Annual Report 2019-20
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Imperialmatters31.Pdf
Imperial Matters 31 QX 6/2/08 08:26 Page 37 head ISSUE 31 WINTER 2007–08_THE UK’S NEW KIND OF HEALTHCARE CENTRE_LOOKING BACK AT A YEAR OF CELEBRATIONS_AN EVENING OF ROCK AND DUST_PLUS ALL THE NEWS FROM THE COLLEGE AND ALUMNI GROUPS IMPERIALmatters Alumni magazine of Imperial College London including the former Charing Cross and Westminster Medical School, Royal Postgraduate Medical School, St Mary’s Hospital Medical School and Wye College. ISSUE 31 WINTER 2007–08 in this issue ... 12 15 16 17 18 26 27 REGULAR FEATURES ALUMNI NEWS 1 editorial by Sir Richard Sykes 22 networks and groups 2 letters 26 Imperial’s international ambassadors 28 alumni focus NEWS 30 media mentions 3 Imperial news 31 books 4 faculty news 32 in memoriam 33 honours FEATURES 12 wrapping up our Centenary year_looking back at a year of celebrations 15 Centenary celebrations reunite alumni_at the Alumni Reunion 2007 16 dust rocks!_alumnus and Queen guitarist Brian May explains zodiacal dust 17 a rare vintage_the possibilities of Manchester Merlot and Sheffield Shiraz 18 a giant step for UK healthcare_a look at the UK’s first Academic Health Science Centre 20 Africa: health matters?_leading academics gather to discuss African healthcare 21 good advice_shaping the College’s future success in fundraising EXCLUSIVE ONLINE FEATURES new Department of Life Sciences_to encourage collaboration across the spectrum of life sciences happy 10th birthday medicine_celebrating 10 years since the Faculty’s formation schistosomiasis control initiative_awarded the Queen’s Anniversary Prize celebrating strong links with Asia_at the Asia Convocation IMPERIALmatters PRODUCED BY THE OFFICE OF ALUMNI AND DEVELOPMENT AND IMPERIAL COLLEGE COMMUNICATIONS EDITOR ZOË PERKINS MANAGING EDITOR SASKIA DANIEL EDITORIAL CONTRIBUTORS LIZ GREGSON, ABIGAIL SMITH, LAURA GALLAGHER, DANIELLE REEVES, COLIN SMITH AND NAOMI WESTON DESIGN JEFF EDEN PRINT PROLITHO LTD DISTRIBUTION PHAROS INTERNATIONAL IMPERIAL MATTERS IS PUBLISHED TWICE A YEAR. -

Grants • Arts • Volunteering • Fundraising Imperial Health Charity Newsletter Spring 2018
IMPERIAL HEALTH CHARITY NEWSLETTER SPRING 2018 GRANTS • ARTS • VOLUNTEERING • FUNDRAISING PAGES 6&7 - We did it! The More Smiles Appeal for the children’s intensive care unit at St Mary’s Hospital reaches its £2 million target INNOVATION INSPIRATION INTERVIEW Elderly care ward Resident artist Meet the eye transformed with joins the team to experts with a support from get creative with new vision for charity grant young patients patient care PAGE 2 PAGE 9 PAGE 10 CHARING CROSS • HAMMERSMITH • QUEEN CHARLOTTE’S & CHELSEA • ST MARY’S • WESTERN EYE Welcome to Focus Imperial Health Charity Chief Executive Ian Lush meets Senior Ward Sister Mojisola Hassan at the opening of the Welcome to the Spring refurbished Thistlethwayte ward at St Mary’s Hospital 2018 edition of Focus, the quarterly newsletter from Imperial Health Charity. I am delighted to announce that we have exceeded the £2 million target of our More Smiles Appeal! The money we have raised will go towards the expansion and refurbishment of the children’s intensive care unit at St Mary’s Hospital. The unit treats some of the country’s sickest children, providing a lifeline where other hospitals are simply not equipped to offer such complex care. We launched the appeal - in partnership with COSMIC charity - back in 2015 and it has taken an incredible amount of hard work and dedication to reach our ambitious target. There is not enough space here to recognise the many people who have helped us along the way. But to everyone who has made a donation or raised money - thank you. -

Issue 175 • 21 March 2007
reporter www.imperial.ac.uk Issue 175 • 21 March 2007 Supporting a healthy outcome A key step forward for UK’s first Academic Health Science Centre centre pages early years grows darling pays a call up! Secretary of State for 44 new places for Trade and Industry visits Imperial children Imperial PAGE 3 PAGE 5 Sponsor Ben Support the Student in brief Opportunities Fund One for all and all for one! Imperial as One, the College’s black and minority ethnic race equality advisory group, was estab- lished in 2005 with the aim of promoting good race relations and supporting good practice throughout London Marathon the organisation. All staff are welcome to join. If you are interested in being involved or wish to Running for Opportunity receive further details, register your interest at [email protected]. Or why not have a taste of a paradise island by going along to their Ben Ryall is Imperial College’s first ever themed ‘Splash’ party this Friday 23 March? A London Marathon runner. He will be running buffet and entertainment will be provided. Contact Sunday 22 April to raise money for the Student Opportunities Fund. The Fund Clive Mendes on 020 7585 7809 to order your enables students from all over the world to tickets. receive a scholarship to support them for the duration of their course at Imperial. Established in 2003, the Student Opportunities Fund has awarded 60 scholarships. Visit Ben’s website to keep track of his weekly blog and training diary, see photos of Ben’s training, and keep him Research grant on the up on his toes by sending him good luck messages. -

Imperial College Healthcare NHS Trust: Annual Report and Accounts 2018/19
Annual report 2018/19 Contents Welcome Welcome 3 I’m delighted to introduce the annual report for Performance report 5 Imperial College Healthcare NHS Trust for 2018/19 – the first to be published during my tenure as Overview 6 chair. I took up my new role in April 2019 and About the Trust 9 the achievements and challenges set out in these pages illustrate perfectly why I feel such pride Trust in numbers 12 and enthusiasm for the task ahead as we embrace Performance analysis corporate objectives 14 the best in patient care. Sustainability report 26 Imperial College Healthcare incorporates five hospitals and a growing portfolio of community-based and Performance against five domains of quality 28 digital services. We offer one of the broadest ranges Research discoveries 37 of acute and specialist care in the country to over one million patients a year. Working closely with partners Accountability report 39 across the healthcare system, we draw patients from Corporate governance report 40 across the UK and from around the world, as well as Paula Vennells CBE being privileged to serve those who live locally in Chair Statement of the chief executive officer’s some of north west London’s most diverse boroughs. responsibilities as the accountable officer of the Trust 45 Like the rest of the NHS and all developed healthcare systems, we are grappling with how best to respond Statement of directors’ responsibilities sustainably to growing needs. At the same time, we in respect of the accounts 45 are excited and inspired by the expanding possibilities Annual governance statement 48 of 21st century healthcare, which has the potential to improve patient care and outcomes – beyond what Care Quality Commission Regulatory Framework 50 we can imagine today. -
Supporters of the HSK Cycle Lane
Supporters of safe cycle lanes on High St Kensington ... and the list is growing! Schools and Universities St Barnabas and St Philip's CofE Primary School Ashburnham Community Primary School Thomas's Kensington London Day School Imperial College Students' Union Notting Hill Preparatory School Avondale Park Primary School Thomas Jones Primary School Kensington Primary Academy Avonmore Primary School Bevington Primary School West London Free School Kensington Park School Imperial College London St Paul’s Girls’ School The Harrodian School Fox Primary School Snowflake School Collingham College NHS and Health Providers Imperial College Healthcare NHS Trust - Charing Cross Hospital - Queen Charlotte's & Chelsea Hospital - Hammersmith Hospital - St Mary's Hospital - Western Eye Hospital Chelsea and Westminster NHS Trust Prescription for Safe Cycling Physio Motion Specs of Kensington The Pan-London NHS Bicycle User Groups (BUG) covers the following groups: Chelsea and Westminster BUG West London Trust BUG Epsom and Saint Helier BUG Imperial College Healthcare BUG Guy’s & St Thomas’ BUG East London NHS Foundation Trust BUG London North West Hospitals BUG Great Ormond Street BUG South London and the Maudsley BUG University College London Hospitals BUG Camden & Islington Trust BUG North East London Commissioning Support Unit BUG South West London & St George’s BUG St George’s University Hospitals BUG Hounslow & Richmond Community Healthcare BUG North East London Trust BUG Barts Health BUG Iconic Sustainable Institutions Transport Royal College of -

Imperial Healthcare Nhs Trust
JOB DESCRIPTION TITLE OF POST: Senior Radiographer SALARY BAND: Band 6 LOCATION: Imaging – Hammersmith Hospital RESPONSIBLE TO: Clinical Services Manager (PROFESSIONALLY) ACCOUNTABLE TO: General Manager HOURS PER WEEK: 37.5 Inspiring futures More than just a healthcare provider, Imperial College Healthcare NHS Trust is on a mission to give our patients exemplary, compassionate and safe care. We're doing this through innovations in patient care, education and research. Every day our people work hard to bring us closer to where we want to be. Join us and you’ll be part of a community that recognises your contribution – and inspires you to achieve great things. Five London hospitals make up Imperial College Healthcare NHS Trust: St Mary's Hospital, Charing Cross Hospital, Hammersmith Hospital, The Western Eye Hospital, and Queen Charlotte's & Chelsea Hospital. Some 10,000 people work together across these sites and in the community to provide the best clinical outcomes and standards of care to our patients. One of the largest Trusts in the country, we're also the UK's first academic health science centre (AHSC), bringing together the benefits of cutting-edge research with high standards of patient care. With more than 50 specialties and one of the largest portfolios of services in the country, we're a place full of opportunity as well as inspiration. Imaging We have the full spectrum of imaging modalities at Hammersmith Hospital, delivering advanced clinical practices such as Cross-sectional Cardiac Imaging in CT, Radiographer led CT Colonoscopy examinations, and highly complex Interventional Radiology including PAVM embolisations, SIRTEX treatments. -

Imperial College Healthcare NHS Trust Western Eye Hospital Ophthalmology Specialty Focused Visit
Quality and Regulation Team (London and South East) Imperial College Healthcare NHS Trust Western Eye Hospital Ophthalmology Specialty Focused Visit Quality Visit Report 23 March 2016 Final Report Visit Details Trust Imperial College Healthcare NHS Trust – Western Eye Hospital Date of visit 23 March 2016 Background to visit The Western Eye Hospital (WEH) had, historically, some seemingly intransigent issues relating to both education and service, which were having a detrimental impact on the quality of training the ophthalmology department could provide. The Specialty Focused Visit in June 2014 to the WEH found numerous issues that needed addressing, these included: the out of hours cover for casualty, consultant supervision, a lack of theatre exposure, the organisation of clinics and the lack of staffing to effectively manage the workload. There was a lack of engagement with the subsequent action plan from the visit in June 2014 and a meeting was held between the Trust and Health Education England North West London (HEE NWL) to ensure engagement and clarify measures of escalation if the issues in the action plan were not adequately addressed. This meeting in March 2015 provided stimulus to the department and there was progress made, unfortunately, the sustainability of this progress was not substantiated by the General Medical Council National Training Survey (GMC NTS) results in 2015, but instead confirmed a very poor training environment. The GMC NTS 2015 for ophthalmology at the Trust produced four pink outliers and four red outliers, which were ‘clinical supervision out of hours’, ‘workload’, ‘access to educational resources’ and ‘supportive environment’. Following the results of the GMC NTS 2015, the specialty was placed in a status of enhanced monitoring by the GMC because the department had produced red outliers in the same indicators for four consecutive years. -
Together on the Frontline of the Ght with MS
PLUGGED IN Life as a blogging professor // SPLASH : Water polo and London 2012 Voyages of particle discovery ➺ KEEPING UP WITH MASCOT RIVALRIES ➺ A grand passion for aviation THE MAGA ZINE OF IMPERIAL COLLEGE LONDON Winter 2012–13 brains trust Together on the frontline of the ght with MS WELCOME | winter 2012–13 FROM THE ➜ inside issue 38 PRESIDENT & RECTOR Sta • Editor-in-Chief: Tom Miller (Biology 1995) • Creative Director: Beth Elzer Hungry for experiences that stretch them and nourish them, • Editor-at-Large and Features Imperial students go well beyond the nerd Editor: Natasha Martineau (MSc Science Communication 1994) • News Editor: Simon Watts • Managing Editors: Pamela Our 2012–13 University Agar, Saskia Daniel Challenge team jokingly referred • Sub Editor and Distribution: to the reputation of Imperial Saskia Daniel students as nerds who can x 32 Behind the scenes • Designers: Abby Lloyd-Pack, a computer but can’t appreciate BODY OF KNOWLEDGE Beth Elzer a good novel. ey went on The virtual cadaver that’s • Contributors: Elizabeth Atkin, to thrash the competition transforming anatomy training Olivia Davenport, Caroline Davis, in their rst match – their John-Paul Jones, Simon Levey, countless winning responses to 34 Going public Kerry Noble, Emily Ross-Joannou, arts and humanities questions I PROFESS Colin Smith, Elizabeth Swi, giving them the edge. Structural biologist Stephen Katie Weeks, Sam Wong (MSc Curry on life as a blogging Science Communication 2009) I’ve watched Imperial students STUDENT EXPLORERS professor tussle on the sports pitch and Over the summer members of The magazine for Imperial’s sing enchantingly in the Royal Imperial College Caving Club 37 Travel friends, supporters and alumni, Albert Hall and am continually helped discover Slovenia’s President & 18 Feature CERN COURIER including former students of in awe of their wide-ranging longest cave system. -

CONTESTED SPACES in LONDON: EXHIBITIONARY REPRESENTATIONS of INDIA, C
University of Kentucky UKnowledge Theses and Dissertations--History History 2012 CONTESTED SPACES IN LONDON: EXHIBITIONARY REPRESENTATIONS OF INDIA, c. 1886-1951 Alayna Heinonen University of Kentucky, [email protected] Right click to open a feedback form in a new tab to let us know how this document benefits ou.y Recommended Citation Heinonen, Alayna, "CONTESTED SPACES IN LONDON: EXHIBITIONARY REPRESENTATIONS OF INDIA, c. 1886-1951" (2012). Theses and Dissertations--History. 1. https://uknowledge.uky.edu/history_etds/1 This Doctoral Dissertation is brought to you for free and open access by the History at UKnowledge. It has been accepted for inclusion in Theses and Dissertations--History by an authorized administrator of UKnowledge. For more information, please contact [email protected]. STUDENT AGREEMENT: I represent that my thesis or dissertation and abstract are my original work. Proper attribution has been given to all outside sources. I understand that I am solely responsible for obtaining any needed copyright permissions. I have obtained and attached hereto needed written permission statements(s) from the owner(s) of each third-party copyrighted matter to be included in my work, allowing electronic distribution (if such use is not permitted by the fair use doctrine). I hereby grant to The University of Kentucky and its agents the non-exclusive license to archive and make accessible my work in whole or in part in all forms of media, now or hereafter known. I agree that the document mentioned above may be made available immediately for worldwide access unless a preapproved embargo applies. I retain all other ownership rights to the copyright of my work. -
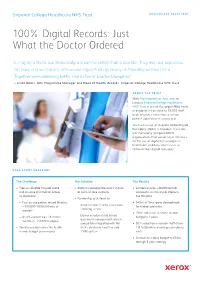
100% Digital Records: Just What the Doctor Ordered
Imperial College Healthcare NHS Trust HEALTHCARE SOLUTIONS 100% Digital Records: Just What the Doctor Ordered “It may be a cliché, but Xerox really is a partner rather than a provider. They own our objectives as theirs, and we couldn’t achieve our digital strategy nearly as smoothly without them. Together we’re delivering better care in five of London’s hospitals.” – Linda Watts, GDE Programme Manager and Head of Health Records, Imperial College Healthcare NHS Trust ABOUT THE TRUST With five hospitals on four sites in London, Imperial College Healthcare NHS Trust is one of the largest NHS trusts in England. It has close to 12,000 staff and completes more than a million patient appointments every year. The trust is one of 16 acute Global Digital Exemplars (GDEs) in England. These are internationally recognised NHS organisations that can act as a reference for the use of digital technologies in healthcare, and help other trusts to follow in their digital footsteps. CASE STUDY SNAPSHOT The Challenge The Solution The Results • Free up valuable hospital space • Ability to leverage the trust’s ‘digital • Successful pilot: ~30,000 records and improve information access at point of care’ strategy scanned in six months at Western by digitising: Eye Hospital • Partnership with Xerox to: – Four on-site patient record libraries • 547m2 of floor space claimed back – Implement an end-to-end record (~700,000-1,000,000 sets of for clinical use so far scanning service records) • >30% reduction in health records – Deliver a secure cloud-based – An off-site archive (~18 million budget in 2 years document management system, records or ~2.8 billion pages) completely integrated with the • 50% reduction in records staff (from • Simultaneously reduce the health trust’s electronic health record 113 to 56) while avoiding redundancy records budget year on year (EHR) system costs • On track to reduce budget to £0.5m through 5-year strategy HEALTHCARE SOLUTIONS THE CHALLENGE permanently hired. -
RYJ Imperial College Healthcare NHS Trust (26/02/2019)
Imperial College Healthcare NHS Trust Inspection report The Bays, South Wharf Road St Mary's Hospital London W2 1NY Date of inspection visit: 26th February to 28th Tel: 02033113311 February 2019 www.imperial.nhs.uk Date of publication: 23/07/2019 We plan our next inspections based on everything we know about services, including whether they appear to be getting better or worse. Each report explains the reason for the inspection. This report describes our judgement of the quality of care provided by this trust. We based it on a combination of what we found when we inspected and other information available to us. It included information given to us from people who use the service, the public and other organisations. This report is a summary of our inspection findings. You can find more detailed information about the service and what we found during our inspection in the related Evidence appendix. Ratings Overall rating for this trust Requires improvement ––– Are services safe? Requires improvement ––– Are services effective? Good ––– Are services caring? Good ––– Are services responsive? Requires improvement ––– Are services well-led? Good ––– Are resources used productively? Good ––– Combined quality and resource rating Good ––– 1 Imperial College Healthcare NHS Trust Inspection report 23/07/2019 Summary of findings We rated well-led (leadership) from our inspection of trust management, taking into account what we found about leadership in individual services. We rated other key questions by combining the service ratings and using our professional judgement. Background to the trust Imperial College Healthcare NHS Trust was formed on October 1, 2007 by merging St Mary's NHS Trust and Hammersmith Hospitals NHS Trust and integrating with the faculty of medicine at Imperial College London. -
Provider Section
Imperial College Healthcare NHS Trust Inspection report The Bays, South Wharf Road St Mary's Hospital London W2 1NY Tel: 02033113311 7th November www.imperial.nhs.uk 28/02/2018 We plan our next inspections based on everything we know about services, including whether they appear to be getting better or worse. Each report explains the reason for the inspection. This report describes our judgement of the quality of care provided by this trust. We based it on a combination of what we found when we inspected and other information available to us. It included information given to us from people who use the service, the public and other organisations. This report is a summary of our inspection findings. You can find more detailed information about the service and what we found during our inspection in the related Evidence appendix. Ratings Overall rating for this trust Requires improvement ––– Are services safe? Requires improvement ––– Are services effective? Good ––– Are services caring? Good ––– Are services responsive? Requires improvement ––– Are services well-led? Requires improvement ––– We rated well-led (leadership) from our inspection of trust management, taking into account what we found about leadership in individual services. We rated other key questions by combining the service ratings and using our professional judgement. 1 Imperial College Healthcare NHS Trust Inspection report 28/02/2018 Summary of findings Background to the trust Imperial College Healthcare NHS Trust was formed on October 1, 2007 by merging St Mary's NHS Trust and Hammersmith Hospitals NHS Trust and integrating with the faculty of medicine at Imperial College London.