect Deakin Kingston FRC Wright Forrest Calvary John WESTON James Hospital Canberra Railway Station CREEK Streeton Drive Grifth Hughes Canberra Avenue Cooleman Court Canberra Hospital Narrabundah Fyshwick R6 R7 WODEN R2 SOUTH CANBERRA Mawson WODEN Rapid Routes Wanniassa Athllon Drive R1 City to Gungahlin via Dickson (Light Rail Stage 1) R2 Fraser to Fyshwick via Kippax, Belconnen, City, Barton & Kingston R3 Spence to Canberra International Airport via Belconnen, City & Russell Erindale R4 City to Lanyon via Woden & Tuggeranong TUGGERANONG R5 City to Lanyon via Woden, Erindale & Calwell Calwell R6 City to Woden via South Canberra & Canberra Hospital R7 City to Woden via Molonglo & Cooleman Court TUGGERANONG R8 Belconnen to Gungahlin direct R9 Belconnen to Watson via Bruce, Dickson & Downer FRC Belconnen to Molonglo (Future Rapid Corridor) via Weetangera Services are proposed to run every 15 minutes all day and weekends with increased frequency during peak periods. Lanyon This map displays the Future Rapid Network only and does not show R4 R5 frequent local, peak express or other routes. Light Rail Rapid Stop/Common Bus Station Light Rail/ Bike and Park and MAP NOT TO SCALE Bus Route Bus stop Bus Station Ride Ride TG17443 - last updated 18 October 2017. -

Woden Interchange Platform Changes Platform Numbers and Departures Are Changing from 6 July 2019
WodenWoden Interchange Interchange - Departure Platform platforms Changes Platform numbers and departures are changing from 6 July 2019 Bowes St Callam St Exit Bowes St Bowes St To PARLIAMENT HOUSE & City via… 57 Garran, Hughes, Yarralumla & Deakin NORTH 58 Curtin, Hughes & Deakin R5 To City via Barton & Russell To Mawson / Woden via… 7 Stop Bowes Pl O’Malley, Isaacs & Farrer (clockwise loop) 2710 60 Stop 61 Mawson, Farrer, Isaacs & O’Malley (anticlockwise loop) 2712 8 62 Lyons, Chiey, Pearce & Torrens R4 To Cooleman Court via… To Cooleman Court DIRECT then… 6 Stop To City DIRECT 63 Waramanga, Fisher & Stirling 64 Rivett, Stirling & Chapman 2709 66 Weston, Coombs, Denman Prospect, Wright & Duffy 65 Holder & Duffy Stop Stop 2814 2815 Stop 9 R6 2716 10 To City via CANBERRA HOSPITAL, 11 4 Narrabundah, Manuka, Kingston, 5 Stop Woden 3 Stop 2908 Barton & Parkes Exit Youth Woden Town Square 2706 Callam St 2 Stop Centre 1 Stop 2705 Stop 2804 R4 School services 2703 To Tuggeranong DIRECT Qcity Transit, Transborder Express R5 To Cooleman Court DIRECT then… To Lanyon Marketplace Exit Callam St 70 Kambah West & Tuggeranong via Erindale & Calwell 71 Kambah East & Tuggeranong Westeld Bradley St Woden Exit Westeld Woden ACT Police 3 Bus platform number 57 Route number Park and Ride Lift School service platform R4 route number Information display Stairs transport.act.gov.au CANBERRA transport.act.gov.au IS BETTER CONNECTED Woden Interchange Platform Changes Platform numbers and departures are changing from 6 July 2019 • Transport Canberra is making improvements to the Woden Interchange, commencing from Saturday 6 July 2019. -
Access UC by TC TC Bike & Bike Racks
Effective Local bus routes Check the instructions for on-bus 27 January 2020 Access UC by TC TC Bike & bike racks. public transport Light Rail Buses Local bus services that are designed to get students to their Ride If travelling on light rail, you can town centre and other destinations wheel your bike onboard and place in their area, such as schools or Transport Canberra buses operate it on one of the four bike racks at Access Transport Canberra provides a Transport Canberra’s Light Rail local shops. All local routes The ACT is a great city for walking 7 days a week across the whole of either end of the vehicle. wide range of bus and light rail route R1 runs from the City to connect with at least two RAPID and cycling, with hundreds of Canberra. A map showing buses options for travel to the University Gungahlin, along Northbourne routes to help for customers kilometres of shared off-road You can also store your bike at one around the UC campus and where of Canberra (UC). Avenue and Flemington Road. making longer journeys. Local paths, a moderate climate, of many bike lockers, cages or racks buses operate to is shown overleaf. relatively at terrain, and an across Canberra and then hop on a There are also extensive options Light rail is fully integrated with routes generally run every 20 to There are three types of bus extensive trail network in our bus or light rail vehicle. You will need for riding and storing your bike the bus ticketing system (same 30 minutes in peak times, and at service types called RAPIDs, Local nature parks. -

Belconnen District Precinct Map and Code
Belconnen District Precinct Map and Code NI2008-27 10.2 District Precinct Maps and Codes Effective: 4 October 2013 Authorised by the ACT Parliamentary Counsel—also accessible at www.legislation.act.gov.au This page is intentionally blank. 10.2 District Precinct Maps and Codes NI2008-27 Effective: 4 October 2013 Authorised by the ACT Parliamentary Counsel—also accessible at www.legislation.act.gov.au NI2008-27 page 1 10.2 District Precinct Maps and Codes Belconnen Precinct Map and Code Effective: 4 October 2013 Authorised by the ACT Parliamentary Counsel—also accessible at www.legislation.act.gov.au Assessment Tracks The following tables identify the additional prohibited development and additional merit track development for blocks and parcels shown in the Belconnen District Precinct Map (identified as PDn or MTn). Development that is exempt from requiring development approval, other prohibited development and the minimum assessment track applicable to each development proposal is set out in the relevant zone development table. The following tables constitute part of the relevant zone development table. Table 1 – Additional prohibited development Additional prohibited development Suburb precinct map label Zone Development NUZ3 ancillary RESIDENTIAL USE PD1 NUZ4 outdoor recreation facility PD2 NUZ4 ancillary RESIDENTIAL USE Table 2 – Additional merit track development Additional merit track development that may be approved subject to assessment Suburb precinct map label Zone Development MT1 NUZ4 treatment plant landfill site MT2 NUZ3 recycling facility recyclable materials collection page 2 NI2008-27 10.2 Districts Precinct Maps and Codes Belconnen Precinct Map and Code Effective: 4 October 2013 Authorised by the ACT Parliamentary Counsel—also accessible at www.legislation.act.gov.au Belconnen District Precinct Code Contents Introduction ........................................................................................................................................... -

Transport Planning and Policy Team Transport Canberra [email protected]
Transport Planning and Policy Team Transport Canberra [email protected] Dear Sir/Madam Woden Valley Community Council’s Submission to the Moving Canberra 2019-2045 - Integrated Transport Strategy (Strategy). The Woden Valley Community Council (WVCC) appreciates the opportunity to provide this submission about the Integrated Transport Strategy. We acknowledge that population growth and the environmental impacts of urban sprawl are creating the need to densify the City and Town Centres. We welcome development but want it to be done well, with the needs of the community at the forefront of planning. The Woden Town Centre is centrally located and accessible making it an ideal location for the provision of jobs, services and facilities for the growing community. While many residents will need to travel to other employment hubs, the current requirement to travel to other districts for cultural and indoor recreational activities encourages car ownership and adds to congestion on our roads. As mentioned in the Strategy, our city is not static and a land use plan is required to guide public and private sector investment as the Woden Town Centre grows. This includes planning for a community centre, indoor multi-purpose sports hall, aquatic centre and higher education to diversify Woden’s economy. Planning for an active Centre provides confidence for the private sector to invest and reduces the reliance on car trips to other districts. Public transport, including the suburban routes, should provide access to our Town Centres, Group Centres and local shops to strengthen connections between people, enabling them to share public spaces, cultural and recreational facilities to build strong and resilient communities. -

Queanbeyan Local Environmental Plan 2012 Under the Environmental Planning and Assessment Act 1979
2012 No 576 New South Wales Queanbeyan Local Environmental Plan 2012 under the Environmental Planning and Assessment Act 1979 I, the Minister for Planning and Infrastructure, pursuant to section 33A of the Environmental Planning and Assessment Act 1979, adopt the mandatory provisions of the Standard Instrument (Local Environmental Plans) Order 2006 and prescribe matters required or permitted by that Order so as to make a local environmental plan as follows. SAM HADDAD As delegate for the Minister for Planning and Infrastructure Published LW 23 November 2012 Page 1 2012 No 576 Queanbeyan Local Environmental Plan 2012 Contents Page Part 1 Preliminary 1.1 Name of Plan 5 1.1AA Commencement 5 1.2 Aims of Plan 5 1.3 Land to which Plan applies 6 1.4 Definitions 6 1.5 Notes 6 1.6 Consent authority 6 1.7 Maps 6 1.8 Repeal of planning instruments applying to land 7 1.8A Savings provision relating to development applications 7 1.9 Application of SEPPs 7 1.9A Suspension of covenants, agreements and instruments 8 Part 2 Permitted or prohibited development 2.1 Land use zones 9 2.2 Zoning of land to which Plan applies 10 2.3 Zone objectives and Land Use Table 10 2.4 Unzoned land 10 2.5 Additional permitted uses for particular land 11 2.6 Subdivision—consent requirements 11 2.7 Demolition requires development consent 11 2.8 Temporary use of land 12 Land Use Table Part 3 Exempt and complying development 3.1 Exempt development 29 3.2 Complying development 30 3.3 Environmentally sensitive areas excluded 31 Part 4 Principal development standards 4.1 Minimum -
Queanbeyan Comprehensive Development Control Plan 2012
Queanbeyan Comprehensive Development Control Plan 2012 Queanbeyan-Palerang Regional Council ECM 668356 Comprehensive Development Control Plan 2012 Combined Table of Contents 1 Queanbeyan Development Control Plan 2012 Part 1 About this Development Control Plan 1.1 Introduction 1.2 Purpose of this DCP 1.3 Statutory Context 1.3.1 Title 1.3.2 Status 1.3.3 Relevant Local Environmental Plan 1.3.4 Relationship with any Environmental Planning Instrument (EPI) 1.3.5 Relationship to Other Plans, Policies and the Like 1.3.6 Commencement 1.3.7 Previous Development Control Plans 1.3.8 Where the DCP Applies 1.4 How the DCP Applies To Development 1.4.1 Development that Needs Consent 1.4.2 Development That Does Not Need Consent 1.4.3 Variation to this DCP 1.5 Contents of the DCP 1.5.1 DCP Structure 1.6 How to use this Development Control Plan 1.7 Information required for a Development Application 1.7.1 Development Application Form 1.7.2 Information Required for the Lodgement of a Development Application 1.7.3 Supplementary Information which may be required with Your Development Application 1.7.4 Site Analysis Plan 1.7.5 Erosion and Sediment Control Pan (ESCP) 1.7.6 Construction Certificate 1.8 Public Notification of a Development Application 1.9 Fees and Contributions Part 2 All Zones 2.1. Introduction 2.1.1 Purpose of This Part 2.1.2 Objectives 2.1.3 Relationship to Other Plans 2.2. Car Parking 2.2.1 Introduction 2.2.2 Objectives for Car Parking 2.2.3 General Principles 2.2.4 Variations and Compliance 2 Queanbeyan Development Control Plan 2012 2.2.5 -

Queanbeyan Sewage Treatment Plant Upgrade
Queanbeyan-Palerang Regional Council October 2020 | Draft Queanbeyan Sewage Treatment Plant Upgrade Environmental Impact Statement Clear waters for future generations Queanbeyan-Palerang Regional Council EIS | Cover page Draft EIS Cover Page Cover page as per Scoping Document requirements: Requirement Detail Name of proposal Queanbeyan Sewage Treatment Plant (STP) Upgrade Block: 27 Section: Block identifier and 0 street address for the proposal District/division: Jerrabomberra Street address: 7 Mountain Road, Jerrabomberra, ACT Date of preparation 30 October 2020 of this document Full name and Queanbeyan-Palerang Regional Council (QPRC) postal address of PO Box 90 the proponent Queanbeyan NSW 2620 Full name and Queanbeyan-Palerang Regional Council (QPRC) postal address of PO Box 90 the applicant Queanbeyan NSW 2620 Arup Australia Pty Ltd Level 4 10 Moore Street Name and contact Canberra ACT 2601 details of the (02) 6191 7700 person/organisation who prepared the Joyanne Manning documents BE M.EngSc CPEng EngExec Fiona Riley BA (AncHist) PGCert (EnvMgmt) Arup Volume 1 Clear waters for future generations Contents – Volume 1 Glossary and Abbreviations Executive Summary 1 Introduction 1 1.1 Background 3 1.2 Purpose and structure of this report 5 2 Proposal details 7 2.1 Proposal location, land uses and existing sewage 7 treatment plant 2.2 Proposal objectives and justification 15 2.3 Proposal overview 16 2.4 Proposal timeframe 30 2.5 Construction activities 30 3 Legislative and strategic context 37 3.1 Planning and Development Act 2007 37 3.2 -

Comprehensive Development Control Plan 2012 Combined Table of Contents
Comprehensive Development Control Plan 2012 Combined Table of Contents C1292517 1 Queanbeyan Development Control Plan 2012 Part 1 About this Development Control Plan 1.1 Introduction 1.2 Purpose of this DCP 1.3 Statutory Context 1.3.1 Title 1.3.2 Status 1.3.3 Relevant Local Environmental Plan 1.3.4 Relationship with any Environmental Planning Instrument (EPI) 1.3.5 Relationship to Other Plans, Policies and the Like 1.3.6 Commencement 1.3.7 Previous Development Control Plans 1.3.8 Where the DCP Applies 1.4 How the DCP Applies To Development 1.4.1 Development that Needs Consent 1.4.2 Development That Does Not Need Consent 1.4.3 Variation to this DCP 1.5 Contents of the DCP 1.5.1 DCP Structure 1.6 How to use this Development Control Plan 1.7 Information required for a Development Application 1.7.1 Development Application Form 1.7.2 Information Required for the Lodgement of a Development Application 1.7.3 Supplementary Information which may be Required with Your Development Application 1.7.4 Information Required for State Environmental Planning Policy No 65 Development 1.7.5 Construction Certificate 1.8 Public Notification of a Development Application 1.8.1 Notification and Advertising of Applications and Notification Period 1.8.2 Notification on Council’s Website 1.8.3 Notice in Newspaper 1.8.4 Notifying an Amendment to a Development Application Prior to Determination 1.8.5 Notification Requirements for Modifications 1.8.6 Persons to be Notified by Letter 1.8.7 Notification Area 1.8.8 Notification to the Owners 1.8.9 Deadline for Council to Receive Submissions 1.8.10 Extension of Notification Period 1.8.11 Late Submissions 1.8.12 Submissions to be made Public Documents 1.8.13 Consideration of Submissions 1.8.14 Determination Process Where Submissions are Lodged 1.8.15 Notification of Council’s Determination C1292517 2 Queanbeyan Development Control Plan 2012 Part 2 All Zones 2.1.